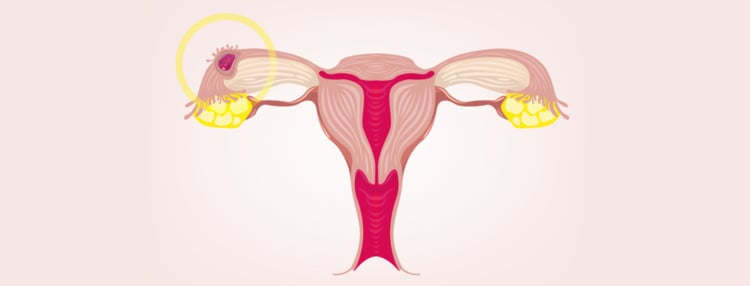
In an ectopic pregnancy, the embryo develops outside the uterus. This condition is not common and affects about two percent of pregnancies. People who use reproductive technologies have a slightly higher rate of five percent.
Let’s find out more about the early signs of ectopic pregnancy. In fact, a timely diagnosis may save your ability to get pregnant again.