Practicing safe sex can have lots of beneficial outcomes for your health. Riskier sexual activities can increase a person’s exposure to sexually transmitted infections (STIs), which spread through vaginal, anal, and oral sex. One STI in particular, called human papillomavirus (HPV), can lead to cancer or genital warts.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
How to Prevent Human Papillomavirus: Four Key Ways

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
In this article, we’ll explore how to prevent human papillomavirus transmission and infection and which methods offer the strongest protection.
Who is at risk of HPV?
Young adults and adolescents aged 15 to 25 have the highest rates of HPV, studies say. In fact, about 75 percent of all HPV infections likely occur within this age range.
Certain risk factors influence a person’s likelihood of developing HPV. These include:
- Type of HPV
- Immune status
- Concurrent infection of another STI with HPV
- Giving birth at a young age
- Smoking
All of these factors can increase a person’s risk of contracting HPV. Before we dive into HPV prevention methods, let’s unpack why they matter.
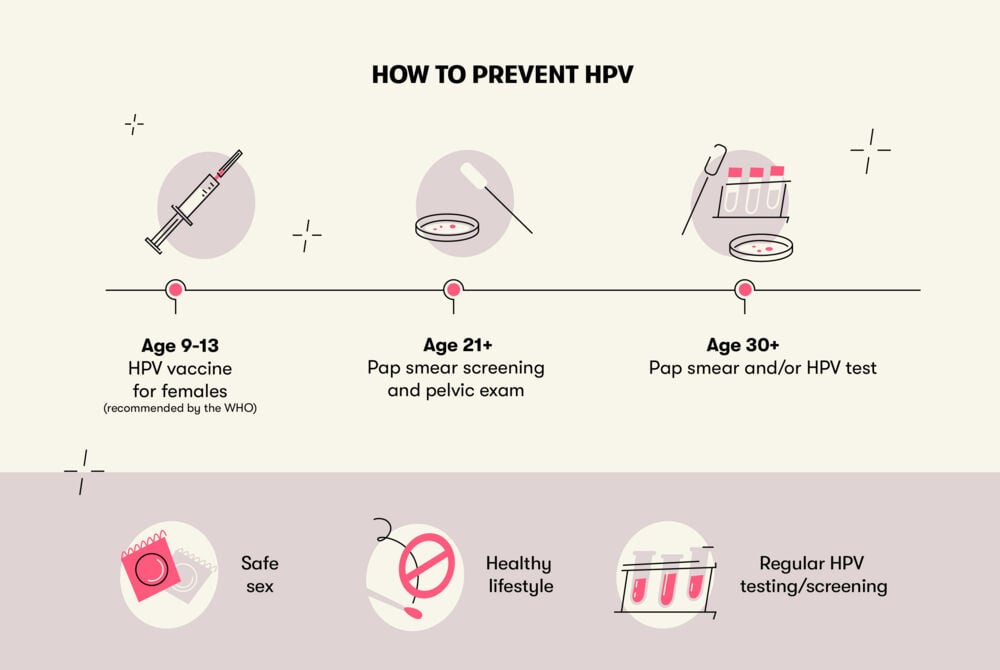
How to prevent HPV
Human papillomavirus prevention and practicing safe sex with HPV matter because an infection can lead to genital warts and cervical cancer. According to the World Health Organization (WHO), two types of HPV cause 70 percent of pre-cancer lesions and cervical cancer. This is significant because cervical cancer accounts for about 7.5 percent of all female cancer deaths.
HPV can also lead to other types of cancer. There are over 100 types of HPV, and about 14 of these can increase the risk of developing other cancers, including vulva, vagina, anus, penis, and throat cancer.
Let’s look at the most effective forms of human papillomavirus prevention.
Take a quiz
Find out what you can do with our Health Assistant
Practice safe sex with HPV
Do condoms protect against HPV? Yes — in fact, safe sex is a key type of HPV prevention.
For people who are sexually active, having HPV can create feelings of anxiety or embarrassment. It’s normal to feel this way, but HPV is very common. No matter your health history, it’s important to communicate honestly with your sexual partner and vice versa.
Practicing safe sex with HPV can protect you and/or your partner from contracting the virus. However, this approach isn’t foolproof: HPV can be spread through skin-to-skin contact, so some risk remains. The female body usually clears HPV within two years, and heterosexual cisgender men rarely develop major health issues from HPV. Wearing a condom can reduce the risk of transmitting HPV. In addition, limiting your sexual partners can also reduce your risk of contracting HPV.
READ MORE: What does HPV look like?
Maintain a healthy lifestyle
If you’re wondering how to prevent getting HPV, you should know that a healthy lifestyle offers extra protection.
Strengthening your immune system by looking after your general health may help protect against HPV. By giving your body adequate nutrients and fuel, you’re also boosting your immune system’s ability to keep you strong.
If you smoke, consider cutting down or quitting, especially if you’re concerned about HPV. Research shows that cigarette smoking increases the risk of cervical cancer among people with HPV compared to non-smokers.
Get regular testing
In the U.S., the Centers for Disease Control and Prevention (CDC) recommends starting Pap smear screening not earlier than age 21 and continuing screening every three years. After you turn 30, you can do HPV testing every five years in addition to regular Pap screening, since these two tests go hand-in-hand. Alternatively, you can opt for HPV testing alone every five years.
According to the WHO, HPV vaccination for female children should start at age 9–13, before they’re sexually active. And female adults 30 and older need to be screened for abnormal cervical cells.
Unfortunately, there is currently no routine or approved HPV screening for men. However, men who have genital warts are often diagnosed with HPV, since this is the most common sign of HPV infection in men.
Ask about the HPV vaccine
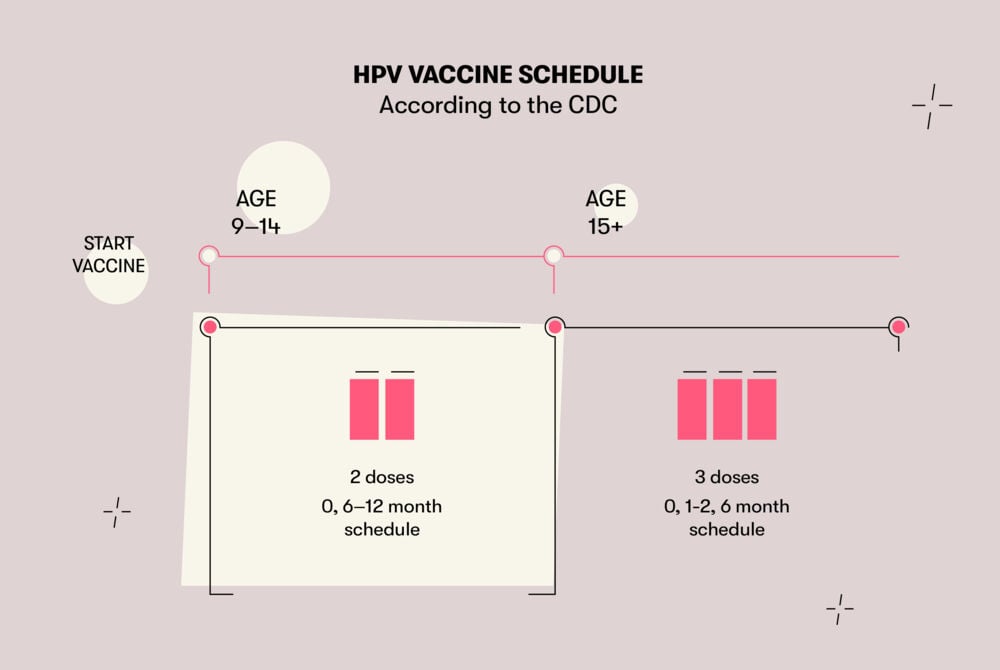
The CDC recommends the Gardasil vaccine for everyone ages 11–12, while the WHO recommends vaccination of female children from age 9–13
For people who get their first dose at ages 9–13, a two-dose HPV vaccine schedule is recommended. The second dose should be given 6-12 months after the first one.
If a person gets their first dose of HPV vaccine at age 15 and over, a three-dose schedule is recommended. The second dose should be given 1–2 months after the first dose, and the third dose needs to be given six months after the first.
Is the HPV vaccine safe? In the United States, Gardasil has been approved by the FDA. HPV vaccination risks are minor and include pain, redness, stinging, bruising, bleeding, nausea, headaches, fever, diarrhea, and abdominal pain. In very rare cases, people develop Gardasil side effects years later, such as chronic fatigue syndrome, premature ovarian failure, complex regional pain syndrome, and Guillain-Barre syndrome.
As with all immunizations, there are HPV vaccine pros and cons. Thankfully, evidence indicates that Gardasil is almost 100 percent effective at preventing cervical, vaginal, and vulvar cancers.
Takeaway
Most health organizations recommend the HPV vaccine. To protect against other STIs and illnesses, using condoms and maintaining a healthy lifestyle are also highly recommended. In fact, taking steps to prevent human papillomavirus infection can help you lead a healthier life.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.




