Perimenopause (the transition to menopause) doesn’t just happen overnight. Here are the signs to expect during this time.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
7 signs of perimenopause everyone needs to know about


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Maybe you’ve noticed that your periods have become more unpredictable. Or perhaps you feel like you’ve suddenly stepped into the least-relaxing sauna ever (hello, hot flashes!).
These are just two potential signs of perimenopause. Perimenopause simply means the years leading up to menopause. You’re diagnosed as having gone through menopause when you haven’t had a period for 12 months.
During perimenopause, the amount of estrogen your ovaries produce begins to fluctuate. This can cause symptoms you might not have experienced before. But everyone’s unique, and not all people experience perimenopausal symptoms. That being said, here are a few common ones to look out for.
Key takeaways
- Perimenopause (the transition into menopause) will most often start in your 40s, but could begin anywhere between your late 30s and 50s.
- It will last for four years on average but could last for up to eight years.
- Perimenopause can cause a number of telltale symptoms, including irregular periods, hot flashes, poor sleep, vaginal dryness, mood swings, brain fog, and bladder problems.
What is perimenopause?
We now know that perimenopause is the years of transition into menopause, but what’s actually happening to your body during this time? Basically, your hormone production begins to change. In particular, the levels of estrogen produced by your ovaries start to fluctuate, meaning that they could go up and down.
It’s this erratic estrogen production that can cause those telltale perimenopause symptoms, such as changes to your cycle, mood swings, and brain fog. When your estrogen levels are low, you could experience hot flashes and night sweats. When they are high, you may experience breast tenderness and an irregular menstrual flow. Want more expert info? Check out our detailed guide to perimenopause.
Know that you don’t need to cope with these symptoms alone. There’s support and treatment available from your doctor.
What is the average age for perimenopause to start?
Perimenopause begins somewhere between your late 30s and 50s, but most often in your 40s, on average around 47 years old.
In comparison, menopause can occur anytime between the ages of 45 and 55, and the average age for this is 51 in the United States. After that, you are postmenopausal.
How long does perimenopause last?
Perimenopause lasts for four years on average, but this time frame will vary from person to person. Some people might only experience it for a few months, while others could have symptoms for up to eight years.
Take a quiz
Find out what you can do with our Health Assistant
Signs of perimenopause
1. Your period is becoming more unpredictable and irregular
This is probably what you’ll notice first. Your period itself might become shorter or longer. Maybe you’ll get longer or shorter gaps between periods (irregular cycles). The bleeding might become heavier or lighter.
“I knew I was nearing [menopause] when my periods changed from a very regular 28-day cycle to shorter or longer cycles,” shares one person in Secret Chats. And the amount of bleeding would change from one cycle to the next. Some periods would be heavy; others would be super light, they add.
With perimenopause periods, there’s no one-size-fits-all pattern, and some people actually have regular periods right up until menopause.
While it’s usual to see period changes during perimenopause, certain changes in your bleeding should be checked out by your doctor to make sure there’s nothing else going on. See your doctor if:
- Your bleeding is really heavy — if you need to change your period products every one to two hours for two or more hours.
- Your bleeding lasts for more than seven days.
- You’re bleeding between periods.
- Your periods are regularly coming fewer than 21 days apart.
2. You’re feeling hot or cold all of a sudden
“Suddenly it was like every pore on my body was a wide-open faucet! I would be at my friend’s house and start pouring sweat out of nowhere while doing nothing.”
Sound familiar? This is how someone in Secret Chats described the experience of hot flashes. They’re super common during perimenopause. Around 80% of perimenopausal women get them.
So what’s the deal? Also called “vasomotor symptoms,” a hot flash is when you feel a sudden wave of heat in your body, often with other symptoms like sweating. Your skin might turn red, your heart might beat rapidly, and after the hot flash, you might feel cold and shivery. You might get all or some of those symptoms.
They can last anywhere from 30 seconds to 10 minutes, and they can vary in frequency. Some people find them OK to manage, while for others, they can feel unbearable and interfere with sleep.
Because of fluctuating hormone levels, hot flashes can happen even when there’s no obvious trigger, like spicy food or hot weather. You can help manage hot flashes by wearing layers (hot tip: breathable cotton, which wicks away sweat) that you can take off when you’re feeling the heat or by popping a portable fan in your bag to use as needed. We’ve got even more tips over here.
When you have hot flashes at night while you’re sleeping, they’re known as night sweats. Which brings us to …

3. Your sleep is getting worse
Maybe you struggle to fall asleep. Maybe you wake up in the middle of the night and lie there, tossing and turning, increasingly frustrated and anxious as the morning edges closer. Research shows that up to 60% of perimenopausal women have disrupted sleep. Hot flashes could be one reason.
A 2006 study from the Stanford University School of Medicine looked at the association between hot flashes and insomnia in 982 women aged 35 to 65 years. Of those, 79% of women in perimenopause reported hot flashes, with almost 57% of those women also reporting insomnia. The researchers found that the more severe the hot flashes were, the more likely a woman was to report insomnia.
Mood changes (more on these later) can contribute to poor sleep too. And it can become a vicious cycle. A terrible night’s sleep hardly does wonders for your mood, right?
If your symptoms are affecting your sleep, it’s time to see your health care provider. But there are steps you can take to try to manage disrupted sleep in the meantime, like adapting your sleep environment (aim for a quiet, cool, dark bedroom). A ceiling or bedside fan, light cotton bedding, and a bottle of water near your bed are good ideas too if hot flashes are keeping you awake.
4. Your vagina feels dry
You’re getting intimate and try penetration, but your vagina feels dry. It’s uncomfortable, painful, and frankly, not feeling great.
Sound familiar? Vaginal dryness is common in perimenopause. The landmark US Study of Women Across the Nation followed more than 2,400 women over 17 years and found that just over 19% of women of perimenopause age (42 to 53) were affected by vaginal dryness.
It’s all due to your estrogen levels. Estrogen is in charge of helping your vagina stay lubricated and elastic, so when perimenopause starts changing your estrogen levels, the result can be dryness and thinning of the vaginal tissue.
You can help ease it by using moisturizer in and around your vagina. There are specific products designed for this. Lubricants are also a good call. You can use these alongside vaginal moisturizer to make penetrative sex more comfortable. And some people find that taking vaginal estrogen (available as a tablet, vaginal suppository, cream, gel, or ring that you insert into your vagina) helps a lot. Talk to your health care provider to learn more.
5. Your mood is a roller coaster
Around 4 in 10 women go through mood symptoms during perimenopause that are similar to premenstrual syndrome (PMS). You might feel anxious, stressed, angry, irritable, sad, lacking in confidence — or all of the above! But unlike PMS, these mood symptoms aren’t necessarily linked to your menstrual cycle — so that could be key in figuring out whether your moods are linked to perimenopause.
One person in Secret Chats describes having “mood swings and sudden anger, followed by days of just holding back from crying.”
Research also shows that the risk of depression spikes during perimenopause.
Mood symptoms can be compounded by perimenopause sleep problems and, of course, the challenges we face as we go through life, whether that’s a demanding job or caring for our families.
Getting good sleep can make a big difference to your mood, as can other lifestyle strategies, like eating a healthy diet, getting enough exercise, and managing stress with techniques such as massage, journaling, or meditation.
If you feel like you’re struggling with your mood and mental health, don’t hesitate to speak to your health care provider. Help and treatment are out there, and we’ve got more expert info here.
6. You’re finding it harder to focus and remember things
You might become forgetful. Maybe upon entering a room, you have absolutely no idea why you’re there. Or perhaps your powers of concentration have dulled. You try to focus on a work task, but your mind veers off in another direction.
In a 2022 study from University College Hospital London, more than 68% of women in perimenopause reported experiencing brain fog. Not sure what this is or if you might be experiencing it? Read our expert guide.
The good news is, there are steps you can take to conquer those cognitive blips. You might find it helpful to slow things down. Recognize when you’re distracted and take a moment to breathe and refocus. Regular exercise and improving your sleep habits can help your brain function at its best.
7. Your bladder is giving you a hard time
Your pee patterns can be affected by perimenopause too, for a couple of reasons. Another important job estrogen does is to keep your pelvic floor muscles well toned, which helps your bladder to work properly. Lower levels of the hormone can mean you need to pee more often or might get more frequent urinary tract infections. Not fun, right?
Also, leaking a little pee when you exercise, laugh, or sneeze is another common experience during perimenopause. This isn’t only due to your hormones, but it can happen more often as menopause approaches.
Simple pelvic floor exercises (Kegels) might make a world of difference though. A pelvic floor physical therapist can help you ace the technique. Always speak to a health care provider if you’re worried something’s not right with your bladder or pelvic floor.
Other signs of perimenopause
Maybe you’re wondering about other perimenopause hallmarks. Here’s the thing: The list of perimenopause signs isn’t exhaustive, and one person’s experience may be different from another’s.
Some folks find that they have sore, tender boobs during perimenopause, while others notice changes to their sexual desire, skin dryness, weight gain, or joint pains. You might also experience fatigue — we’ve got the lowdown here.
Perimenopause symptoms can come on gradually over time, so you might not connect the dots and realize that’s what’s happening at first.
What's the treatment for perimenopause?
If perimenopausal symptoms are disrupting your life, you don’t just have to put up with them. In fact, there are a number of treatment options available to help you feel like yourself again. These differ according to which symptoms you’re experiencing and how severe they are.
Some of the main types of perimenopause treatment include:
- Hormone therapy (HT, also known as hormone replacement therapy, or HRT): This can include a combination of estrogen and progesterone for most people or just estrogen, and it is the most effective treatment for hot flashes, night sweats, and vaginal dryness.
- Certain antidepressants are another option to treat hot flashes and night sweats if you can’t take estrogen or have a mood disorder.
- An anti-seizure medication called gabapentin can also relieve hot flashes and night sweats.
- If you’re already using hormonal contraceptive pills, then they can be prolonged in the early stages of perimenopause or if you are avoiding pregnancy. These could help to stabilize your fluctuating hormone levels, which in turn could help to decrease perimenopause symptoms.
- Vaginal creams and lubes can provide relief from vaginal dryness or pain during sex.
If you’d like to explore treatment for your symptoms, reach out to your doctor. They can offer advice to help you decide which option is best for you.
READ MORE: Birth control for perimenopause: How can it help?
It’s important to remember that perimenopause is a stage of life that every woman and person who has a period will pass through at some point. But that doesn’t mean every experience of it will be the same, especially when it comes to perimenopause symptoms. They’re often as individual as our cycles.
The symptoms associated with perimenopause can be challenging, so we’d recommend having open conversations with friends and family, along with your health care provider, so that you have the support in place that you need. Remember: You don’t need to suffer in silence with perimenopause symptoms. There are things your health care provider can do to help.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Abraham, Cynthia. “Experiencing Vaginal Dryness? Here’s What You Need to Know.” The American College of Obstetricians and Gynecologists, Oct. 2020, www.acog.org/womens-health/experts-and-stories/the-latest/experiencing-vaginal-dryness-heres-what-you-need-to-know.
Baker, Fiona C., et al. “Sleep and Sleep Disorders in the Menopausal Transition.” Sleep Medicine Clinics, vol. 13, no. 3, 2018, pp. 443–56, https://doi.org/10.1016/j.jsmc.2018.04.011.
Bansal, Ramandeep, and Neelam Aggarwal. “Menopausal Hot Flashes: A Concise Review.” Journal of Mid-Life Health, vol. 10, no. 1, 2019, pp. 6–13, https://doi.org/10.4103/jmh.jmh_7_19.
Bilodeau, Kelly “Sleep, Stress, or Hormones? Brain Fog during Perimenopause.” Harvard Health Publishing, 9 Apr. 2021, www.health.harvard.edu/blog/sleep-stress-or-hormones-brain-fog-during-perimenopause-202104092429.
“Breast Pain: Not Just a Premenopausal Complaint.” Harvard Health Publishing, 7 July 2020, www.health.harvard.edu/pain/breast-pain-not-just-a-premenopausal-complaint.
Harlow, Siobán D., and Pangaja Paramsothy. “Menstruation and the Menopausal Transition.” Obstetrics and Gynecology Clinics of North America, vol. 38, no. 3, 2011, pp. 595–607, https://doi.org/10.1016/j.ogc.2011.05.010.
Harper, Joyce C., et al. “An Online Survey of Perimenopausal Women to Determine Their Attitudes and Knowledge of the Menopause.” Women's Health, vol. 18, 2022, pubmed.ncbi.nlm.nih.gov/35758176/.
“How Does Menopause Affect My Sleep?” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/wellness-and-prevention/how-does-menopause-affect-my-sleep. Accessed 24 Aug. 2023.
Li, Tao, et al. “Prevalence and Risk Factors of Stress Urinary Incontinence among Perimenopausal Women and Its Influence on Daily Life in Women with Sexual Desire Problem.” Current Medical Science, vol. 39, 2019, pp. 615–21, https://doi.org/10.1007/s11596-019-2082-7.
“Menopause.” NHS, www.nhs.uk/conditions/menopause/. Accessed 18 Oct. 2023.
“Menopause and Your Mental Wellbeing.” NHS Inform, 29 Nov. 2022, www.nhsinform.scot/healthy-living/womens-health/later-years-around-50-years-and-over/menopause-and-post-menopause-health/menopause-and-your-mental-wellbeing.
“Menopause 101: A Primer for the Perimenopausal.” The North American Menopause Society, www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal. Accessed 18 Oct. 2023.
Ohayon, Maurice M. “Severe Hot Flashes Are Associated with Chronic Insomnia.” Archives of Internal Medicine, vol. 166, no. 12, 2006, pp. 1262–68, https://doi.org/10.1001/archinte.166.12.1262.
“Perimenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21608-perimenopause. Accessed 18 Oct. 2023.
“Perimenopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666.
Pinkerton, Joann V. “Menopause.” MSD Manual Consumer Version, July 2023, www.msdmanuals.com/en-gb/home/women-s-health-issues/menopause/menopause
“Scenario: Managing Women with Menopause, Perimenopause, or Premature Ovarian Insufficiency.” National Institute for Health and Care Excellence, cks.nice.org.uk/topics/menopause/management/management-of-menopause-perimenopause-or-premature-ovarian-insufficiency/. Accessed 3 Aug. 2023.
Silver, Nazanin E. “Mood Changes during Perimenopause Are Real. Here’s What to Know.” The American College of Obstetricians and Gynecologists, Apr. 2023, www.acog.org/womens-health/experts-and-stories/the-latest/mood-changes-during-perimenopause-are-real-heres-what-to-know.
“The Menopause Years.” The American College of Obstetricians and Gynecologists, Dec. 2018, www.acog.org/womens-health/faqs/the-menopause-years.
“Urinary Incontinence.” The North American Menopause Society, www.menopause.org/for-women/sexual-health-menopause-online/causes-of-sexual-problems/urinary-incontinence. Accessed 3 Aug. 2023.
Waetjen, L. Elaine, et al. “Factors Associated with Developing Vaginal Dryness Symptoms in Women Transitioning through Menopause: A Longitudinal Study.” Menopause, vol. 25, no. 10, 2018, pp. 1094–104, https://doi.org/10.1097/gme.0000000000001130.
“What Is Menopause?” National Institute on Aging, www.nia.nih.gov/health/what-menopause. Accessed 18 Oct. 2023.
History of updates
Current version (17 November 2023)
Published (07 March 2024)
In this article
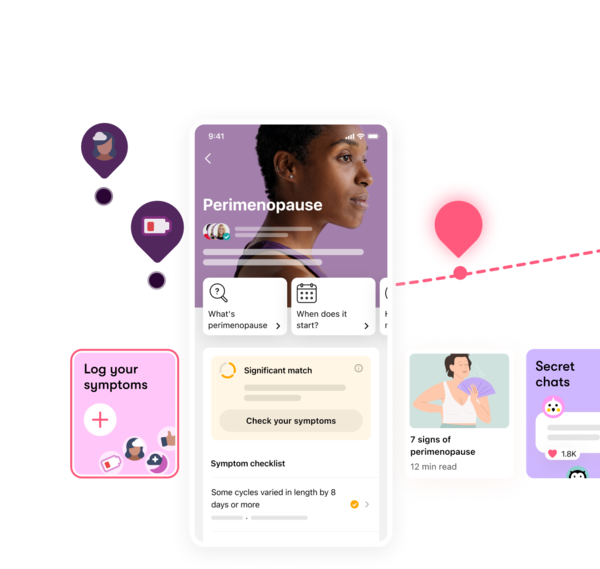
Track your perimenopause journey in the Flo app
-
Log symptoms and get tips to manage them
-
Learn what to expect with expert-led articles and videos
-
Connect with others who can relate to how you're feeling




