Yeast infections are relatively common, but did you know that you can also get a yeast infection under your breasts?
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Yeast Infection Under Breasts and Nipple Thrush: Symptoms and Treatment


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Another name for a breast yeast infection is breast and nipple thrush (BNT). It can develop in moist and warm places — such as skin folds — and appear under the breasts and on the nipples.
Signs and symptoms of breast yeast infection
These are some of the most common symptoms of breast and nipple thrush:
Rash under breast
Candida infections on the skin don’t usually generate discharge that smells. A smelly rash under the breasts could signal a different condition, such as a bacterial skin infection.
Thrush can cause a breast rash that is raised, swollen, tender, shiny, and red. As thrush progresses, the affected area can expand quickly. It can also make the skin flaky, discolored, and cracked.
Itching
Fungal infections tend to cause intense itching and burning sensations. These symptoms can range from mild to severe.
Take a quiz
Find out what you can do with our Health Assistant
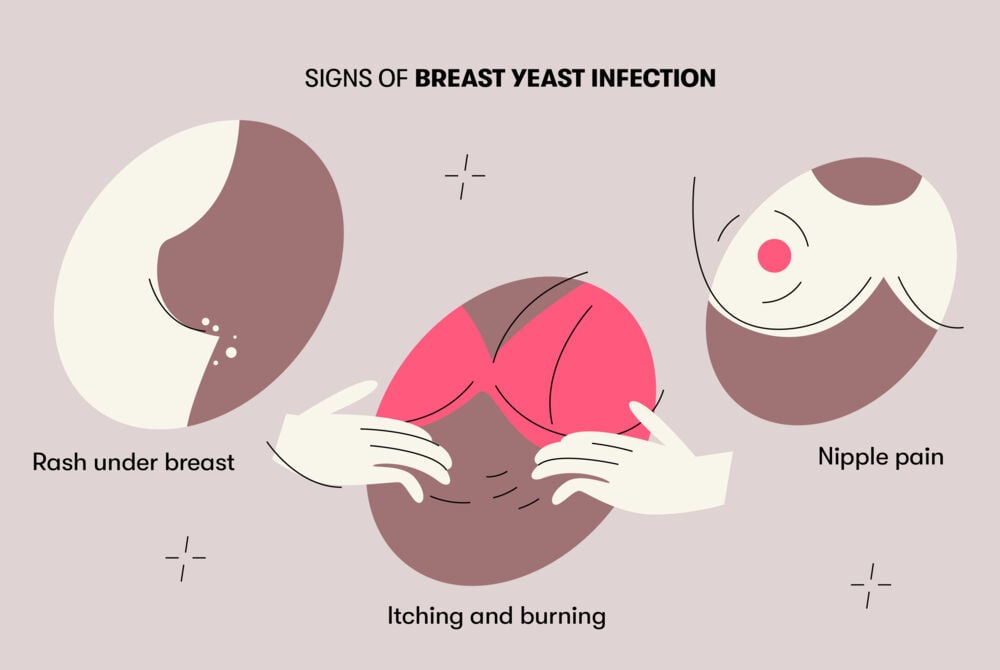
Nipple pain
Nipple pain caused by thrush typically occurs after expressing milk. It can also be painful when clothing brushes against the affected area or cause a stabbing or shooting pain during feeds. Nipples may appear bright pink.
If you experience a sudden increase in breast pain, it could be a bacterial superinfection in addition to the initial thrush.
You may also see signs of thrush in your baby’s mouth or on your baby’s bottom, or both. Thrush in the mouth causes a thick, white coating on the tongue, white spots on the inside of the cheeks, or both. Thrush on a baby’s bottom looks like a bright red rash with spots around it. This rash does not resolve without antifungal cream.
Causes
Thrush is caused by a fungus called Candida albicans, which grows in moist and warm places, such as skin folds.
Candida is part of the normal human skin microbiome, which are the bacteria, viruses, and fungi that normally live on our skin. In some cases, our microbiome can experience an overgrowth that leads to infections.
Yeast infections under breasts commonly occur in conjunction with breastfeeding. However, they can still affect anyone regardless of whether they’re breastfeeding, their breast size, or their age.
Thrush can occur shortly after beginning to breastfeed, especially if the baby has oral thrush. Oral thrush is especially common for people who had vaginal candidiasis at the time of childbirth or if their baby has taken antibiotics.
Although thrush doesn’t usually affect healthy skin, it can quickly affect damaged skin, and if left untreated, it may cause severe breast and nipple pain, itching, redness, and inflammation. This can lead to a skin infection if the inflamed area becomes cracked or if scratching causes open sores or raw spots. Other factors that increase the risk of yeast infection on breasts and nipples include:
- Cracked nipples or skin lesions during breastfeeding
- Use of breast pads
- Recent antibiotic use
- Previous vaginal yeast infection
- High stress levels
- Inadequate diet
- Chronic illnesses, such as diabetes or HIV
- Environmental factors, including warm climates and humidity
- Not rinsing or towel drying the area under or around the breast

Why You Keep Getting Yeast Infections
Read medically reviewed articles on topics like this
How to tell breast yeast infection from other conditions
Other breast infections can cause similar skin symptoms to thrush, including:
- Herpes, which causes clusters of small, fluid-filled blisters
- Bacterial infections that cause systemic symptoms like fever and pus discharge
- Mastitis, which can cause a painful, swollen red lump in the breast
- Contact dermatitis, which causes a dry, scaly rash that appears after contact with an allergen
It’s always a good idea to visit your midwife, lactation consultant, or other health care professional for guidance. The first thing your health care provider will do is to take your medical history and perform a physical examination. If the diagnosis is unclear, they may take a sample of discharge or fluid, perform an ultrasound, or request additional lab tests.
Treatment
In most cases, thrush can be treated with simple over-the-counter medications. Topical antifungal medications that can be applied directly to the skin are effective for the treatment of fungal skin infections, and they frequently have long-lasting results.
These medications are often considered the preferred form of treatment for infections like thrush. Common topical and oral antifungal medications used for thrush include:
- Miconazole
- Nystatin
- Clotrimazole
- Bifonazole
- Fluconazole (oral)
Your health care provider might also prescribe anti-inflammatory medications or steroid creams to relieve your symptoms while the infection is clearing.
Mild yeast infections should clear up in as few as three days. Sometimes, they don’t even require any treatment. Moderate to severe infections may take one to two weeks to resolve with treatment.
It’s important to rule out oral thrush in your baby and make sure you’re using correct technique while breastfeeding. If your baby is diagnosed with oral thrush, they may require a course of antifungal treatment.
In addition to treatment for yourself and your baby, it is important to:
- Clean bottle nipples and pacifiers thoroughly after use by boiling for five minutes. Replace weekly, if possible.
- Wash your hands thoroughly after diaper changes and before and after applying any creams or lotions to prevent the spread of thrush.
- Wash towels, bras, cloth nursing pads, and similar items in hot, soapy water and air dry.
Prevention
The best way to prevent yeast infections under your breasts is by keeping the area clean and dry. Other strategies that can help prevent thrush include:
- Keep nipples dry. If you use breast pads to prevent leaks, it’s best to use disposable pads and change them frequently.
- Sleeping in your bra can irritate your skin, so you may want to avoid this practice to let your skin heal properly.
- Wear a comfortable bra made of natural materials, like cotton.
- Wash your nipples and the skin under your breasts with warm water after breastfeeding or sweating, and pat them dry.
Fortunately, yeast infections under the breasts typically respond well to treatment.
If your symptoms don’t resolve within a week or two, see your health care provider. The treatment you choose may not have been strong enough to cure the infection, and another treatment may be prescribed.
You also need to see your health care provider if the infection returns within two months. Recurrent yeast infections aren’t uncommon, especially during breastfeeding.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.




