Cervical cancer affects hundreds of thousands of women globally each year. When detected early enough, it can be prevented and cured. Keep reading to learn all about this condition, including its causes, possible symptoms, types, and prevention at different stages of life.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Cervical Cancer Prevention: The Best Tips Gathered by Flo


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
What is cervical cancer?
Cervical cancer is a disease that occurs when cancerous cells grow in the cervix, which is the part of the body that connects the uterus and the vagina. It is a major public health issue and the fourth most common form of cancer in women.
The World Health Organization (WHO) reports that in 2018, an estimated 570,000 women worldwide were diagnosed with cervical cancer, and about 311,000 women passed away from it. Women ages 35–44 are most often diagnosed with cervical cancer, and those under the age of 20 rarely develop this disease.
There are four stages of cervical cancer, which are diagnosed based on the size of the cancer and where it has spread throughout the body. And different types of cervical cancers and precancers are classified based on how they appear under a microscope.
Technical, medical, and policy tools and approaches to eliminate cervical cancer exist. The WHO states that a comprehensive global approach to prevent, screen, and treat cervical cancer could completely eradicate it as a public health issue within just one generation.
What causes cervical cancer?
Ninety-nine percent of cervical cancer cases are connected to an infection with a high-risk strain of HPV, human papillomavirus. HPV is an extremely common sexually transmitted virus. The WHO says that most sexually active people will be infected at some point in their lives, and some may be infected repeatedly.
What are the symptoms of cervical cancer?
Pre-cancer usually does not have symptoms, and cervical cancer might not have symptoms in the early stages.
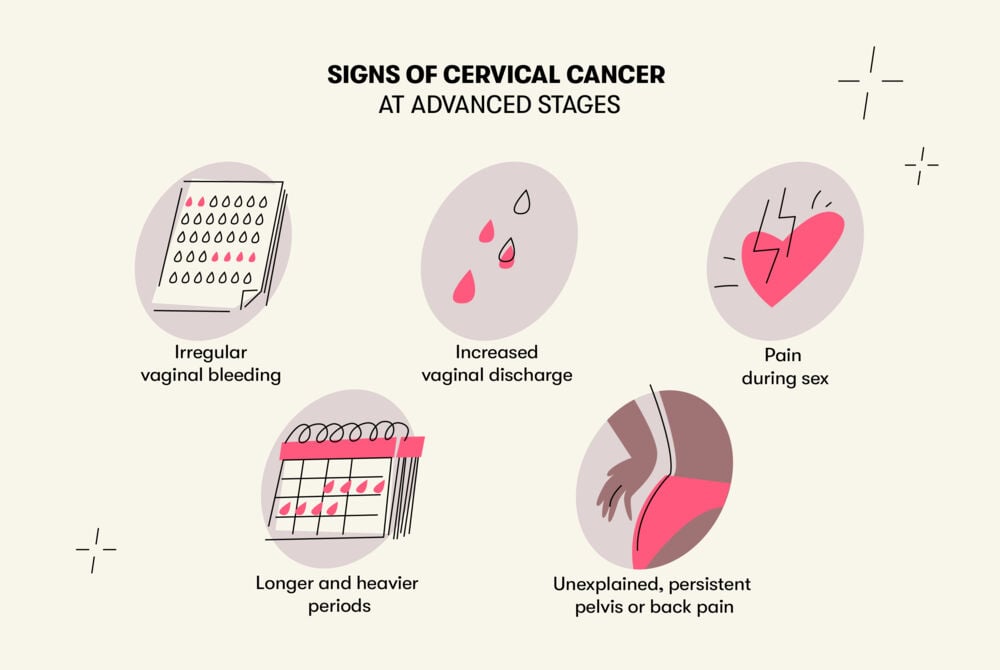
Any of the following could be signs of cervical cancer as it advances:
- Pain during sex
- Irregular vaginal bleeding
- Increased vaginal discharge
- A longer and heavier menstrual period
- Unexplained, persistent pain in the pelvis or back
If cancer reaches a more advanced stage and spreads to other parts of the body, symptoms could become more severe.
These signs can also be caused by something else, but it’s important to visit a health care provider if you notice any symptoms that don’t go away.
The risk of cervical cancer increases with age. Although cervical cancer is most often diagnosed in people who are 35–44, people 20 and older can also be affected. And it’s rarer for people younger than 20.
How to prevent cervical cancer?
The HPV vaccine and regular screening tests help prevent cervical cancer.
Here’s a guide for keeping yourself safe from cervical cancer throughout life:
- Ages 9–13: Get the HPV vaccine, which is administered in two shots. The vaccine works only before a person gets HPV. According to the WHO, girls are prioritized for HPV vaccination, because it’s the most effective way to prevent cervical cancer. The CDC recommends it for everyone.
- Ages 21–30: Get a Pap smear every three years. If the Pap smear shows abnormal cells, your doctor may recommend more regular screenings or further testing.
- Ages 31–64: Get a Pap smear every three years or a combined Pap and HPV test every five years.
To help protect yourself from cervical cancer, practice safe sex by using a condom and dental dams.
Screening tests look for pre-cancer or early stage cervical cancer, which is more treatable and has the best chance of recovery. When cervical cancer is found early enough, it is associated with long survival and better quality of life.
In the U.S., cervical cancer was once the leading cause of cancer death among women, but cases and deaths have decreased significantly over the past few decades thanks to increased screening.
Takeaway
Cervical cancer is mostly caused by HPV. It develops in the cervix and can spread throughout the body. Early-stage cancer may not have symptoms, which is why it’s essential to get vaccinated against HPV and get regular gynecological screenings. If cervical cancer is found early, the chance of recovery is high.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.

