Your egg count decreases over time, but when does it become an issue for fertility? Find out how many eggs a woman is likely to have at different life stages and what this means for getting pregnant with advice from a Flo expert.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
How many eggs does a woman have?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
When it comes to understanding your fertility, your egg count is a key factor. But exactly what goes on in your ovaries can feel like a bit of a mystery.
You may know that you release one egg each month (aka ovulation), but are you developing a new egg each time or losing an old one? And what happens to all the others in your reserve?
Find out how many eggs a woman has in her lifetime, what happens to these eggs as we age, and, most importantly, what you need to know to increase your chances of conceiving.
For reference, we know it’s not just women who have eggs, periods, and babies. But for the purposes of this article, we’ll use the term “women” because that’s what most people search for.
Key takeaways
- A woman is born with all the eggs she’ll ever have — approximately 1 to 2 million of them. Her egg count gradually decreases with age, but the decline gets faster during her 30s.
- By age 45, a woman’s fertility will have reduced so much that getting pregnant naturally will be unlikely. However, many people are now having babies later, in their late 30s and even 40s. So, while it’s important to be aware that your fertility will decline naturally with age, for many people, getting pregnant later in life is still possible. It may just require the support of fertility treatment to help it happen.
- Your chances of conceiving each month are not just related to your egg count but also the quality of your eggs.
Take a quiz
Find out what you can do with our Health Assistant
What do we mean by eggs?
An egg is a type of sex cell. When an egg meets the other type of sex cell — a sperm — it can become fertilized. Eventually, if all goes well, this fertilized egg will develop into a baby.
How many eggs is a woman born with?
Women’s bodies are mind blowing. A baby girl develops up to 6 to 7 million eggs while she’s still in her mother’s womb. That means when you’re pregnant with a girl, you’re not only carrying your daughter but the eggs that could one day become your grandchildren!
The number of eggs a baby has in her teeny ovaries represents her fixed lifetime supply — she cannot produce any more. This number starts decreasing before birth, but she’ll still be born with a bumper supply of around 1 to 2 million. This number drops again before puberty to around 300,000 to 500,000 eggs.
How many eggs are released during ovulation?
A woman’s gradual fall in egg count is largely caused by what happens during the menstrual cycle. “One egg is released in each cycle,” says Dr. Allison K. Rodgers, reproductive endocrinologist, infertility specialist, obstetrician, and gynecologist, Fertility Centers of Illinois, US. But before that, a whole bunch of eggs — known as a “cohort” — start growing due to your hormone levels changing, explains Dr. Rodgers.
In every cycle, one egg will grow faster than the others. This will be the one you release during ovulation. “That one egg suppresses the rest in the cohort from growing,” says Dr. Rodgers. “In rare situations, two eggs are released [also known as hyper ovulation], which is how some twins form.”
As the dominant egg grows and is released, the rest in the group will dissolve and be absorbed back into your body. The number of eggs that start growing each cycle is unique to you, but women tend to lose around 1,000 eggs with each ovulation cycle.
“There is not a significant drop in egg count per cycle, but over time, egg count decreases as each cohort in each cycle is lost,” says Dr. Rodgers.
If you’re trying to get pregnant and unsure of when you’re likely to ovulate, a cycle-tracking app like Flo can help you figure it out.
How many eggs a woman has (according to age)
As we’ve seen, the number of eggs a woman has starts decreasing while she’s still in the womb. “Age is the most important factor when it comes to egg count,” says Dr. Rodgers. “As time goes on, we lose both egg quantity and quality.”
The older we get, the more eggs we lose with each passing cycle. But as well as that, the number of eggs that are strong enough to go on to make a baby also drops.”
That said, if you're considering trying for a baby after 30 then there's positives, too. Let's take a closer look at egg count per decade.
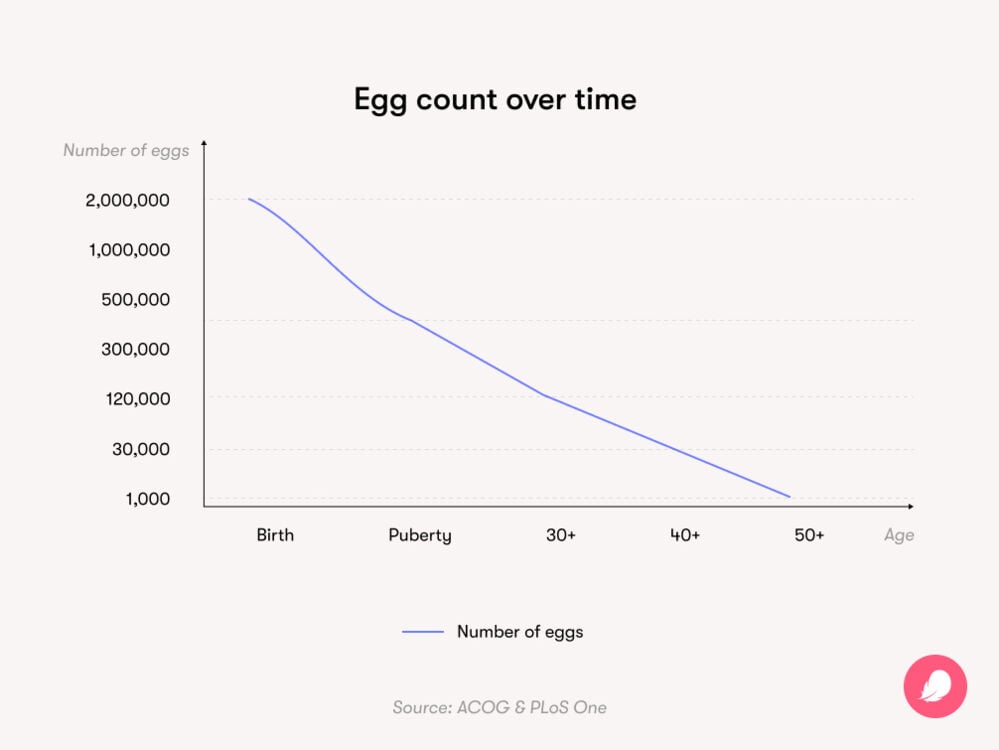
Age 30+
Your 30s are when the decline in your egg count starts to speed up, but the idea that your fertility nosedives at age 35 is a myth. In reality, it’s more of a gentle slope than a sheer drop. Here are the numbers: At age 30, a woman has around 12% of the number of eggs she was born with — so around 120,000 eggs if she was born with 1 million. The downward slope becomes steeper around age 32 and then drops more rapidly again after age 37.
Age 40+
By age 40, a woman will have around 3% of the number of eggs she was born with — or around 30,000 eggs if she was born with 1 million. By age 45, a woman is unlikely to be able to get pregnant naturally. There is a small chance (2.9%) that in vitro fertilization (IVF) using her own eggs may work at the age of 45. However, she may want to consider using donor eggs to boost her chances of getting pregnant via IVF at this age.
Age 50+
By the time she reaches 50, a woman has around 1,000 eggs left on average.
There’s no denying that age impacts fertility. The older we get, the fewer healthy eggs we have, which is why conceiving naturally can get harder or take longer as you age.
But it’s important to keep things in perspective. Many women have healthy babies in their late 30s and 40s. In fact, in the United States, the number of women having their first baby (both with or without the help of fertility treatment) over the age of 35 is rising. Between 2020 and 2021, there was a 5% increase in women having their first child aged 35 to 39 and a 4% rise in women aged 40 to 44. So, if you’re hoping to have children a little later on, don’t lose hope.
There are plenty of reasons why people are having children later in life. Some women are choosing to focus on their careers and education for longer. For others, baby making in early adulthood simply isn’t possible in today’s tough economic climate — it can be expensive to have a child, after all. Dating culture has changed too, with people often having multiple relationships before they settle down. And for some, finding a partner to have children with isn’t as easy as they’d hoped it might be. The bottom line is that it’s not always possible to plan your life according to your “body clock” — yep, we’re not big fans of that saying either.
If you’re currently trying, speak to your doctor if you haven’t gotten pregnant after a year. Schedule an appointment after six months if you’re over 35 or as soon as possible if you’re aged 40 or above. They’ll be able to help you get a fertility checkup in case you need any help conceiving.
What other factors can impact your egg count?
Age might be important, but it’s not the only factor that determines your egg count. We all work in different ways.
“While more women lose the ability for their eggs to make a baby between [the ages of] 42 and 44, some women will have the ability to produce a baby later than that, and some will lose it before,” says Dr. Rodgers. “We are each individuals, and just like we didn’t all get our first menstrual periods at the same time, our ovarian reserve drops individually too.”
Menopause
When a woman runs out of eggs completely, she reaches what’s known as menopause. This is officially diagnosed when you’ve gone 12 months without a period and marks the end of your reproductive years.
Often, the first signs of menopause are longer or shorter menstrual cycles, spotting between periods, or changes in vaginal bleeding. You may also notice some of the classic menopause symptoms, like hot flashes or night sweats. This is known as perimenopause or the years leading up to menopause.
While most women reach menopause around age 51, it can happen earlier for some people. So, what are the chances of this happening to you? Well, reassuringly, menopause before the age of 40 (which is considered to be “premature” in medical terms) isn’t that common: 1% of women experience this.
While sometimes there is no clear cause, there are some factors that can make you more likely to have menopause prematurely that are good to be aware of.
Genetics
The timing of menopause can be genetic, so the age when people in your family stopped having periods can be a good indicator of when it’ll happen to you. Certain genetic conditions can also lead to early fertility loss. “There are several known mutations, but the most common is fragile X [syndrome],” says Dr. Rodgers. “This is a gene mutation that causes you to lose your eggs quicker. Other genetic problems such as Turner’s Syndrome (where you are missing an X chromosome) cause premature menopause.”
Autoimmune diseases can also run in families and are one of the most common causes of a reduced egg count, according to Dr. Rodgers. These include conditions like rheumatoid arthritis, Crohn’s disease, or thyroid disease.
If you’re worried your family history might increase your chance of going into menopause prematurely, try not to panic. Speak to your health care provider to work out a plan to get a clearer picture of what’s going on. “Get checked out and talk with a [doctor] about your long-term family goals and if you have enough eggs to get you there,” says Dr. Rodgers.
Your doctor may talk to you about the ways you can preserve your fertility. For example, you may want to consider egg freezing or embryo freezing (when you freeze eggs that have already been fertilized by sperm).
Smoking
“Women who smoke tend to go into menopause earlier,” says Dr. Rodgers. In fact, smoking is the only lifestyle factor that has a confirmed link to reducing egg count.
However, it’s worth knowing that other lifestyle factors — like drinking more than two alcoholic drinks a day or four a week — may have an impact on your chances of conceiving. Though the findings across different studies are inconsistent, women who are already seeking treatment for infertility should be mindful of minimizing alcohol intake, as even moderate levels could make it harder to conceive.
Cancer treatments and surgeries
“Some medications, such as radiation or chemotherapy for cancer, can destroy a person’s healthy eggs,” says Dr. Rodgers. “It depends on what medications are used and how much.” Having surgery on your ovaries or having one or more of your ovaries removed can also lead to a lower egg count.
If this applies to you, remember that there are ways you can preserve your fertility. If it has not already come up in conversations with your doctor, bring it up in your next appointment.
Should you be worried about your egg count?
“I wouldn’t say worried; I would say ‘in touch with,’” says Dr. Rodgers. If you are worried about your egg count, the best thing to do is get in touch with your doctor and discuss your future plans to have a family. They can explain what is best for your situation.
There are some simple tests and checks that can be done either at home or in a clinic to get a better idea of your ovarian reserve (how many eggs you have left). Testing can include:
- Checking the levels of anti-Mullerian hormone (AMH) in your blood. AMH is produced by your follicles, so higher levels show that you have a large supply of eggs.
- Testing your levels of follicle-stimulating hormone (FSH) — the hormone that prepares eggs for ovulation.
- Having your doctor count the number of follicles you have in your ovaries via a transvaginal ultrasound.
Before you rush to your doctor and request every ovarian reserve test available or buy an at-home testing kit, there are a few things that are important to know.
While some of these tests are marketed as such, there’s not much scientific evidence in favor of using them as fertility tests if you don’t have known fertility issues. In other words, if you’re just curious about your future fertility or you’re considering egg freezing, don’t bank on ovarian reserve tests to give you a reliable prediction. There are so many other factors involved in your chances of getting pregnant in the future, and your age will probably give you a better idea of this.
How many eggs does a woman have? The takeaway
Incredibly, we are born with all the eggs we’ll ever have — and that’s a lot, somewhere between 2 to 3 million eggs. On average, women do have fewer eggs available for fertilization after the age of 35 — and the number of eggs declines year on year from this point until you reach menopause. But as we have learned, that doesn’t always mean your chances of getting pregnant are lower, as it’s the quality of the eggs that are generally more important than the quantity. And if you do happen to struggle with conceiving at any age, there are plenty of options available, from IVF to surrogacy and donor eggs/embryos.
If you’re unsure where you stand with your egg count and want to get a better picture, then have a conversation with a medical professional or your OB-GYN. That’s the best way of empowering yourself to make the choices that are right for your reproductive health.
However, there are times when AMH or FSH testing might be advised. “If you have any red flags — such as irregular cycles, hot flashes, night sweats — you should [consider getting] your ovarian reserve checked,” advises Dr. Rodgers. Your health care provider may also suggest you have ovarian reserve testing if you have a diagnosed medical condition known to impact egg count (for example, some cancers), you’re starting IVF, or you’re planning egg freezing. In that case, it could help to guide your fertility experts on how much medication you might need to stimulate your ovaries to produce eggs for the treatment.
If, for any reason, you have had ovarian reserve testing and you’re concerned about your results, know this: If you don’t have fertility issues, then having a low egg count doesn’t generally influence your chances of conceiving each month. The odds of conceiving with a single egg are more about the quality of that egg. “Egg count and quality are different,” says Dr. Rodgers. “Age tends to tell us about quality, but quantity can be a little more variable.” Unfortunately, we still don’t have a way to test the quality of a woman’s eggs.
If you’re worried about age, fertility, and egg count, then chat with your doctor. They can walk you through egg freezing and discuss whether that might be an option for you. By allowing you to save some of your higher quality eggs for later, egg or embryo freezing can help you preserve your fertility, although it’s important to remember it doesn’t come with any guarantees. “Having a family is important to do when it’s right for you,” says Dr. Rodgers. “However, biologically, your eggs are only good for so long, so technology like egg or embryo freezing [can be a] successful way to stop that clock.”
Of course, the cost of egg freezing means it’s not an option for everyone, and you may find you don’t need to use the eggs in the end anyway. But, for some women, the peace of mind it can bring alone makes it worth the investment — everyone is different. The best thing you can do is be aware of the fertility facts. And remember, you can talk to your doctor about any concerns you might have before trying to conceive.
More FAQs
How many eggs does a woman produce each month?
A woman doesn’t produce eggs each month — she’s born with all the eggs she’ll ever have. But once she starts having periods, her ovaries will develop and release one of those eggs each month during ovulation.
How do you check egg count?
Each egg you have lives inside a fluid-filled sac in your ovaries called a follicle, so doctors can check egg count by estimating the number of follicles you have.
As follicles produce a hormone called AMH, checking the levels of this hormone in your blood can help build a picture of how many eggs you have. Alternatively, doctors can count the number of follicles you have via a transvaginal ultrasound.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Broekmans, F. J., et al. “A Systematic Review of Tests Predicting Ovarian Reserve and IVF Outcome.” Human Reproduction Update, vol. 12, no. 6, Nov./Dec. 2006, pp. 685–718, https://doi.org/10.1093/humupd/dml034.
Carson, Sandra Ann, and Amanda N. Kallen. “Diagnosis and Management of Infertility: A Review.” JAMA, vol. 326, no. 1, 6 July 2021, pp. 65–76, doi: 10.1001/jama.2021.4788.
Cox, Emily, and Veronica Takov. “Embryology, Ovarian Follicle Development.” StatPearls, StatPearls Publishing, 14 Aug. 2023, www.ncbi.nlm.nih.gov/books/NBK532300.
“Diminished Ovarian Reserve.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/23975-diminished-ovarian-reserve. Accessed 4 June 2024.
“Egg, Embryo Freezing Are Options for Women Who Want to Delay Pregnancy.” UCLA Health, 21 Jan. 2022, www.uclahealth.org/news/article/egg-embryo-freezing-are-options-for-women-who-want-to-delay-pregnancy.
Erickson, Gregory. “Follicle Growth and Development.” The Global Library of Women’s Medicine, 2008, www.glowm.com/section-view/heading/Follicle%20Growth%20and%20Development/item/288.
“Evaluating Infertility.” The American College of Obstetricians and Gynecologists, Jan. 2020, www.acog.org/womens-health/faqs/evaluating-infertility.
“Female Age-Related Fertility Decline.Committee Opinion No. 589. American College of Obstetricians and Gynecologists.” Obstetrics and Gynecology, vol. 123, no. 589, Mar. 2014, pp. 719–21, www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2014/03/female-age-related-fertility-decline.
“Follicle-Stimulating Hormone (FSH) Levels Test.” MedlinePlus, 4 Dec. 2023, medlineplus.gov/lab-tests/follicle-stimulating-hormone-fsh-levels-test/.
Gunnala, Vinay, et al. “One Thousand Seventy-Eight Autologous IVF Cycles in Women 45 Years and Older: The Largest Single-Center Cohort to Date.” Journal of Assisted Reproduction and Genetics, vol. 35, no. 3, Mar. 2018, pp. 435–40, doi: 10.1007/s10815-017-1088-y.
“Having a Baby after Age 35: How Aging Affects Fertility and Pregnancy.” The American College of Obstetricians and Gynecologists, Feb. 2023, www.acog.org/womens-health/faqs/having-a-baby-after-age-35-how-aging-affects-fertility-and-pregnancy.
Intranet, Rogel. “Normal Ovarian Function.” Rogel Cancer Center, University of Michigan Health, www.rogelcancercenter.org/fertility-preservation/for-female-patients/normal-ovarian-function.
MacMillan, Carrie. “Women, How Good Are Your Eggs?” Yale Medicine, 2 Aug. 2018, www.yalemedicine.org/news/fertility-test.
“Menopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/menopause/symptoms-causes/syc-20353397.
“Menstrual Cycle.” Cleveland Clinic, my.clevelandclinic.org/health/articles/10132-menstrual-cycle. Accessed 4 June 2024.
Mesen, Tolga B., et al. “Optimal Timing for Elective Egg Freezing.” Fertility and Sterility, vol. 103, no. 6, June 2015, pp. 1551–56.e1–4, https://doi.org/10.1016/j.fertnstert.2015.03.002.
Osterman, Michelle J. K., et al. “Births: Final Data for 2021.” National Vital Statistics Reports, vol. 72, no. 1, 31 Jan. 2023, pp. 1–53, www.cdc.gov/nchs/data/nvsr/nvsr72/nvsr72-01.pdf.
“Ovarian Reserve Testing.” Cleveland Clinic, my.clevelandclinic.org/health/diagnostics/25142-ovarian-reserve-testing. Accessed 4 June 2024.
“Ovarian Reserve Tests Fail to Predict Fertility, NIH-Funded Study Suggests.” National Institutes of Health, 10 Oct. 2017, www.nih.gov/news-events/news-releases/ovarian-reserve-tests-fail-predict-fertility-nih-funded-study-suggests.
Owen, Amy, et al. “Age-Related Fertility Decline.” StatPearls, StatPearls Publishing, 2 Feb. 2024, www.ncbi.nlm.nih.gov/books/NBK576440.
Practice Committee of the American Society for Reproductive Medicine. “Testing and Interpreting Measures of Ovarian Reserve: A Committee Opinion (2020).” Fertility and Sterility, vol. 114, no. 6, Dec. 2020, pp. 1151–57, www.asrm.org/practice-guidance/practice-committee-documents/testing-and-interpreting-measures-of-ovarian-reserve-a-committee-opinion-2020/.
“Premature and Early Menopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21138-premature-and-early-menopause. Accessed 4 June 2024.
“The Menstrual Cycle.” UCSF Health, www.ucsfhealth.org/education/the-menstrual-cycle. Accessed 4 June 2024.
“The Use of Antimüllerian Hormone in Women Not Seeking Fertility Care. ACOG Committee Opinion No. 773. American College of Obstetricians and Gynecologists.” Obstetrics and Gynecology, vol. 133, no. 773, 2019, p. e274–8, www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2019/04/the-use-of-antimullerian-hormone-in-women-not-seeking-fertility-care.
Van Heertum, Kristin, and Brooke Rossi. “Alcohol and Fertility: How Much Is Too Much?” Fertility Research and Practice, vol. 3, 10 July 2017, p. 10, doi:10.1186/s40738-017-0037-x.
Wallace, W. Hamish B., and Thomas W. Kelsey. “Human Ovarian Reserve from Conception to the Menopause.” PLoS One, vol. 5, no. 1, 27 Jan. 2010, https://doi.org/10.1371/journal.pone.0008772.
Witt, Barry. “Trying to Get Pregnant? Here’s When to Have Sex.” The American College of Obstetricians and Gynecologists, Aug. 2023, www.acog.org/womens-health/experts-and-stories/the-latest/trying-to-get-pregnant-heres-when-to-have-sex.




