Yeast infections are more common than you might think. Here’s everything you need to know, including what a yeast infection is, symptoms, and effective treatment so you can feel better quickly
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
What is a yeast infection?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Concerned you might have a yeast infection? You’re far from alone, but what exactly is a yeast infection?
Yeast infections (also known as thrush, monilia, vaginal candidiasis, vulvovaginal candidiasis, and candidal vaginitis) affect 70% of us at some point in our lives — and an unlucky 8% deal with recurrent infections.
In the US alone, yeast infections are responsible for some 1.4 million outpatient visits every year, making them the second most common type of vaginal infection. Because many people never visit the doctor when they have a yeast infection, the true incidence is probably much higher.
All that said, knowing the statistics doesn’t help much when it’s you who’s dealing with the symptoms. No matter how common they are, yeast infections can be a frustrating (and itchy!) experience, and there’s a lot of misinformation out there about the best way to clear them up. Here’s how you can identify a yeast infection and stop it in its tracks.
So, what is a yeast infection?
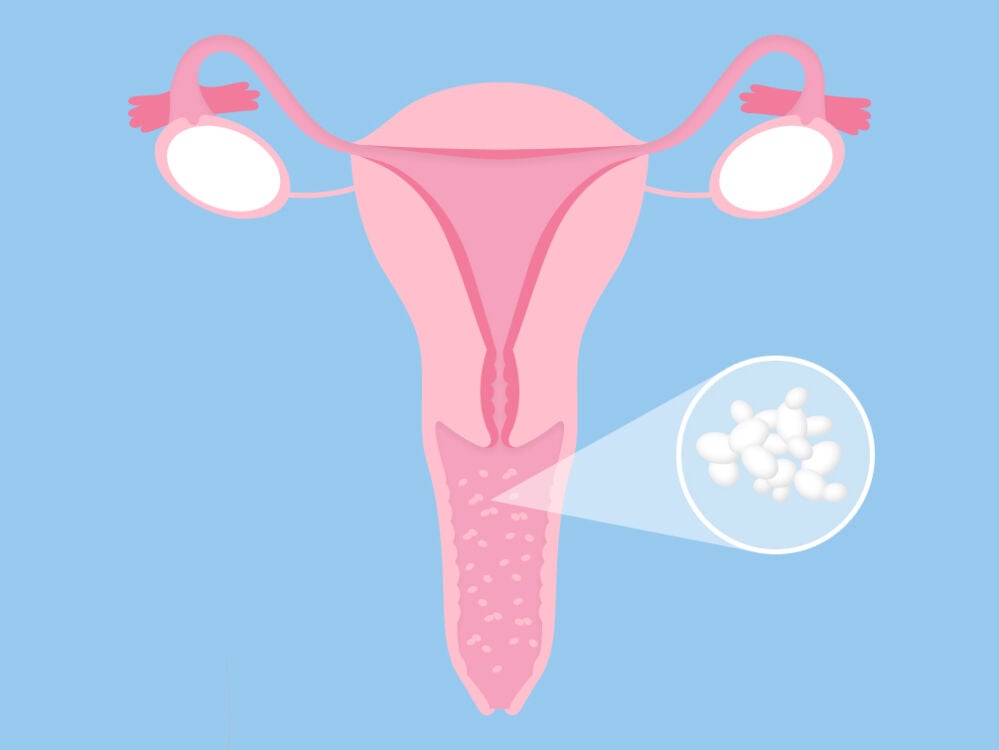
A vaginal yeast infection is a fungal infection that causes irritation, unusual discharge, and intense itching in the vagina and vulva.
Yeast infections are caused by a tiny fungus called candida, which normally lives in the body undetected. If you looked at the body under a microscope, you might find small amounts of candida in the mouth, throat, gut, and on the skin. And when it comes to vaginas, as many as 20% of people have candida there that’s not causing symptoms.
While our body normally has ways of keeping this fungus in check, sometimes our lines of defense break down, and candida starts to multiply out of control. The result is an infection: candidiasis.
Vaginal candidiasis is unpleasant, itchy, and sometimes painful, and it can certainly be a buzzkill in the bedroom. The good news is that it isn’t dangerous, and in most cases, it can be easily treated.
Vaginal thrush vs. yeast infection: What’s the difference?
Vaginal thrush is just another name for a vaginal yeast infection. You might also hear yeast infections called monilia, vaginal candidiasis, vulvovaginal candidiasis, and candidal vaginitis.
Take a quiz
Find out what you can do with our Health Assistant
What does a yeast infection feel like? Yeast infection symptoms
Most commonly, you may notice itching, burning sensations around the vulva and vagina. You might experience pain during sex or while peeing, and there may be a thick, usually odorless white, greenish, or yellow-tinged discharge that looks a bit like cottage cheese.
These symptoms can range from subtle to severe, and they won’t all be present every time. In severe cases, there may be some swelling and redness and fissures (small cracks) that feel like paper cuts in and around the vulva and vagina.
Needless to say, by the time the infection reaches this stage, you’re likely to be pretty miserable.

Why You Keep Getting Yeast Infections
Read medically reviewed articles on topics like this
How to get rid of a yeast infection
Because there are over-the-counter medications available for yeast infections, it can be tempting to stock up and hope for the best. It’s best to hold off on doing this unless you’re really sure it’s a yeast infection (and have had one before), as many other conditions have similar symptoms.
In one small study from the journal Obstetrics & Gynecology, only a third of study participants who purchased over-the-counter yeast treatments had actually self-diagnosed correctly — which means a lot of people are taking antifungal drugs when they shouldn’t be. That’s why it’s best to visit a medical professional, so they can do an examination and swab test.
Pelvic exams aren’t anyone’s idea of a good time, but they are the best way to get the right diagnosis and get started on the path to a full recovery.
"The good news is that it isn’t dangerous, and in most cases, it can be easily treated"
Forget the old wives’ tales, too — yogurt, garlic, and other home remedies haven’t been shown to help treat a yeast infection. Anecdotally, some people swear by inserting a garlic clove into their vagina or adding vinegar to their bathtub. However, there’s no scientific evidence to support this, and (unless your alternative remedy of choice is simply to eat a lot of yogurt) you may end up doing more harm than good.
Antifungal medications, on the other hand, have been shown to reliably clear up yeast infections. You might be prescribed a cream, pills, or suppository as a short course of medication or a one-time thing. You may also need a topical ointment to help with the swelling, itching, and pain. Ointments are more soothing than creams which will often burn irritated, raw skin.
If you’re generally healthy and the infection is uncomplicated, all these forms of treatment should work equally well. However, your doctor may recommend a different course of action if the problem is severe or keeps coming back.
Online Quiz

4 Changes to Your Discharge That Might Signal an Infection
Read medically reviewed articles on topics like this
What causes a yeast infection? Are some people more at risk?
Because the growth of candida is linked to higher estrogen levels, it’s most common in younger people, as well as those taking some types of hormonal birth control (any type that changes your natural balance of estrogen and progesterone). It’s also commonly seen during pregnancy and among postmenopausal people on hormone replacement therapy whose estrogen levels are being artificially raised. Another risk factor is antibiotics.
While antibiotics are great for clearing up bacterial infections caused by bad bacteria, they can also disrupt the natural balance of good bacteria that prevents candida fungus from overgrowing.
You are more likely to get a yeast infection if your immune system has taken a dip (for instance, if you’re very stressed or run down) or if you have diabetes that isn’t well managed. Yeast may be present in your sex partner’s mouth (maybe you’ve heard of thrush in babies), and receiving oral sex could set up yeast overgrowth in your vagina.
If that happens, consult with your health care professional about ways to prevent this.
There are other factors that are more in our control, like clothing choices! You may love your tight, synthetic underwear, but unfortunately, so does candida. Sweaty gym clothes are another culprit — they create the kind of warm, moist environment candida thrives in — so make sure to get out of those wet clothes as soon as you can after exercising.
That’s not to say that a yeast infection means you’ve been unhygienic. In fact, you may have been too clean in the sense that certain soaps and shower gels can aggravate the problem. Because the vagina is self-cleaning, you don’t need to douche — or put any scented products near that area. And although yeast infections are not considered STIs, some people do find sex to be a trigger, particularly if you have used spermicides or received oral sex.
"Because the vagina is self-cleaning, you don’t need to douche — or put any scented products near that area"
How long does a yeast infection last?
How long a yeast infection lasts depends on two things: the severity of the infection and the method of treatment.
Mild infections may get better in a few days with over-the-counter treatments. However, moderate-to-severe yeast infections can take up to two weeks to get better — and need stronger medicines that only your doctor can prescribe.
A word of warning: Failing to treat a yeast infection properly can just make your symptoms worse, increasing the irritation, inflammation, and chances of it coming back again. This can take weeks to fully heal, so it’s best to nip the problem in the bud. If your yeast infection doesn’t go away after treatment or if your symptoms recur within two months of treatment, then contact your health care provider again.
Although yeast infections can be a miserable experience, they should be temporary, and they are not dangerous. So seek advice from your doctor and wave goodbye to that itch for good.
Chronic yeast infections: What causes them?
We now know that there’s a wide range of creams, suppositories, vaginal pills, and oral pills available for treating yeast infections. But what if the infection keeps coming back?
As many as 8% of us have recurring or chronic vaginal yeast infections, defined as four or more flare-ups a year. A 2018 study, which appeared in The Lancet, estimated that 138 million people worldwide are affected by recurring yeast infections every year — and case numbers are increasing. That’s a lot of us dealing with itching, pain, discomfort, disruptions to our sex lives, and unwarranted stigma. So what’s the deal?
The most common causes of a chronic yeast infection
- Drug resistance. Most of the time, the yeast belongs to a strain called Candida albicans, which antifungal drugs can usually knock out. However, about 10% of cases are caused by a different type of candida. Candida auris, Candida glabrata, and Candida parapsilosis are often resistant to common medications, and that might be why your infection keeps returning. Unfortunately, drug-resistant Candida albicans is becoming more prevalent too, so if you do take antifungals, always make sure to take your full course of meds.
- A previous infection never fully went away in the first place. A small study published in The Journal of Infectious Diseases tracked 10 women with recurring yeast infections and found that eight of them had the exact same strain of Candida albicans every time. This suggests their yeast infections might have been a “relapse” rather than a reinfection. The best thing you can do to prevent this is to be vigilant about medication. Even if your symptoms have gone away, it’s important to keep applying the cream or taking the pills exactly as they were prescribed.
There are also a few medical conditions that make yeast infections more likely to return:
- Uncontrolled diabetes, which can cause blood sugar levels to spike. This, in turn, leads to higher sugar levels in the vagina, which is essentially more food for the candida to feed on. People with diabetes may also have a reduced immune response, which makes it harder for their bodies to wipe out the infection. It's unlikely your recurring thrush is caused by diabetes, but if you’re having symptoms like peeing more than usual (particularly at night), losing weight without actively trying, and/or feeling thirsty all the time, it’s a good idea to see a medical professional to get it checked out.
- A weakened immune system, perhaps because you’re feeling run down or stressed out. People with conditions like HIV fall into this bracket, too, as do people taking certain medications, like corticosteroids or TNF inhibitors. (If that’s you, talk to your provider.) There are also genetic factors that make it tougher for some people’s immune systems to deal with candida.
Chronic yeast infection treatment: What helps?
So what should you do about recurring, chronic yeast infections? While your first impulse might be to rush to the drugstore, it’s best to see a medical professional to get a proper diagnosis and prescription.
For one thing, it might not be a yeast infection at all. You can find a list of other things a yeast infection could be below — and it goes without saying that antifungals won’t help if it’s actually a bacterial or viral infection. In fact, the creams can make irritation worse, especially if it is caused by exposure to soaps or other scented “hygiene” products.
Secondly, recurring or “complicated” infections generally warrant a different approach. Yeast infections can be treated in lots of ways, including creams, pills, suppositories, or ointments, so there are a few different options your provider might want to try.
It’s possible they might prescribe suppressive treatment that you take for a longer period, even after symptoms have gone away. And if there’s something else going on, (think ongoing antibiotic treatments, the need for long-term drugs like corticosteroids, diabetes, or HIV), they’ll need to factor that into your treatment plan.
"138 million people worldwide are affected by recurring yeast infections every year — and case numbers are increasing"
In addition to all that, they might take a swab to send off to a lab to check which strain of candida is causing the infection. If it’s a drug-resistant variant, they may need to refer you to a specialist. Don’t worry — there are lots of treatment options out there. Sometimes, it’s just a matter of finding the right one.
Recurring yeast infections can have a serious impact on your quality of life. We know it can be really challenging at times, but don’t give up. Even the most stubborn or persistent infection can be banished with the right treatment.
How to know if you have a yeast infection: What else could it be?
If you’ve recently been on antibiotics, chances are that your clumpy discharge, itching, and burning is a yeast infection. But if you have symptoms and you don’t have a classic cause, you should see your health care professional for a definite diagnosis.
There are other conditions that cause similar symptoms:
- Vulval dermatitis — Caused by an allergic reaction or an irritant, symptoms include chronic itching and a rash.
- Genital herpes — A sexually transmitted infection, it can cause blistering and ulceration of the skin and be itchy and painful.
- Bacterial vaginosis — This is the most common vaginal infection, and it’s caused by a bacterium rather than a fungus. The main symptom is a strong-smelling grayish, thin vaginal discharge.
- Lichen sclerosis — Most common in postmenopausal people, this is a skin condition, not an infection, that can cause itching, redness, and pain.
- Urinary tract infections — Symptoms include pelvic pain and a frequent need to urinate. The burning sensation with urination may be similar to a yeast infection.
- Vestibulitis — This causes a severe stinging, burning pain at the entrance to the vagina during sex and sometimes during everyday activities.
- Lichen simplex chronicus — This is caused by persistent itching and scratching unrelated to an infection. Scratching can make itching worse, and over time, the skin can become chronically irritated, red, swollen, and itchy.
All of these conditions can and should be treated — so whether it’s a yeast infection or something else, you owe it to yourself to get the right diagnosis and medication.
How long to wait for sex after yeast infection treatment
If you have a yeast infection, it’s better not to have sex because it slows down the healing process and can be passed back and forth from partner to partner. Although candidiasis isn’t a sexually transmitted infection, your partner could end up with thrush from unprotected sex, depending on their immune response.
Sex can also make your symptoms worse because the vaginal tissue is already inflamed and sore — and it’s likely to be uncomfortable too. Often, women report the itching getting worse after sex.
You’re better off waiting until all of your symptoms have cleared up after a course of treatment.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Jeanmonod, Rebecca, and Donald Jeanmonod. 2021. “Vaginal Candidiasis.” In StatPearls. Treasure Island (FL): StatPearls Publishing. “Vaginal Candidiasis.” Centers for Disease Control and Prevention, 13 Oct. 2021. www.cdc.gov/fungal/diseases/candidiasis/genital/index.html.
“Differential Diagnosis.” National Institute for Health and Care Excellence, https://cks.nice.org.uk/topics/candida-female-genital/diagnosis/differential-diagnosis/. Accessed 19 May 2022.
Ferris, Daron G., et al. “Over-the-Counter Antifungal Drug Misuse Associated with Patient-Diagnosed Vulvovaginal Candidiasis.” Obstetrics and Gynecology, 99 (3): 2002, pp. 419–25.
Women’s Health Team. “Do Home Remedies Actually Work for Yeast Infections?” Cleveland Clinic (blog), 8 Nov. 2019, https://health.clevelandclinic.org/do-home-remedies-actually-work-for-yeast-infections/.
Krapf, Jill M., “Vulvovaginitis.” Practice Essentials, Background, Anatomy, Medscape, 2 May 2022, www.medscape.com/answers/2188931-94650/what-is-the-role-of-contraception-in-the-pathogenesis-of-vulvovaginal-candidiasis.
“Thrush in Men and Women.” NHS Choices, www.nhs.uk/conditions/thrush-in-men-and-women/. Accessed 19 May 2022.
“Vaginal Yeast Infections More Common When Using Contraceptives or Spermicides, or Participating in Receptive Oral Sex.” University of Michigan News, 11 Dec. 2006, https://news.umich.edu/vaginal-yeast-infections-more-common-when-using-contraceptives-or-spermicides-or-participating-in-receptive-oral-sex/.
Denning, David W., et al. “Global Burden of Recurrent Vulvovaginal Candidiasis: A Systematic Review.” The Lancet, 2 Aug. 2018, https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(18)30103-8/.
“Antifungal Resistance in Candida.” Centers for Disease Control and Prevention, 18 May 2020, www.cdc.gov/fungal/diseases/candidiasis/antifungal-resistant.html.
Vazquez, J. A., et al. “Karyotyping of Candida Albicans Isolates Obtained Longitudinally in Women with Recurrent Vulvovaginal Candidiasis.” The Journal of Infectious Diseases, 170 (6): 1994, pp. 1566–69.
Rodrigues, Célia F., et al. “Candida Sp. Infections in Patients with Diabetes Mellitus.” Journal of Clinical Medicine Research, 8 (1), 2019, https://doi.org/10.3390/jcm8010076.
Jaeger, M., et al. “A Systems Genomics Approach Identifies SIGLEC15 as a Susceptibility Factor in Recurrent Vulvovaginal Candidiasis.” Science Translational Medicine, vol. 11 (496), 2019, https://doi.org/10.1126/scitranslmed.aar3558.
Vilano, Samantha E., and Cynthia L. Robbins. “Common Prepubertal Vulvar Conditions.” Current Opinion in Obstetrics & Gynecology, 28 (5): 2016, pp. 359–65.
Schwebke, J. R., “Bacterial Vaginosis.” Current Infectious Disease Reports, 2 (1): pp. 14–17.
“Lichen Sclerosus.” NHS Choices,. www.nhs.uk/conditions/lichen-sclerosus/. Accessed 19 May 2022.




