Everything you need to know if you’re thinking of switching to hormonal birth control.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Hormonal birth control: Is it right for you?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Thinking about starting birth control? Or switching it up? The sheer amount of contraceptive options available can feel overwhelming (particularly hormonal vs. nonhormonal birth control), so we’re here to help.
Flo spoke to Dr. Jennifer Boyle, obstetrician and gynecologist at Massachusetts General Hospital, Massachusetts, US, to answer some of your questions on hormonal birth control — from the different types of contraceptives to potential side effects and how to choose the right one for you.
Once you’ve learned about hormonal birth control, read our guide to the nonhormonal options.
Key takeways
- There are multiple types of hormonal contraception. Finding the right one depends on your birth control needs, your lifestyle, and your medical history. Your doctor can help you decide.
- The most common forms of hormonal birth control include the pill, implant, intrauterine device, injection, contraceptive patch, and vaginal ring.
What’s the difference between hormonal contraceptives and nonhormonal contraceptives?
As their name suggests, hormonal contraceptives contain hormones, specifically those that help keep your menstrual cycle in check.
We have lots of different types of hormones in our body that do vastly different things. Here’s the lowdown on some of the ones that impact your menstrual cycle and reproductive health. The female sex hormones are progesterone and estrogen. Think of these hormones as chemical messengers from the brain telling the body to do something.
Over to Dr. Boyle to explain the jobs these two hormones do in more detail: “The menstrual cycle involves a gradual increase in estrogen that leads to ovulation [when your ovaries release an egg]. Estrogen then gradually decreases. After ovulation, progesterone is released. It increases and decreases as well. When both estrogen and progesterone fall, this triggers a menstrual bleed, which is the shedding of the uterine lining that developed throughout the cycle.”
They work by keeping your hormones steady, as Dr. Boyle explains.
“When taking hormonal birth control, you don’t have these same changes in hormone levels,” she says. “You receive (in most cases) the same amount of estrogen and progestin for COCs and progestin for POPs every day. If people have bleeding while using hormonal birth control, it is not a true menstrual period, but what we call a ‘withdrawal bleed.’” You might confuse withdrawal bleeding with a period, and that’s understandable.
During the week when you have a pause in your birth control or take placebo contraception, your estrogen and progestin levels decrease because you are pausing the medication. This triggers a withdrawal bleed. It tends to be lighter because the lining of the uterus does not grow and build up as much as it would without hormonal contraception.
Examples of hormonal birth control include the combined contraceptive pill and the implant. Condoms are a good example of an easily accessible form of nonhormonal birth control. To make it easier, we’ve created a helpful guide to nonhormonal birth control methods.

Types of hormonal contraceptives
One study found that virtually all sexually active American women aged 15 to 44 had used at least one method of contraception during their lifetime. That’s 99% or 53 million women. But not everyone will use the same type of birth control. What suits you best won’t be the same for everyone.
When looking at your options, your doctor will talk to you about your medical history, lifestyle factors (like whether you smoke), and reasons for taking birth control. COCs, for example, can increase your chance of blood clots, so they may not be right for you.
Knowing a little bit more about each option available to you may help you feel more confident when talking to your doctor.
Birth control pills

You might have heard of oral contraceptives or birth control pills. Typically, there are two different types of birth control pills: combined oral contraceptive pills (COCs) and progestin-only pills (POPs). As their names suggest, they contain either both or one of the hormones that control our cycles.
“COCs contain both estrogen and progestin,” explains Dr. Boyle. “Progestin is the synthetic form of the body’s natural hormone, progesterone. POPs contain only progestin. In the United States, there are currently only two types of POP: norethindrone 0.35 mg and drospirenone (Slynd) 4 mg. Drospirenone is new to the market.”
While COCs and POPs are both pills that you swallow and are designed to prevent pregnancy, Dr. Boyle says, “They work in slightly different ways.”
She explains, “COCs make it so the ovary does not release an egg (ovulation) — and in that way, a person can’t become pregnant. They also affect cervical mucus by making it thicker, making it harder for sperm to travel into the uterus and up to the tube where they would fertilize an egg.”
POPs can prevent ovulation (although 4 in 10 women will continue to ovulate) and thicken your cervical mucus, but they also thin the lining of your uterus.
When taken correctly, the pill is over 99% effective at preventing pregnancy. However, you might forget to take it, and that’s fairly common, so the pill is thought to be about 93% effective.
Birth control implant
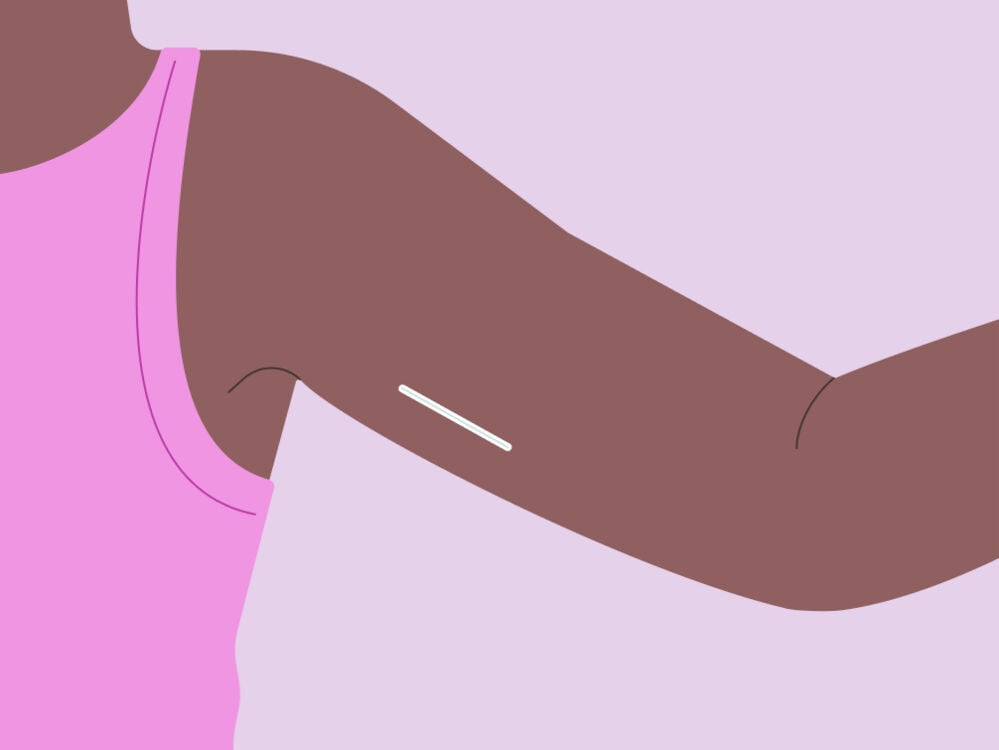
You might have heard about long-acting reversible contraception (LARC) or so-called “fit-and-forget” methods of birth control. If you don’t want to have to remember to take a pill every day, then this could be the method for you. They still need to be changed once in a while, though, so you can’t forget entirely!
The implant is a type of LARC. It’s a little plastic rod that’s about the size of a matchstick. “It is inserted into the skin of the upper arm,” Dr. Boyle explains. “It is a progestin-only method and does not contain any estrogen.”
Once the implant is in your arm, you’re 99% protected from unplanned pregnancy for, Dr. Boyle explains, “up to three years of use, but medical studies show it works for even longer.”
She adds, “A lot of people love it because it is so convenient, easy to use, and effective. It’s important to note that if people have issues with the implant, the usual problem is irregular bleeding.” That means your periods could become less frequent or stop completely.
If you’re interested in the implant, then you’ll need to book an appointment with your health care provider to have one inserted or removed. And remember, the implant doesn’t protect against sexually transmitted infections, so be sure to use condoms if you or a partner hasn’t had a recent sexual health checkup.
Birth control injection
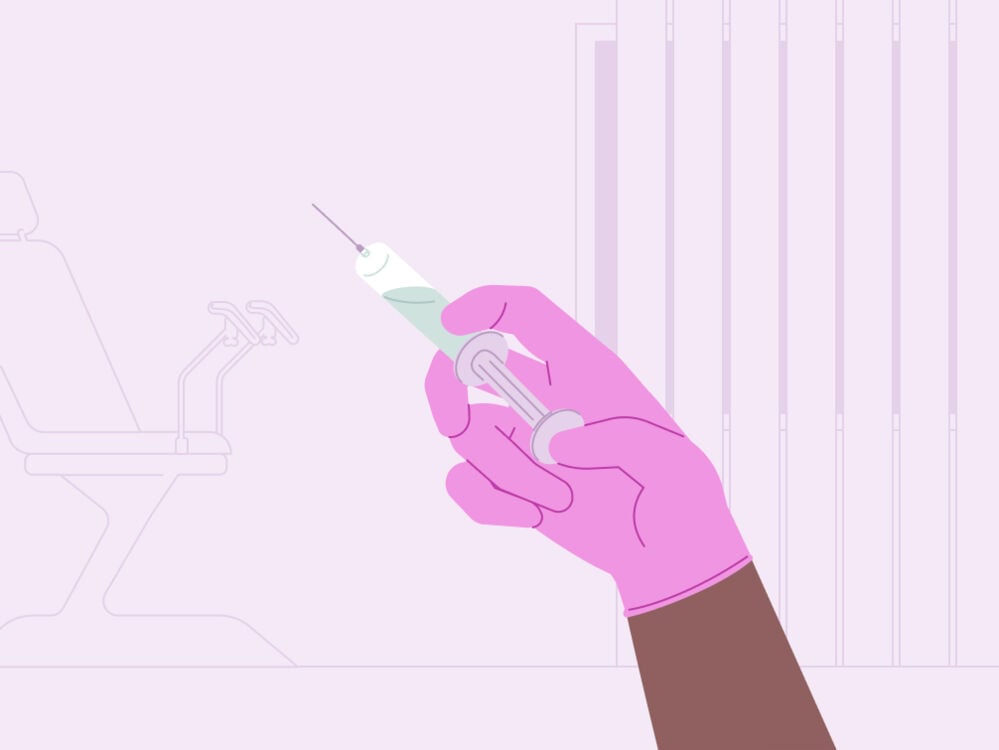
“Injectable birth control releases a progestin and is given about every 12 weeks,” Dr. Boyle explains.
Like the implant, the injection is a good option if you don’t always remember to take a pill each day. And it’s 96% effective at preventing pregnancy. But there are some potential early side effects to be aware of.
“It can cause irregular bleeding or spotting in the beginning,” Dr. Boyle says. “But this usually goes away after the first three to six months of use. Then it is very common for a person to not have any bleeding at all.”
Contraceptive patch or vaginal ring

If you’re looking for hormonal birth control that you can insert at home, then the patch or ring could be a good fit for you. “The contraceptive ring and patch contain both estrogen and progestin as well,” says Dr. Boyle. “They are just like COCs but have a different delivery system. Instead of taking a pill every day, you would place a ring in the vagina or place a patch on your skin.”
How does that work in practice? The ring is a small, plastic circle. You insert the tip of it into your vagina by squeezing it (with clean hands) and then push it up and inside until it feels comfortable. The ring then remains inside you for 21 days (three weeks), before you remove it for a seven-day break.
You’re protected from pregnancy the whole time thanks to the hormones the ring releases (estrogen and progestin). They stop your ovaries from releasing an egg.
The contraceptive patch is small with a sticky side that can be attached to your skin and is worn for seven days. During this time, it releases a daily dose of estrogen and progestin into the bloodstream (like the ring and the combined pill) to stop ovulation.
Both the contraceptive patch and vaginal ring are more than 99% effective when used correctly. However, this drops to 93% with imperfect use — for example if you don’t insert your ring or patch correctly or at the right time during your cycle.
IUD with progestin
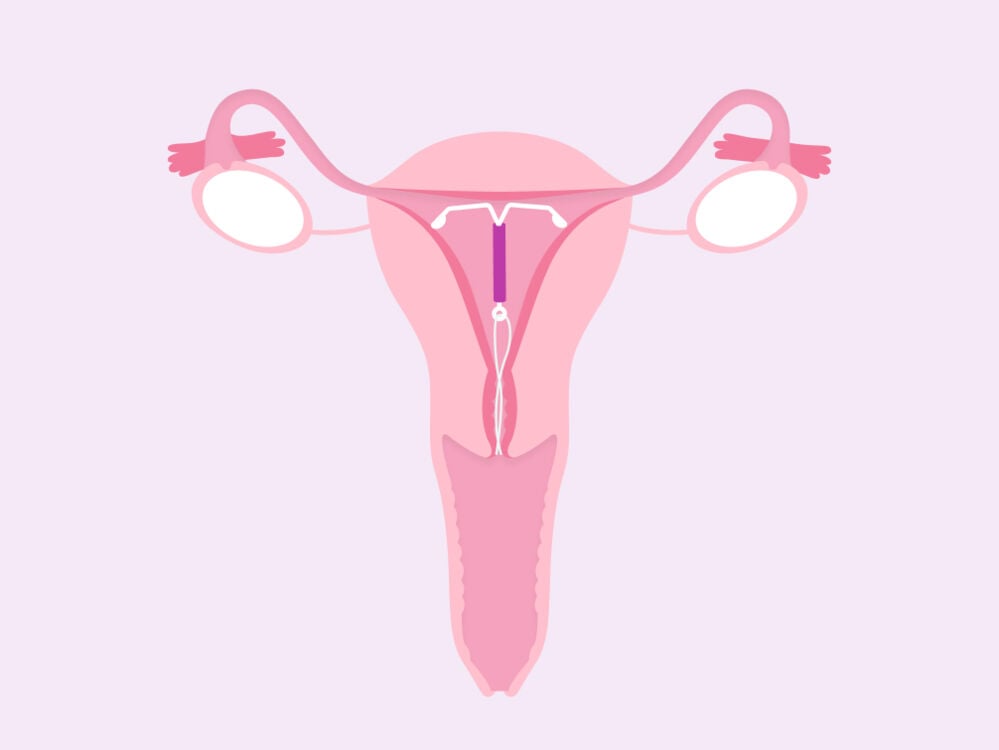
If your doctor recommends progestin-only forms of birth control, then you may be interested in the hormonal intrauterine device (IUD).
“Progestin-releasing IUDs are different from the other progestin-only methods of birth control such as the implant, the injection, and the POPs,” explains Dr. Boyle.
They’re more than 99% effective at preventing pregnancy and “are estrogen-free, so in that way they are similar, but the IUDs release progestin just in the uterus. They have a localized effect.
This means it has a very, very low chance of causing any of what we call systemic side effects, such as changes in mood, headaches, acne, breast tenderness, weight gain, etc.”
Side effects of hormonal contraceptives
It’s very typical for medication to come with some side effects. You’re introducing something new to your body after all. However, Dr. Boyle points out, “Side effects can be both good and bad.” Some “good” side effects of COCs, for example, can include:
- Lighter and less painful periods
- Less chance of developing ovarian cysts
- Reduced risk of ovarian and uterine cancer
- Clearer skin
- Fewer premenstrual syndrome (PMS) symptoms
- Less anemia (low iron, which can be caused by heavy bleeding)
Not all side effects are good though. Some people report:
- Nausea
- Tender breasts
- Headaches
- Irregular bleeding or spotting
In most cases, these will settle down after the first two to three months. If they don’t, don’t hesitate to reach out to your doctor.
Take a quiz
Find out what you can do with our Health Assistant
Birth control and weight gain: Are they linked?
You might have heard rumors that taking hormonal birth control is linked to weight gain. However, “Many medical studies have been done to investigate this, and COCs do not cause weight gain,” says Dr. Boyle.
For example, one study found that it is very unlikely that hormonal contraceptives cause major weight gain. “Researchers compare women taking COCs with those taking a placebo, or they compare women taking one contraceptive with those taking another,” explains Dr. Boyle. “In both groups, some gain weight, some lose weight, and some stay the same. So you can gain weight while taking COCs, but COCs don’t make you gain weight.”
Birth control and mood: What’s the latest science?
Another concern you might have may be how hormonal birth control might impact your mood.
“This has also been investigated thoroughly, and we don’t think COCs cause mood problems,” Dr. Boyle says. “One study in the United States even found a lower rate of depression and suicide attempts among women who used COCs. A study from Denmark did find that people who used COCs were more likely to start an antidepressant than those who didn’t use COCs, but the difference was small.”
However, it should be noted that taking estrogen (which is found in COCs) is not advised for some people. That’s because, as Dr. Boyle explains, “It can increase the chance of having certain dangerous medical problems such as a stroke or forming a blood clot in blood vessels (deep venous thrombosis).”
"We don’t think COCs cause mood problems"
Your doctor will also ask about your lifestyle when talking to you about your birth control options. “People shouldn’t take estrogen if they have high blood pressure, have had a stroke before, have had deep venous thrombosis before, if they smoke and are over age 35, if they have certain types of migraines, or if they have certain types of lupus,” Dr. Boyle adds.
Reading a list of conditions like that can be really scary, but try not to worry. If any of the above applies to you, then your doctor will be able to talk to you about a safe method of contraception.
How to choose your birth control
So, now we know that there are many different hormonal birth control options. Lifestyle and medical history can also contribute to what’s best for you. So how do you find out which form of birth control is right?
“First, make sure there are no medical reasons to choose one method over another,” says Dr. Boyle. “This mainly relates to using an estrogen-containing method versus an estrogen-free method. People should talk with their clinicians about their health history and family history to see if there are any reasons why they should use only estrogen-free.
“After that, it is mainly about personal preference. Do you like the idea of taking a pill every day, knowing you can stop it anytime? Or do you worry you will forget to take it? Like the idea of the pill, but not the everyday dosing? Then the ring or patch might be great for you.”
A pros and cons list could help you make the final decision once you’ve consulted with your doctor.
More FAQs
What are the pros and cons of hormonal contraceptives?
Dr. Boyle explains:
- “IUDs and the birth control implant are the most effective methods, the easiest to use, and generally have high satisfaction rates, and people tend to continue to use them.
- “However, you have to see a medical provider both to have them placed and to have them removed.”
- The pill, patch, and ring don’t need to be inserted by your doctor, so they might feel more low-maintenance.
- If your periods tend to be heavy or painful, then you may want to think about a method of birth control that could make your period lighter or make it stop altogether.
How does hormonal birth control affect the menstrual cycle?
The impact on your menstrual cycle depends on the type of birth control you choose. But as Dr. Boyle explains, “In most cases, hormonal birth control causes a person not to ovulate and not have the hormonal changes that are associated with a menstrual cycle.”
However, this really depends on the type of birth control you take and also differs from person to person. If you have questions about how your birth control might impact your cycle, the best thing to do is speak to your doctor.
Is it bad to take hormonal birth control?
In a word: no. Discovering the right contraceptive option for you can be life changing. It may help you feel more confident and in control of your family planning. Or it may help you manage PMS symptoms. Choosing the right form of birth control is really personal to you, but you can talk through your options with your doctor. They’re there to help you figure out where to begin.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Abou-Ismail, Mouhamed Yazan, et al. “Estrogen and Thrombosis: A Bench to Bedside Review.” Thrombosis Research, vol. 192, Aug. 2020, pp. 40–51.
Ali, Moazzam, et al. “Extended Use up to 5 Years of the Etonogestrel-Releasing Subdermal Contraceptive Implant: Comparison to Levonorgestrel-Releasing Subdermal Implant.” Human Reproduction , vol. 31, no. 11, Nov. 2016, pp. 2491–98.
“Birth Control Pill: Types, Side Effects & Effectiveness.” Cleveland Clinic, https://my.clevelandclinic.org/health/treatments/3977-birth-control-the-pill. Accessed 14 Feb. 2024.
“Birth Control: Forms, Options, Risks & Effectiveness.” Cleveland Clinic, https://my.clevelandclinic.org/health/articles/11427-birth-control-options. Accessed 14 Feb. 2024.
“Breastfeeding and Birth Control.” Journal of Midwifery & Women’s Health, vol. 69, no. 1, Jan. 2024, pp. 171–72.
Combination Birth Control Pills. 13 Jan. 2023, https://www.mayoclinic.org/tests-procedures/combination-birth-control-pills/about/pac-20385282.
Contraception. 1 May 2023, https://www.cdc.gov/reproductivehealth/contraception/index.htm.
Daniels, Kimberly, and William D. Mosher. “Contraceptive Methods Women Have Ever Used: United States, 1982-2010.” National Health Statistics Reports, no. 62, Feb. 2013, pp. 1–15.
Depo-Provera (contraceptive Injection). 22 Feb. 2022, https://www.mayoclinic.org/tests-procedures/depo-provera/about/pac-20392204.
“Depo-Provera® (Birth Control Shot).” Cleveland Clinic, https://my.clevelandclinic.org/health/drugs/4086-depo-provera-birth-control-shot. Accessed 14 Feb. 2024.
Estrogen and Progestin (Vaginal Ring Contraceptives). https://medlineplus.gov/druginfo/meds/a604032.html. Accessed 14 Feb. 2024.
Family Planning/contraception Methods. https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception. Accessed 14 Feb. 2024.
“Fit & Forget Contraception.” Lets Talk About It, https://www.letstalkaboutit.nhs.uk/contraception/fit-forget-contraception/. Accessed 14 Feb. 2024.
Gallo, Maria F., et al. “Combination Contraceptives: Effects on Weight.” Cochrane Database of Systematic Reviews , vol. 2014, no. 1, Jan. 2014, p. CD003987.
Hormonal IUD (Mirena). 20 Aug. 2022, https://www.mayoclinic.org/tests-procedures/mirena/about/pac-20391354.
“Hormones.” Endocrine System, June 2001, https://medlineplus.gov/hormones.html.
Jeanmonod, Rebecca, et al. “Vaginal Bleeding.” StatPearls, StatPearls Publishing, 2023.
Kerns, Jennifer, and Philip Darney. “Vaginal Ring Contraception.” Contraception, vol. 83, no. 2, Feb. 2011, pp. 107–15.
Keyes, Katherine M., et al. “Association of Hormonal Contraceptive Use with Reduced Levels of Depressive Symptoms: A National Study of Sexually Active Women in the United States.” American Journal of Epidemiology, vol. 178, no. 9, Nov. 2013, pp. 1378–88.
Kuehn, B. “Birth Control Patch.” JAMA: The Journal of the American Medical Association, vol. 299, Feb. 2008, pp. 890–890.
“LARC (long-Acting Reversible Contraceptive): Overview.” Cleveland Clinic, https://my.clevelandclinic.org/health/treatments/23269-larc. Accessed 14 Feb. 2024.
Long-Acting Reversible Contraception (LARC): Intrauterine Device (IUD) and Implant. https://www.acog.org/womens-health/faqs/long-acting-reversible-contraception-iud-and-implant. Accessed 14 Feb. 2024.
Minipill (progestin-Only Birth Control Pill). 13 Jan. 2023, https://www.mayoclinic.org/tests-procedures/minipill/about/pac-20388306.
“Progestin.” Cleveland Clinic, https://my.clevelandclinic.org/health/treatments/24838-progestin. Accessed 14 Feb. 2024.
Reed, Beverly G., and Bruce R. Carr. The Normal Menstrual Cycle and the Control of Ovulation. MDText.com, Inc., 2018.
Skovlund, Charlotte Wessel, et al. “Association of Hormonal Contraception With Depression.” JAMA Psychiatry , vol. 73, no. 11, Nov. 2016, pp. 1154–62.
Zhang, Ping, et al. “Exploring the Relationship between Drug Side-Effects and Therapeutic Indications.” AMIA... Annual Symposium Proceedings / AMIA Symposium. AMIA Symposium, vol. 2013, Nov. 2013, pp. 1568–77.




