Cervical cancer is a major public health issue worldwide, causing the deaths of over 300,000 women in 2018. Read on to learn about causes of cervical cancer and cervical cancer risk factors and prevention.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Cervical Cancer Risk Factors: What You Need to Know

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
What is cervical cancer?
Cervical cancer is a disease that causes cancer cells to develop in the cervix, which is the part of the body that links the uterus and vagina. Human papillomavirus, or HPV, is the leading cause of cervical cancer.
Cervical cancer tends to develop slowly over a long time, so it can be detected early through a combination of HPV testing and Pap screening, which collects and examines cervical cells. Thanks to the HPV vaccine and Pap smears, cervical cancer is the most preventable type of cancer.
When diagnosed early and treated promptly, cervical cancer can be cured. The first signs of cervical cancer are precancerous lesions on top of the cervix, which can be removed by a doctor in a nearly painless procedure. If the cancer is more developed, different treatment methods are available, such as radiation, chemotherapy, or targeted therapy and surgery.
Cervical cancer risk factors
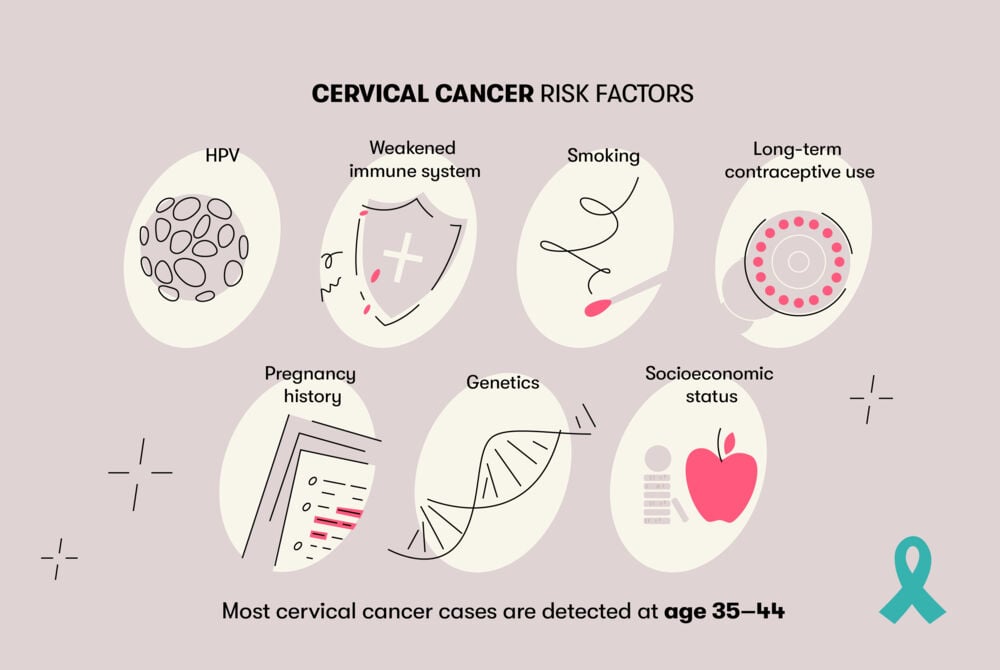
- STIs
HPV is an extremely common sexually transmitted infection, mainly passed through skin-to-skin genital contact or sharing sex toys. Out of over 100 types of HPV, 14 can cause cervical cancer.
Co-infections such as herpes, chlamydia, gonorrhea, and HIV are risk factors for cervical cancer. HIV weakens the immune system, and chlamydia may help HPV grow on the cervix. An estimated five percent of cervical cancer cases are attributed to HIV.
Having multiple sexual partners increases the chances of contracting an STI. Becoming sexually active at a young age, having many partners, and having sex with someone who has HPV also increases the risk of cervical cancer.
- Weakened immune system
Cervical cancer can develop much quicker in people with weakened immune systems. The immune system is responsible for destroying and slowing the growth of cancerous cells. A weakened immune system may be caused by an untreated HIV infection, autoimmune disease, or organ transplant.
- Smoking
Tobacco smoke contains at least 70 cancer-causing chemicals that enter the bloodstream and damage DNA, leading the body to produce unusual cells that can develop into cancer. People who smoke are twice as likely as non-smokers to be affected by cervical cancer. Smoking also makes it more difficult for the immune system to fight an HPV infection.
Long-term hormonal contraceptive use
Research shows that using hormonal contraceptives for a long time — five years or more — carries an increased risk for cervical cancer, but the risk decreases again after stopping contraceptives and eventually returns to normal.
- Pregnancy history
Becoming pregnant before the age of 20, giving birth to three or more children, and having children less than two years apart increases the risk for cervical cancer. Hormonal changes and a weaker immune system during pregnancy may also make it difficult to fight off an HPV infection and stop cancer growth.
- Genetics
The probability of developing cervical cancer is 2–3 times higher if a blood relative has had it than if no one in the family has been affected.
- Socioeconomic status
Worldwide, many low-income people don’t have access to proper health care, so they can’t receive regular Pap screenings and HPV vaccines, which increases their cervical cancer risk.
Cervical cancer prevention
There are several ways to prevent cervical cancer.
- Vaccination
It’s estimated that the HPV vaccine can prevent 90 percent of cervical cancer cases. Vaccination should be done before becoming sexually active because the vaccine can only prevent HPV infection. It doesn’t stop an existing infection. - Regular screening
The HPV test screens for HPV infection, and Pap smears detect changes in the cervix that could develop into cancer. These tests can be done at the same time by your gynecologist. The recommendations on when and how often these tests should be done vary widely internationally, so make sure to consult your health care provider for details. - Healthy lifestyle
Using condoms during sex, eating a diet full of fruits and vegetables, and not smoking (or quitting) can also help prevent cervical cancer.
Summing Up
There are certain risk factors that increase the chance of getting cervical cancer. Raising awareness of these factors and improving access to HPV vaccines and regular Pap screenings will prevent most cervical cancer cases and greatly improve female health on a global scale.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.

