Pregnancy can be an anxious time, and it’s natural to worry about miscarriage. While there are causes and risks to consider, it’s important to note that most miscarriages happen for reasons that are completely out of your control, so remember that it’s not your fault if this happens. And thankfully, for the vast majority of people affected, loss of pregnancy is usually a one-off occurrence.
Miscarriage affects around 10% to 25% of known pregnancies — but they often occur very early on, before you even realize you’re pregnant. Symptoms of pregnancy loss include vaginal bleeding or loss of fluids, tissue, or clots from the vagina. Cramping or pain in the abdomen or lower back is also a known symptom. However, remember that spotting and cramping are both also common early signs of pregnancy; while experiencing them can be unnerving, it doesn’t necessarily mean you will miscarry. Some miscarriages can occur without any symptoms, but try not to let this thought run away with you. If you’re concerned, always reach out to your doctor, and they can provide reassurance and advice.
Read on to discover more about what can cause miscarriage and, hopefully, find a little bit of reassurance during this time.
Causes of miscarriage during pregnancy
First of all, let’s get one thing clear: “There is nothing you can do to prevent or cause a miscarriage,” says Dr. Allison Rodgers, obstetrician and gynecologist, Fertility Centers of Illinois, US. However, it can be helpful to understand what can cause miscarriages and which things to try to avoid during pregnancy, as there are some lifestyle tweaks you can make to help mitigate some of the risks.
Chromosome abnormalities
Approximately 50% of all miscarriages occur because of chromosomal abnormalities — such as having too many or too few chromosomes — which can unfortunately prevent the embryo from developing properly. That might sound confusing if it’s been a while since you studied biology, so let’s break it down a bit. Chromosomes from the sperm and the egg carry the genes an embryo needs to develop into a baby — half from each of the two biological parents. Problems with those chromosomes usually happen by chance during the complex process of cell division (the very first stages of pregnancy), and this can unfortunately lead to a miscarriage a little later down the line.
Physical problems
“Other causes for losses are physical problems,” Dr. Rodgers explains. But what exactly are physical problems? Essentially, there may be problems with the placenta (the organ that grows alongside the baby to provide it with oxygen and nutrients), the uterus (sometimes known as the womb, where the fetus grows), or the cervix (the donut-shaped organ between the uterus and the vagina) — such as an abnormally shaped uterus — or problems with the sperm.
Miscarriage risk factors
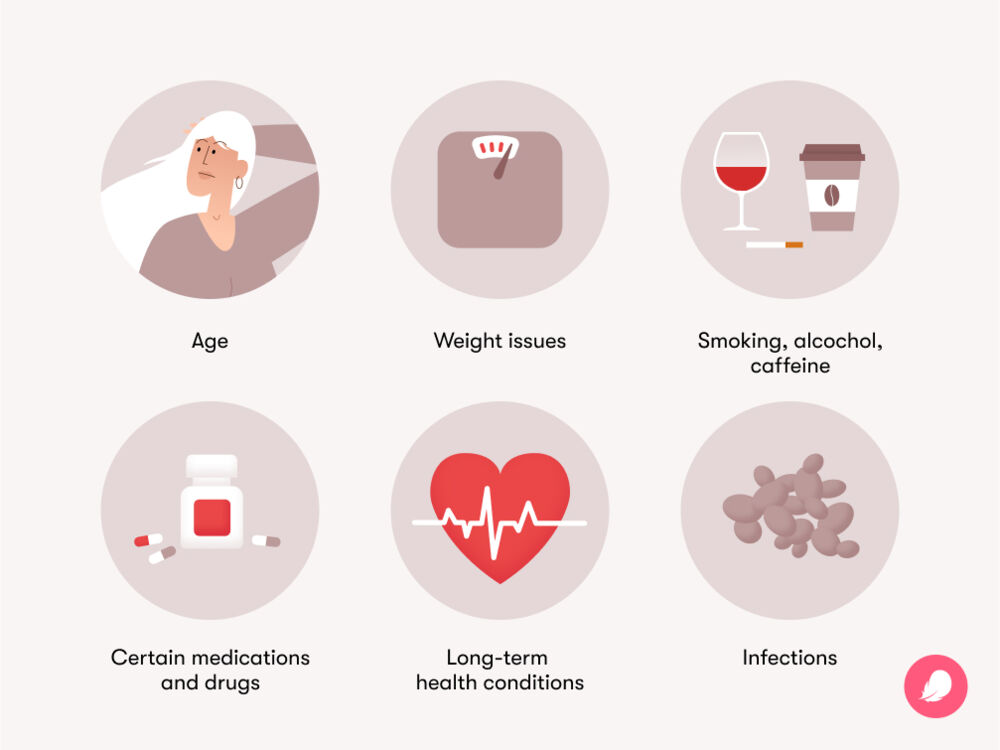
Frustratingly, it isn’t always possible to identify the cause, or causes, of miscarriage. However, we do know there are factors that can unfortunately put you at a slightly increased risk of experiencing a miscarriage.
Age
One risk factor for a miscarriage is advanced maternal age. “The risk increases as we get older, so, by the time we are 40, our chances of miscarriage are 40%,” Dr. Rodgers explains. The risk of miscarriage also increases as the father gets older, although this has less impact than the age of the mother.
These statistics might sound frightening, but they certainly don’t mean that people over the age of 40 can’t have positive pregnancy outcomes. Recent data shows that birth rates in the US have declined for nearly all age groups of women under 35 but have actually risen for women in their late 30s and early 40s. So if you’re older and you’re trying to conceive, you have every reason to keep hope.
Long-term health conditions
Unfortunately, some chronic diseases and long-term health issues can also increase the risk of miscarriage.
These include:
- Diabetes that is not well controlled: If you live with either Type 1 or Type 2 diabetes, getting your blood glucose levels under control before pregnancy can be a good way to mitigate this risk. If you have any concerns or questions about your treatment or medication, seek medical advice (ideally before you start trying to conceive).
- Some autoimmune diseases
- Hormonal conditions like thyroid disease or polycystic ovary syndrome (PCOS): People with PCOS are three times as likely to miscarry as those without, but there is hope on the horizon; researchers are currently studying whether taking metformin (a diabetes medication) could reduce this risk.
- High blood pressure (also referred to as hypertension)
- Kidney disease
Remember that although they can increase the risk, living with any of these conditions does not mean that you will have a miscarriage — far from it. If you have any concerns, speak to your health care provider for advice on managing your condition and your overall well-being during pregnancy.
Infections
We’re always encountering viruses and bacteria in our normal lives, so it’s difficult to avoid infections completely. However, some infections could also affect your baby and, in some rare scenarios, may potentially lead to a miscarriage. But it’s important to remember that many of these infections can be easily treated or managed — or, in the case of listeriosis and toxoplasmosis, avoided by not eating high-risk foods, such as raw or undercooked meat and eggs and unpasteurized cheeses.
When it comes to infections, some risk factors include:
- Rubella
- Herpes simplex virus
- Toxoplasmosis
- Chickenpox
- HIV
- Syphilis
- Parvovirus B19
- Cytomegalovirus
If you’re concerned about any of these or other infections or want more information, it’s best to speak to your doctor, who will be happy to help.
Weight issues
Being over or underweight (that means having a Body Mass Index (BMI) below 20 or over 25) may increase your risk of a miscarriage, while being obese (having a BMI over 30) can further increase that risk. If you’re concerned about your weight, speak to your health care provider for advice on healthy eating and exercise during pregnancy.
Smoking
There is evidence that smoking is associated with an increased risk of miscarriage, as well as other adverse pregnancy outcomes. There isn’t currently enough research to determine whether vaping poses a similar risk, but experts recommend avoiding e-cigarettes during pregnancy. Although overcoming a nicotine addiction can be understandably difficult, support is available if you want to quit smoking for your own health and that of your growing baby; try the Centers for Disease Control and Prevention if you’re in the US or the NHS if you’re in the UK.
Alcohol
Experts agree that there is no “safe” amount of alcohol that can be drunk during pregnancy, while research suggests that alcohol consumption can increase the risk of miscarriage. That risk was not related to the number of drinks per week, beverage type, or binge drinking, meaning that alcohol may sadly be linked to a miscarriage even at low levels of consumption. If you’re looking for some ideas of non-alcoholic drinks that are safe to consume during pregnancy, you can read our article on the best drinks to have during pregnancy.