Human papillomavirus (HPV) is the most common sexually transmitted infection (STI), with the highest rate in Africa, Eastern Europe, and Latin America. HPV can be passed from one person to another through vaginal, anal, or oral sex or skin-to-skin sexual contact. Anyone who’s exposed to HPV during sex can be infected, but is it possible for someone to pass it to their unborn child? This article explains the potential risks associated with HPV and fertility, conception, and pregnancy.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Human Papillomavirus and Pregnancy: Can HPV be passed from mother to child?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
What are the risks of pregnancy with HPV?
The majority of people infected previously with HPV have no more difficulties with pregnancy than other people. If you have ever had genital condyloma (genital warts), tell your OB-GYN. If you currently have genital warts, they can be removed before labor to prevent bleeding during delivery.
Some studies have shown that there’s a greater risk of miscarriage and preterm delivery in people diagnosed with HPV who have had significant cervical tissue removed to prevent cervical cancer from developing. A history of HPV has not been shown to change labor and delivery processes.
How is HPV passed to a baby?
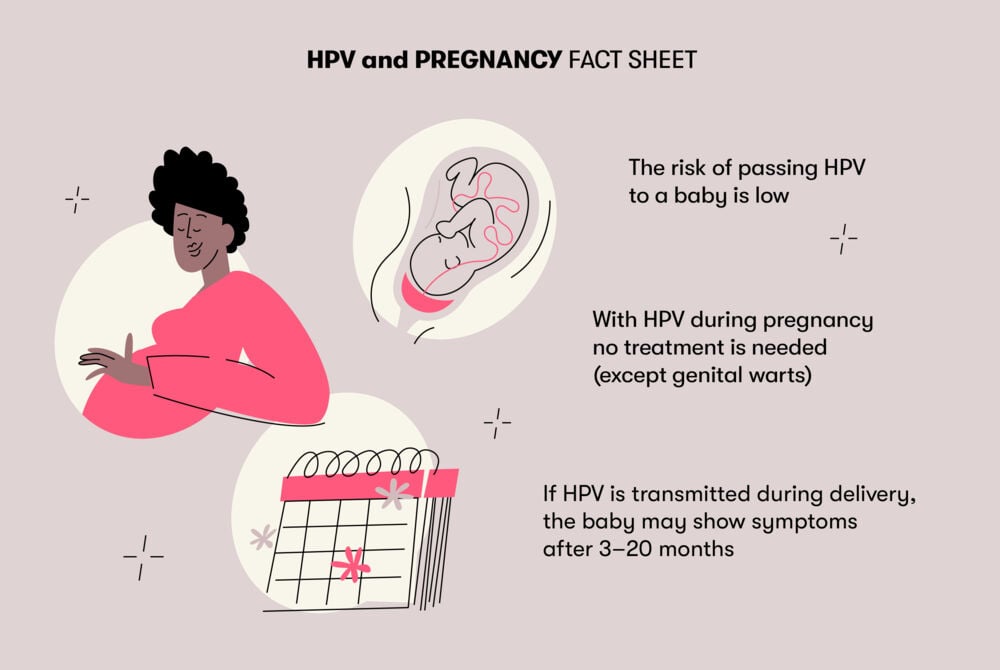
The risk of spreading the virus to a baby during childbirth is relatively low. Nevertheless, current medical literature states that HPV can be passed through the placenta, amniotic fluid, and contact with genital warts.
Medical experts have researched this topic and concluded that if the virus is passed at the time of birth, the baby may have symptoms that appear after several months. The average time is about three months, but it can take as long as 20 months for HPV symptoms (genital warts) to appear.
The treatment of genital warts in infants includes removing them under general anesthesia or applying a topical medication (podophyllin). However, many babies who contract HPV during delivery never become symptomatic because their immune system is strong enough to fight the infection.
So you might be wondering whether a person might need a C-section if they have HPV. Centers for Disease Control and Prevention (CDC) says that a cesarean section can be recommended if large or spread-out warts are blocking the birth canal.
Take a quiz
Find out what you can do with our Health Assistant
HPV while pregnant: What can be done?
If you are diagnosed with HPV during pregnancy, no additional treatment is needed, unless you have genital warts. Typically, smaller warts don’t have to be removed. Warts can grow in size during pregnancy because of hormonal changes and may need to be removed if they become large enough to block the birth canal or to possibly cause heavy bleeding during delivery.
How can passing HPV to a child be prevented?
The best way to prevent getting HPV or spreading HPV to a partner or a baby is by getting the HPV vaccine before being infected. The vaccine does not help if a person has already been infected.
The current recommendations from the World Health Organization (WHO) for the HPV vaccine include routine vaccination of all female children starting at age 9–13. For more information about the HPV vaccine, contact your health care provider.
If you have HPV and notice that you’re developing genital warts or they begin to grow rapidly, let your physician know so they can determine if treatment is necessary.
The risk of passing HPV to a baby is considered low. Studies have shown that the time between the water breaking and delivery may be a critical factor in predicting transmission, so your health care provider will monitor this closely.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.




