LH is a key hormone when you’re trying to conceive. So what do you need to know? A Flo expert breaks it down.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Luteinizing hormone (LH): What is it and how does it affect the menstrual cycle?

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Our bodies are mighty clever. In part, that’s because there are more than 50 hormones swirling around inside at any given time, managing everything from metabolism to mood.
If you’re trying to conceive, then one of the hormones you’ll want to pay the most attention to is luteinizing hormone (LH). This is vital for fertility, as it’s responsible for triggering ovulation (the release of an egg from your ovaries), making pregnancy possible. But if luteinizing hormone levels are too high or too low, it can disrupt the process.
Unless you have a biology degree, you might not be all that familiar with the ins and outs of LH. So what is luteinizing hormone, and how can you check that your body is making enough? We asked Dr. Jenna Flanagan, Flo medical board expert and generalist obstetrician and gynecologist, Massachusetts, US, to help give us the lowdown.
What is luteinizing hormone?
Luteinizing (pronounced loo·tuh·nai·zing, in case you were wondering) hormone plays a key role in sexual development in all of our bodies. In male reproductive systems, LH triggers the testicles to make testosterone, and in female reproductive systems, well … you can read more on that in the section below. In short, it ensures that your reproductive system is working as it should.
If we’re getting technical, luteinizing hormone is a “glycoprotein hormone” (some hormones are proteins, some are classified as steroids, and this one just happens to be a protein). It’s released by a small part of the brain called the pituitary gland, at the same time as follicle-stimulating hormone (FSH). Developing eggs live in little sacs of fluid in the ovaries called follicles, and FSH is designed to help these follicles prepare eggs for release during ovulation. The two hormones (LH and FSH) work in tandem to hopefully release a healthy, mature egg for potential fertilization (and pregnancy) each cycle.
What is the function of it?
Now that we know where it comes from, what does luteinizing hormone do? When LH is released from the pituitary gland, it kick-starts the sex organs (ovaries in women and testicles in men) into producing the hormones required for reproduction.
In the male reproductive system, LH is released at a regular pace to ensure a constant supply of testosterone, which is needed for sperm production. In the female reproductive system, LH surges at certain times of the month to control the menstrual cycle. “Luteinizing hormone contributes to egg maturation and ovulation. It also helps to regulate the length and order of the menstrual cycle,” explains Dr. Flanagan. Clever, huh?
How do luteinizing hormone levels change throughout the cycle?
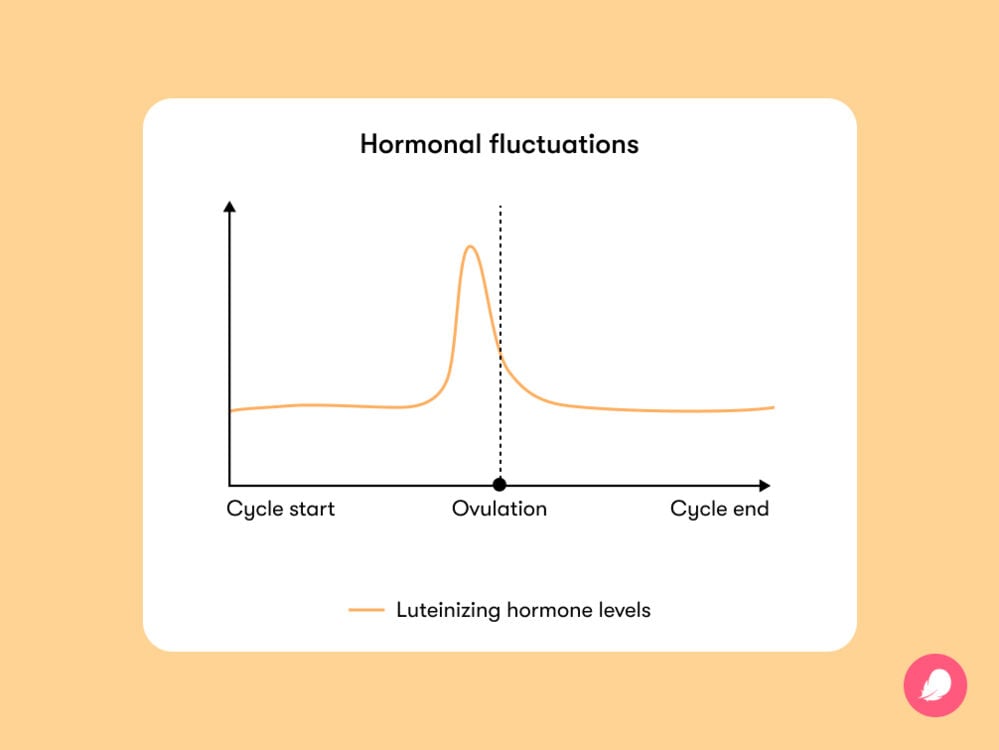
In women and people who have periods, luteinizing hormone levels fluctuate during the menstrual cycle. They rise sharply just before you ovulate and drop once the egg has been released.
During a luteinizing hormone surge, your body might give you a few signs that ovulation is just around the corner. For example, you may notice that your cervical mucus changes consistency, turning clear and slippery. Cervical mucus is released with your vaginal discharge, so you might spot this change in your underwear. This is totally normal; it makes it easier for the sperm to swim to meet the egg and signals the best time to have sex to conceive.
Ovulation also causes an increase in basal body temperature (BBT), which some people track as part of natural family planning. However, this rise in temperature isn’t directly caused by LH (it’s progesterone, which also rises around ovulation, that you can thank for that). Doctors don’t normally recommend tracking your BBT, as it’s generally more useful for telling you that you ovulated after the fact, which makes it a bit impractical for preventing pregnancy. But if you do want to monitor your daily temperature for conception purposes, you need to do this consistently over several weeks to spot a slight rise. It’s worth bearing in mind, however, that other factors can affect your temperature, including illness, stress, alcohol, certain medications, and interrupted sleep cycles, so this method isn’t foolproof. If you’d rather steer clear of getting pregnant, it’s usually recommended to consider a more effective method of contraception.
When and why does LH surge?
Because our bodies know what they’re doing when it comes to procreation, the surge of LH sends a signal to the ovary to release an egg. When luteinizing hormone levels are at their peak, roughly midway through your cycle, this is the time you’re most likely to get pregnant.
“LH typically surges 24 to 48 hours prior to ovulation, and in a 28- to 30-day cycle, that’s typically midcycle, or around day 14 to 16 of the cycle,” says Dr. Flanagan. Of course, not everyone has a cycle that length. A 2020 study in Australia using Flo’s period tracker found that only 16% of women have a 28-day cycle, so you could try using our online ovulation calculator to get a better idea of when ovulation is likely to happen for you depending on your cycle patterns.
Another common way of predicting when ovulation will strike is by monitoring your luteinizing hormone surge with a home ovulation test. This involves dipping a test stick into a sterile container of urine or peeing straight onto the stick, just like a pregnancy test. A positive test means that ovulation is imminent, and you’re at the most fertile point of your cycle, so you should get straight to the bedroom if you want to have a chance of conceiving.
“Typically, the test is performed daily approaching midcycle, then twice daily around the predicted time of a surge,” advises Dr. Flanagan. Explaining why, she adds, “The LH surge can last 12 to 24 hours; therefore, testing twice a day should be done so that the LH surge isn’t missed during testing.”
Take a quiz
Find out what you can do with our Health Assistant
Is it possible to increase luteinizing hormone? And why might you want to?
Considering how important LH is for conception, you might be wondering if you should try to increase your luteinizing hormone levels. You may question this particularly if regular ovulation testing suggests your levels may be low. Realistically, there’s not all that much you can do to increase your LH levels because they’re controlled naturally. But remember that you may not be seeing an LH surge on your ovulation tests because it’s simply not the right time in your cycle — not because your levels are too low altogether.
It’s also important to keep in mind that all home ovulation tests have some degree of unreliability. Instead, you may find that tracking your cycles using an app like Flo (72% of women say Flo helps them spot the signs of ovulation*) and monitoring changes in your cervical mucus work better for you.
Around 85% of people will conceive within the first year of trying, which is why it’s recommended you wait 12 months before reaching out to a doctor (if you’re under the age of 35, have a regular menstrual cycle, and don’t have any obvious health problems). However, you should consider scheduling an appointment sooner if either partner has a risk factor for infertility or if you’re older than 35. Wait for around six months before seeking help if you’re between 35 and 40, and it’s advisable to consult a specialist right away if you’re over 40.
Regardless of your age and your LH levels, it’s always important to eat a healthy, balanced diet if you’re preparing to get pregnant and to make sure you are getting extra folic acid. So make sure you’re getting all the proteins, carbohydrates, fats, vitamins, and minerals that you need.
Are LH levels high during pregnancy?
Although LH levels spike just before ovulation, these high levels aren’t maintained during pregnancy. In fact, studies show that levels of luteinizing hormone are undetectable during pregnancy. And it makes sense, really. If the main job of LH is to trigger ovulation and to help regulate the menstrual cycle, and neither of these things happen while you’re pregnant, there’s no need for LH to be floating about during this time.
What is a luteinizing hormone serum test, and should you have one?
If you’ve searched online for info about LH before, you might have heard of a luteinizing hormone serum test. So what actually is it? Don’t confuse the serum test with the at-home ovulation kits you can buy from the drugstore when trying to conceive — they’re quite different.
A measurement of LH is sometimes checked as a blood test when doctors are trying to investigate a menstrual cycle abnormality. Usually, if an LH blood test is done, LH will be checked along with many other hormones to try to figure out why someone might be having irregular periods or not ovulating regularly. LH levels that are high during a time other than the midcycle surge might suggest polycystic ovary syndrome (PCOS), decreased ovarian reserve, or menopause.
At the other end of the scale, a blood test might find that LH doesn’t peak during your cycle. Because you need a certain amount of LH for reproduction to work, ovulation can also be disrupted in this scenario. “When someone is not ovulating regularly, they will not have an LH surge. This doesn’t mean that LH is the problem, however. Problems with ovulation can be caused by many things, including stress, medications, and other hormonal imbalances,” explains Dr. Flanagan.
Whatever the result, your health care provider will be able to talk you through what it means for your health and your future fertility. There will likely be various treatments you can try if you’d like to get pregnant, and a health care professional will be able to talk you through the options. Don’t hesitate to ask lots of questions to make sure you understand as best you can.
Luteinizing hormone (LH): The takeaway
If you’ve read all this, you probably now feel like you’re a pro on the topic of LH. And you might find the information particularly useful if you’re trying to conceive. At-home ovulation kits are a great way of pinpointing when your LH levels are surging, indicating the best time to try for a baby. However, by using an app like Flo, getting to know your body, and looking for the most obvious sign of ovulation (stickier cervical mucus that’s like raw egg whites in texture), you may find you don’t need to pee on sticks. You can save that for when you think you’re pregnant!
If you’ve been trying to conceive for 12 months or more without success, or if your periods are irregular or have gone missing altogether, don’t be afraid to ask your doctor for advice. That way, you can check if there are any underlying issues you should know about.
*Based on a 2022 survey of 3,750 Flo users


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Basal Body Temperature for Natural Family Planning.” Mayo Clinic, 3 Mar. 2021, www.mayoclinic.org/tests-procedures/basal-body-temperature/about/pac-20393026.
“Cervical Mucus.” Cleveland Clinic, my.clevelandclinic.org/health/body/21957-cervical-mucus. Accessed 8 Feb. 2023.
“Characteristics of Hormones.” National Cancer Institute, training.seer.cancer.gov/anatomy/endocrine/hormones.html. Accessed 30 Jan. 2023.
Follicle Stimulating Hormone (FSH): Paediatrics. NHS Manchester University, Nov. 2019, mft.nhs.uk/app/uploads/2020/01/Follicle-Stimulating-Hormone-FSH-Paediatrics.pdf.
“FSH Levels: Follicle-Stimulating Hormone Function in Fertility and Menopause.” Flo Health, 5 Nov. 2020, flo.health/menstrual-cycle/menopause/changes/follicule-stimulation-hormone-fsh-level.
“Gonadotropin-Releasing Hormone (GnRH).” Cleveland Clinic, my.clevelandclinic.org/health/body/22525-gonadotropin-releasing-hormone. Accessed 8 Feb. 2023.
Grieger, Jessica A., and Robert J. Norman. “Menstrual Cycle Length and Patterns in a Global Cohort of Women Using a Mobile Phone App: Retrospective Cohort Study.” Journal of Medical Internet Research, vol. 22, no. 6, June 2020.
“Hormones.” Cleveland Clinic, my.clevelandclinic.org/health/articles/22464-hormones. Accessed 8 Feb. 2023.
Leiva, Rene Antonio, et al. “Urinary Luteinizing Hormone Tests: Which Concentration Threshold Best Predicts Ovulation?” Frontiers in Public Health, vol. 5, Nov. 2017, p. 320, www.ncbi.nlm.nih.gov/pmc/articles/PMC5712333/.
“Luteinizing Hormone.” Cleveland Clinic, my.clevelandclinic.org/health/body/22255-luteinizing-hormone. Accessed 30 Jan. 2023.
“Luteinizing Hormone (LH) Levels Test.” MedlinePlus, 7 Dec. 2020, medlineplus.gov/lab-tests/luteinizing-hormone-lh-levels-test/.
Nassar, George N., and Stephen W. Leslie. “Physiology, Testosterone.” StatPearls, StatPearls Publishing, 4 Jan. 2022, www.ncbi.nlm.nih.gov/books/NBK526128/.
“Ovulation Home Test.” MedlinePlus, medlineplus.gov/ency/article/007062.htm. Accessed 8 Feb. 2023.
“Session 24: Ovulation and Fecundity.” Human Reproduction, vol. 25, suppl. 1, June 2010, pp. i37–38.
Soma-Pillay, Priya, et al. “Physiological Changes in Pregnancy.” Cardiovascular Journal of Africa, vol. 27, no. 2, pp. 89–94, doi: 10.5830/CVJA-2016-021.
Su, Hsiu-Wei, et al. “Detection of Ovulation: A Review of Currently Available Methods.” Bioengineering & Translational Medicine, vol. 2, no. 3, Sep. 2017, pp. 238–46.




