Our bodies are mighty clever. In part, that’s because there are more than 50 hormones swirling around inside at any given time, managing everything from metabolism to mood.
If you’re trying to conceive, then one of the hormones you’ll want to pay the most attention to is luteinizing hormone (LH). This is vital for fertility, as it’s responsible for triggering ovulation (the release of an egg from your ovaries), making pregnancy possible. But if luteinizing hormone levels are too high or too low, it can disrupt the process.
Unless you have a biology degree, you might not be all that familiar with the ins and outs of LH. So what is luteinizing hormone, and how can you check that your body is making enough? We asked Dr. Jenna Flanagan, Flo medical board expert and generalist obstetrician and gynecologist, Massachusetts, US, to help give us the lowdown.
What is luteinizing hormone?
Luteinizing (pronounced loo·tuh·nai·zing, in case you were wondering) hormone plays a key role in sexual development in all of our bodies. In male reproductive systems, LH triggers the testicles to make testosterone, and in female reproductive systems, well … you can read more on that in the section below. In short, it ensures that your reproductive system is working as it should.
If we’re getting technical, luteinizing hormone is a “glycoprotein hormone” (some hormones are proteins, some are classified as steroids, and this one just happens to be a protein). It’s released by a small part of the brain called the pituitary gland, at the same time as follicle-stimulating hormone (FSH). Developing eggs live in little sacs of fluid in the ovaries called follicles, and FSH is designed to help these follicles prepare eggs for release during ovulation. The two hormones (LH and FSH) work in tandem to hopefully release a healthy, mature egg for potential fertilization (and pregnancy) each cycle.
What is the function of it?
Now that we know where it comes from, what does luteinizing hormone do? When LH is released from the pituitary gland, it kick-starts the sex organs (ovaries in women and testicles in men) into producing the hormones required for reproduction.
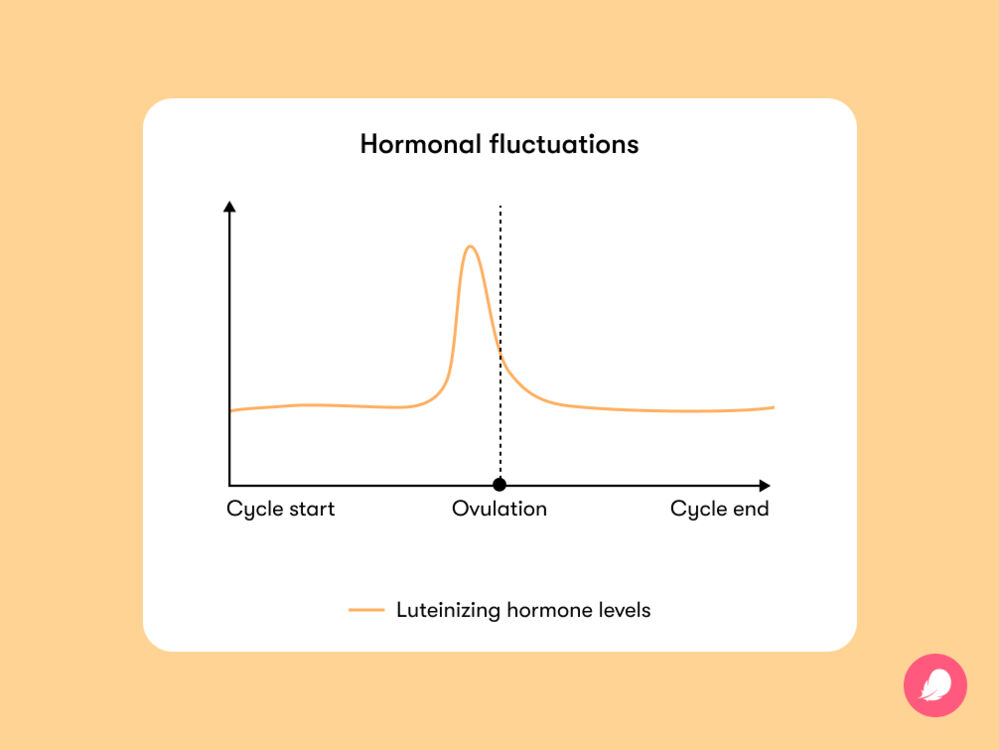
In the male reproductive system, LH is released at a regular pace to ensure a constant supply of testosterone, which is needed for sperm production. In the female reproductive system, LH surges at certain times of the month to control the menstrual cycle. “Luteinizing hormone contributes to egg maturation and ovulation. It also helps to regulate the length and order of the menstrual cycle,” explains Dr. Flanagan. Clever, huh?