How does the body regulate vaginal pH? What are the warning signs of pH imbalance besides odor and unusual discharge? As always, Flo’s here to shed some light on this important subject. Safeguard your health with the latest facts on normal vaginal pH and what to do if there’s ever a problem.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Normal Vaginal pH: How to Test, Balance, and Restore Vaginal pH

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
What is normal vaginal pH?
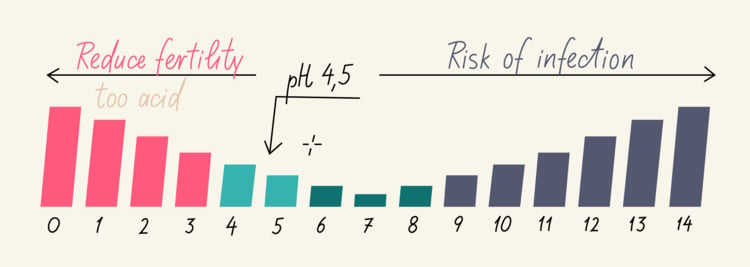
pH describes the acidity or alkalinity of a specific substance and is assigned a number on a scale of 1 to 14. Zero is considered the most acidic, while 14 is the most alkaline. When a substance is labeled as neutral, that usually means it carries a pH level of 7.
A normal vaginal pH of 5 or lower is thought to fall within the healthy range. It registers below the neutral mark of 7 and qualifies as acidic. When vaginal pH is higher (or more alkaline), the chances of developing an infection increase. That’s because as vaginal pH rises, unhealthy bacteria and yeast multiply and affect the reproductive and urinary systems. Numerous factors come into play when vaginal pH balance is disrupted.
Vaginal pH imbalance and potential complications
What is vaginitis?
Vaginitis is a general term that refers to any form of vaginal inflammation, most commonly caused by infection. However, inflammation could also be related to changes in normal vaginal pH, resulting from injury, rough sex, or an allergic reaction. You may have an allergy to certain laundry detergents, soaps, lotions, perfumes, feminine hygiene products, latex condoms, or spermicidal agents.
Ordinarily, vaginal discharge has little or no odor and appears clear, milky, or blood-tinged depending on hormone levels and the current phase of your menstrual cycle. It could be a warning sign of vaginitis if your discharge:
- Gives off an unpleasant odor
- Alters in color (to yellow or green)
- Changes in texture (becoming thick and chunky)
Consult your doctor if you also observe symptoms like burning, itching, or irritation. And if abnormal discharge is accompanied by back pain, painful urination, severe abdominal discomfort, or fever, please seek immediate medical care.
Three different pathogens have been identified in most cases of vaginal infection: bacterial vaginosis, candida vaginitis, and trichomoniasis. Because their symptoms often overlap, these conditions are tough to diagnose without a medical examination.
Symptoms of vaginitis
High vaginal pH that leads to bacterial vaginosis (BV) or another infection might produce the following symptoms:
- Vaginal itching and burning
- Burning while peeing
- Thin and grey, white, or green discharge
- Foul-smelling or “fishy” discharge
Please note that, in some instances, women diagnosed with BV display none of the typical warning signs of infection.
Take a quiz
Find out what you can do with our Health Assistant
Contributing factors for vaginitis
The likelihood of contracting bacterial vaginosis increases under the following circumstances:
- When you engage in sex with new or multiple partners (particularly when it’s between two or more female partners). Though clinical studies link BV to sexual activity, its exact cause isn’t completely understood.
- The lactobacilli levels in your vaginal secretions are lower than they should be. This type of healthy bacteria helps maintain healthy vaginal pH, inhibiting the growth of harmful bacteria.
- Douching with a commercially-prepared or homemade cleansing fluid. It upsets normal vaginal pH and similarly leads to bacterial overgrowth. Note that the vagina has its own natural, self-cleaning process and douching is unnecessary.
Complications of vaginitis
Complications arising from bacterial vaginosis are pretty rare, but it can negatively affect vaginal pH and increase your vulnerability to:
- Sexually transmitted infections (STIs)
The presence of BV makes you more susceptible to contracting infections through unprotected sex like chlamydia, gonorrhea, syphilis, HIV, hepatitis, and herpes.
- Pelvic inflammatory disease (PID)
Recent studies have connected BV to a higher incidence of infection in the uterus and fallopian tubes which produces scarring and possible infertility.
- Preterm births
When BV is contracted during pregnancy, it could potentially trigger premature delivery and low birth weight.
- Post-surgical complications
Serious medical issues may present themselves if you carry BV while undergoing gynecological surgery, such as a dilatation and curettage (D&C) or hysterectomy.
How to test vaginal pH

Vaginal pH is tested with a special type of paper called litmus paper, which changes color when exposed to an acidic or alkaline substance. Assuming normal vaginal pH, a piece of litmus paper would turn from blue to red when held against the vaginal wall for a few seconds, indicating its acidity.
Why use vaginal pH test strips?
Should you ever experience vaginal itching and burning, an unpleasant odor, or unusual discharge, it’s a good idea to test vaginal pH. Just keep in mind that these strips are not intended to check for infections or other conditions (e.g., HIV, chlamydia, gonorrhea, syphilis, hepatitis, or herpes).
It’s important to remember that vaginal pH irregularities do not necessarily indicate an infection. This can only be confirmed by a doctor through physical examination, microscopic observation of discharge, and perhaps a swab collection of bacterial or yeast samples.
If you test positive for high vaginal pH, please make an appointment with your doctor for further evaluation. There are currently no over-the-counter medications available to restore vaginal pH balance.
Alternatively, if you test negative for high vaginal pH, but symptoms persist, a vaginal infection may in fact be present. Double-check all fragrance-containing products you currently use and if the source of irritation cannot be identified, consult your doctor. They’ll be able to thoroughly assess vaginal health using medical and social history, physical exams, and lab tests.
Tips for balancing vaginal pH
Always practice safe sex
Chlamydia, gonorrhea, syphilis, herpes, genital warts, hepatitis, and HIV are transmitted through blood and bodily fluids during unprotected sex. It’s crucial to use a condom every time you engage in sexual activity.
Eat probiotic-rich foods
The female body features remarkable natural defenses to ward off infections caused by bacteria, yeast, and other pathogens. One way it controls vaginal pH is with probiotic lactobacillus or healthy bacteria.
Probiotic-rich products include yogurt, kefir, chia seeds, and cottage cheese. Don’t imagine a boring diet — there may be plenty of tasty dishes!
Maintain good hygiene
Follow these simple steps to ensure healthy vaginal pH:
- Take gentle baths regularly to cleanse the outside of your vagina. Avoid douching (or internal cleansing) as it only disrupts normal vaginal pH. Remember to use only clean water and mild soap as products containing fragrances could irritate the area.
- After urinating or bowel movement, always wipe from front to back (or rinse with warm water) to prevent the spread of unwanted bacteria.
- Do not shave your entire pubic area, which leads to irritation and increases your chances for infection.
- Never apply hair removal creams near the vaginal opening. They’re designed to burn the hair off and are much too harsh.
See the gynecologist regularly
Any woman of childbearing age who is sexually active should get annual gynecological exams, which include a cervical screening and Pap test. Routine screenings catch abnormalities in cervical tissue when it’s more easily addressed. Early diagnosis and treatment of cervical, ovarian, uterine, or breast cancer can stack the odds in the patient’s favor.
Takeaway
The most effective approach to maintaining healthy vaginal pH is by taking all the necessary precautions outlined above and giving your vagina the TLC it deserves. If you can keep vaginal pH at a normal level, you’ll better protect yourself from potential infections and the unpleasant symptoms associated with them.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.




