If you’re considering starting a family in your late 30s or thinking about a second pregnancy after 35 — now or someday in the future — you may have some questions.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Pregnancy after 35: What an OB-GYN wants you to know


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Will it happen? What are the risks of pregnancy after 35? And what do doctors think about (prepare for a stomach-turning phrase) “geriatric” pregnancies, aka pregnancies after 35?
We’ve put your most-asked questions to Dr. Charlsie Celestine, an obstetrician and gynecologist (OB-GYN) in New Jersey, US, who had a child after the age of 35.
Remember: If this is what you decide to do, you won’t be alone. According to a 2022 analysis of Census Bureau and National Center for Health Statistics data, fertility rates (how many children a woman has) of US women ages 20 to 24 declined by 43% over a roughly 30-year period. Fertility rates of women ages 35 to 39 increased by 67%. So generally, people are waiting longer before having children.
Dr. Celestine says, “A lot of my patients are in their early to late 30s, having their first or second baby, and I do have some patients in their early 40s too.”
As a quick note, if you’ve already had one or more children, the guidance here might not be the same for you. Double check with your OB-GYN — for some people, fertility can increase or decrease after a first pregnancy.
“Does my age affect my chances of getting pregnant?”
Age and fertility are closely intertwined. Dr. Celestine explains, “As we get older, our egg quality and quantity declines. This is part of the natural aging process.”
“Our eggs are usually best between 20 and 30. Their quality dips after 35 and then again more significantly at 40 and beyond. This means it’s likely to take more time to get pregnant as we get older, and we may need extra support to do so.”
This doesn’t mean you have to rush out and get pregnant if you’re not ready yet. But it’s good to know the facts so you can consider them when making your reproductive choices.
“If I conceive after 35, will I be called a geriatric mom?”
OK, it’s time to clear this up. “Historically, we used to call pregnancies where the mother was over 35 years old ‘geriatric pregnancies.’ Now, thankfully, we refer to this as advanced maternal age or AMA,” explains Dr. Celestine.
It’s still not how we’d introduce ourselves at a party, but it’s a definite improvement.
“This is just a label to help us with coding people and their pregnancies, so when we look at your records, we know that we should watch you a little bit more closely to make sure everything’s OK.
“It’s not nice to be lumped into a category of people, but there’s no judgment attached to it. And it’s definitely not that you’re elderly or ‘geriatric.’”
Take a quiz
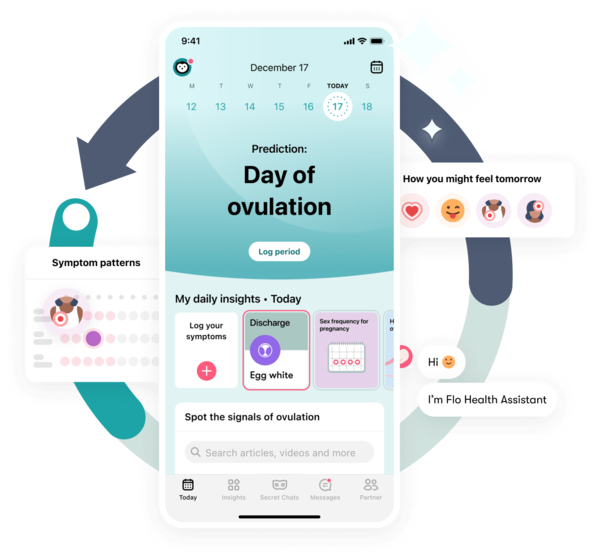
Find out what you can do with our Health Assistant
“Does my male partner’s age make a difference?”
It makes some difference. But as Dr. Celestine explains, “It’s not a huge difference compared to the impact of age on eggs.”
Men’s fertility also declines with age because their sperm quality decreases as they get older. Like women, they’re also more likely to have certain medical issues that can impact fertility, such as diabetes.
“There are some genetic conditions (such as achondroplasia, the most common form of dwarfism, and Marfan syndrome, a connective tissue disorder) that have risks associated with the dad being older. However, these risks are not as common as those linked to the mom’s age.
“Depending on your partner’s age, if you get pregnant, you may want to ask about some additional screening to keep an eye on your baby as your pregnancy progresses.” This might consist of extra blood tests or ultrasounds.
"I think having a baby over 35 can be a fantastic thing. You’ve experienced more in life, so there are fewer worries about missing out, and you’re more likely to feel ready to settle down."
“Should I have fertility testing?”
If you haven’t started trying to get pregnant yet and you’re interested in fertility testing (perhaps out of curiosity or you want to be particularly well-informed ahead of time), then it’s best to speak to your health care provider about your options.
Generally speaking, fertility testing (which can include checking your hormone levels with a blood test and your ovaries and uterus with an ultrasound, or for a male partner, a semen analysis) isn’t recommended before trying to conceive. But it might make sense in certain situations — for example, if you have a medical condition or your partner has trouble ejaculating.
Once you start trying to conceive, though, there are clear guidelines about when to seek testing:
- If you’re under 35, the general recommendation is to try to have sex every two to three days throughout your cycle, especially around ovulation. (Tracking your cycle with Flo can help with this.) If you haven’t gotten pregnant after one year of trying, it’s time for some additional tests.
- If you’re over 35, the recommendation is to try for six months before you go for fertility testing. It's best to get help sooner rather than later if you need it.
- Finally, if you’re over 40, fertility testing is recommended as soon as you decide you want to get pregnant.
“Can my lifestyle affect fertility more after 35?”
Yes. Because egg quality is likely to already be lower after 35, healthy habits are even more important.
Dr. Celestine says, “To be honest, it’s the same lifestyle factors that pretty much every doctor is going to preach about.” For example, if you smoke, prioritize quitting. “Smoking is hazardous to so many aspects of your health, including fertility.”
What else can help you prep for pregnancy?
“You should also get any medical issues under control, including obesity," explains Dr. Celestine. “Obesity can wreak havoc on your hormones.” Obesity and difficulty conceiving are strongly linked with the risk of infertility being three times higher for obese women than nonobese women. It’s likely that this is due, at least in part, to insulin resistance.
Insulin is a hormone that helps lower your blood sugar levels, regulating how it travels from the blood into cells where it’s used for energy. Typically, blood sugar remains relatively stable. But if you’re experiencing insulin resistance, your body isn’t carrying out this process properly, leaving too much sugar in your bloodstream. Your body then produces even more insulin in an attempt to lower your sugar levels. Having excess sugar and insulin in your body can lead to weight gain.
Insulin resistance can also cause hormonal imbalance, and this, in turn, can disrupt menstruation and ovulation (making it harder to get pregnant). “So maintaining a healthy weight by eating a balanced diet and exercising regularly is really important when it comes to trying to get pregnant, no matter if you’re under or over 35,” Dr. Celestine adds.
Getting pregnant while obese also carries additional risks, with higher rates of complications like gestational diabetes and preeclampsia.
Another lifestyle change you may need to make: Cut back on drinking, as high levels of alcohol in your system will diminish egg quality. That said, it’s not necessary to go completely dry as long as you’re truly drinking in moderation. Studies show that having one or two servings of alcohol daily (or less than 14 servings per week) had no noticeable impact on fertility.

That said, the American College of Obstetricians and Gynecologists recommends that you stop drinking if you’re actively trying to conceive in case you get pregnant without realizing right away. It’s also important to completely stop drinking alcohol if you do find out that you’re pregnant.
“And the final one, which I love talking about, is decreasing stress. It truly affects everything to do with your health. Obviously, if trying to conceive starts taking a long time, that can cause stress itself. It’s a vicious cycle, I know.
“Some people find exercising to be helpful. I’m not one to meditate or do yoga, but some people also find that really works for them. And some people even find acupuncture great for decreasing stress. Personally, I like massages. They’re great. But do anything that helps you personally decrease your stress levels.”
“Is it inevitable that I’ll need in vitro fertilization (IVF) or other fertility treatment because of my age?”
On this, Dr. Celestine is clear. “No, it’s definitely not inevitable.”
Instead, she says it’s something that depends on your individual case. “There are many reasons why somebody might need IVF or other fertility treatment. But I do see many people in their mid to late 30s, and some even in their early 40s, getting pregnant naturally. If you’re healthy overall, and try not to wait until you’re 40 or later if possible, then you still have a good chance.”
So, who’s actually having fertility treatments? In 2020, medical professionals in the United States carried out a whopping 326,468 ART cycles (assisted reproductive technology cycles — this is the medical term for fertility treatment and includes procedures like IVF or ovarian stimulation).
Most of these cycles (37.2%) involved people under the age of 35. The next largest number (23.3%) involved those aged 35 to 37, 20% were aged 38 to 40, 9.4% were aged 41 to 42, and 10.1% were older than 42.
The average age of patients using ART was 36.2. Even the mention of fertility treatment can be worrying for some, but Dr. Celestine suggests trying to flip the way you think about it. “If you do end up needing fertility treatment like IVF, then isn’t it great that it exists? It’s still a fairly recent option and has helped so many people achieve their reproductive goals.”
To give you an idea of average success rates, in 2021, the Society for Assisted Reproductive Technology reported the following percentage of live births per egg retrieval (when you extract an egg as part of IVF or egg freezing):
- For those under the age of 35, 44.5%
- Ages 35 to 37, 32.4%
- Ages 38 to 40, 20.2%
- Ages 41 to 42, 9.6%
- Over the age of 42, 2.9%
“What pregnancy complications are more common after 35?”
Dr. Celestine explains, “I’m going to be frank here — most pregnancy complications are more common after 35. This includes an increased chance of diabetes in pregnancy (also known as gestational diabetes) and blood pressure conditions such as gestational hypertension (when you develop high blood pressure that goes away after giving birth) and preeclampsia (a similar condition with the addition of protein in your urine and other symptoms). There’s also an increased chance of miscarriage and preterm delivery (when you give birth early).
“However, I definitely don’t want you to think this will affect everybody. I had my baby over 35, and I was fine — I didn’t develop any of those complications. And all of this is why we watch you more closely during pregnancy if you’re of an advanced maternal age. This might mean more monitoring and more frequent visits to keep you and your baby safe.”
"It's definitely not inevitable you'll need fertility treatment"
“Are there any benefits to getting pregnant after 35?”
Absolutely! “I think having a baby over 35 can be a fantastic thing,” reassures Dr. Celestine. “You’ve experienced more in life, so there are fewer worries about missing out, and you’re more likely to feel ready to settle down.”
“You’re also more likely to have a more established career, a place to live, and, if you’re in a relationship, that could be more established than in your 20s too. All the risks and other things I’ve mentioned are just to be aware of. It’s not all doom and gloom, I promise.”


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Having a Baby after Age 35: How Aging Affects Fertility and Pregnancy.” The American College of Obstetricians and Gynecologists, Feb. 2023, www.acog.org/womens-health/faqs/having-a-baby-after-age-35-how-aging-affects-fertility-and-pregnancy.
Harris, Isiah D., et al. “Fertility and the Aging Male.” Reviews in Urology, vol. 13, no. 4, 2011, pp. 184–90, www.ncbi.nlm.nih.gov/pmc/articles/PMC3253726.
“Male Infertility.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/17201-male-infertility. Accessed 23 Nov. 2023.
Lenzi, T. A., and T. R. B. Johnson. “Screening, Prenatal.” Encyclopedia of Infant and Early Childhood Development, Elsevier, 2008, pp. 78–90, www.sciencedirect.com/topics/medicine-and-dentistry/paternal-age.
“Should My Partner and I Seek Testing for Infertility?” Planned Parenthood, www.plannedparenthood.org/learn/pregnancy/infertility/should-my-partner-and-i-get-tested-infertility. Accessed 23 Nov. 2023.
“Treating Infertility.” The American College of Obstetricians and Gynecologists, Aug. 2022, www.acog.org/womens-health/faqs/treating-infertility.
“Not Pregnant Yet? When to Seek Help.” Cleveland Clinic, 11 June 2019, health.clevelandclinic.org/not-pregnant-yet-when-to-seek-help.
“Preconception Counseling.” Cleveland Clinic, my.clevelandclinic.org/health/articles/4503-preconception-counseling. Accessed 23 Nov. 2023.
“Non-Invasive Prenatal Testing (NIPT).” NHS Inform, 25 Oct. 2023, www.nhsinform.scot/healthy-living/screening/pregnancy/non-invasive-prenatal-testing-nipt.
“Prenatal Genetic Testing.” Cleveland Clinic, my.clevelandclinic.org/health/diagnostics/24136-pregnancy-genetic-testing. Accessed 23 Nov. 2023.
“2020 National ART Summary.” Centers for Disease Control and Prevention, www.cdc.gov/art/reports/2020/summary.html. Accessed 23 Nov. 2023.
“Preliminary National Summary Report for 2021.” Society for Assisted Reproductive Technology Clinic Outcome Reporting System, sartcorsonline.com/CSR/PublicSnapshotReport?ClinicPKID=0&reportingYear=2021. Accessed 23 Nov. 2023.
Silvestris, Erica, et al. “Obesity as Disruptor of the Female Fertility.” Reproductive Biology and Endocrinology, vol. 16, no. 1, Mar. 2018, www.ncbi.nlm.nih.gov/pmc/articles/PMC5845358.
“Causes: Polycystic Ovary Syndrome.” NHS, www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/causes/. Accessed 24 July 2023.
Kahn, B. B., and J. S. Flier. “Obesity and Insulin Resistance.” The Journal of Clinical Investigation, vol. 106, no. 4, Aug. 2000, pp. 473–81, www.ncbi.nlm.nih.gov/pmc/articles/PMC380258.
Mikkelsen, Ellen M., et al. “Alcohol Consumption and Fecundability: Prospective Danish Cohort Study.” BMJ, vol. 354, Aug. 2016, www.bmj.com/content/354/bmj.i4262.long.
Alcohol and Pregnancy. The American College of Obstetricians and Gynecologists, Feb. 2023, www.acog.org/-/media/project/acog/acogorg/womens-health/files/infographics/alcohol-and-pregnancy.pdf.
Morse, Anne, “Fertility Rates: Declined for Younger Women, Increased for Older Women.” United States Census Bureau, 6 Apr. 2022, www.census.gov/library/stories/2022/04/fertility-rates-declined-for-younger-women-increased-for-older-women.html?utm_campaign=20220406msacos1ccstors&utm_medium=email&utm_source=govdelivery.
History of updates
Current version (07 December 2023)
Published (07 December 2023)
In this article
Get your personal guide to fertility
-
Learn how to read your body's ovulation signals
-
Find daily conception tips from our experts
-
Chat with others who are trying to get pregnant




