Although this pregnancy-related condition is rare, it’s always good to be aware.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
What is preeclampsia? Signs, symptoms, and treatment explained


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Pregnancy can be one of the most joyful experiences for a parent-to-be, but it’s not always smooth sailing all the way through. Unfortunately, complications such as preeclampsia do sometimes occur.
Preeclampsia is a condition that accounts for around 2% to 8% of all pregnancy-related complications, which means it’s pretty rare. Having said that, recent studies have found possible links between the recent COVID-19 pandemic and an increase in cases of preeclampsia. So, given it can pose a risk to both you and your baby, it’s helpful to be aware of the symptoms of preeclampsia.
With that in mind, we asked Dr. Gian Carlo Di Renzo, professor and chair of obstetrics and gynecology at the University of Perugia, Italy, to share everything it’s useful to know. From what preeclampsia actually is to risk factors, symptoms, and treatment, keep reading to find out more.
What is preeclampsia?
Preeclampsia is a pregnancy complication most often seen after the 20-week mark of pregnancy that can cause a number of health issues at the same time. The most common signs are high blood pressure, protein in your urine, and swollen legs, which is why all these things are regularly monitored in your prenatal appointments. Usually, preeclampsia will be picked up quite quickly, thanks to these tests.
In more severe cases, usually when left untreated, preeclampsia can lead to organ damage such as kidney disease, stroke, seizures known as “eclampsia,” HELLP syndrome (which can cause abdominal pain, exhaustion, vomiting, blurred vision, and swelling), or in a very worst-case scenario, death. Of course, this all sounds very scary. But rest assured: these situations really are the rarest ones. And mostly, cases of preeclampsia are mild. Anyone who’s diagnosed is monitored very carefully by health care professionals, so you’re in safe hands.
What causes preeclampsia?
It’s difficult to pinpoint a specific reason why preeclampsia develops, and as with many female health conditions, that’s because there’s still a lot more research that needs to be done. But the main theory as to why preeclampsia occurs is that there’s something wrong with the way the placenta develops and functions.
Let’s rewind for a moment. The placenta is the organ that develops in pregnancy to provide the fetus with all the oxygen and nutrients it needs to survive in the uterus. In order for the placenta to do its job, it needs to connect the baby to the mother’s supplies via a network of blood vessels. But in women or people who get preeclampsia, it’s thought that these blood vessels don’t develop properly, causing issues with how well blood is circulated. In turn, this can lead to the high blood pressure that preeclampsia is known for.
Risk factors for preeclampsia
If you’ve read this far, you’re probably keen to know how to prevent preeclampsia. But unfortunately, as with many pregnancy complications, there’s no real way to tell if anyone will experience it before it happens. There are, however, some factors that may give you a slightly higher chance of developing preeclampsia, so it’s useful to know if any of them are relevant to you. They include:
- Having diabetes (including Type 1, Type 2, or gestational diabetes)
- Having high blood pressure before and/or during pregnancy
- Having had kidney disease or an autoimmune condition (such as lupus) before pregnancy
- Having had preeclampsia in a previous pregnancy
- If it’s your first pregnancy with your current partner
- If it’s 10 years or more since a previous pregnancy
- Having had complications in a previous pregnancy
- Being over the age of 35
- Having a BMI of 35 or more
- Having a family history of preeclampsia
- Expecting more than one baby
If any of these are familiar, have a chat with your health care provider as soon as possible. Many of the factors listed above are very common in many pregnancies, so ticking any one or more of these boxes doesn’t necessarily mean you will go on to experience preeclampsia. But it’s worth speaking to your doctor because they may plan for some extra monitoring throughout your pregnancy or give you aspirin to reduce the chance of developing the condition, which will hopefully provide you with a bit more reassurance. Additionally, it’s also important to attend your prenatal visits and to be aware of the physical symptoms of preeclampsia so you can raise the alarm with your health care provider if you think you’re developing any. More on that is below.
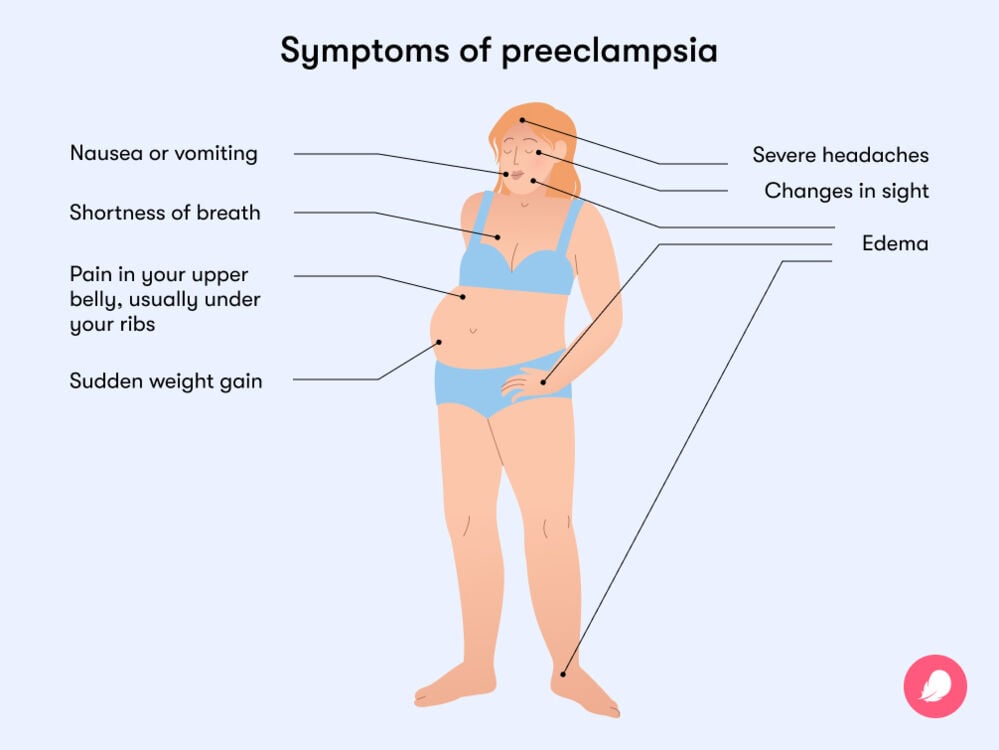
Symptoms of preeclampsia
There’s a good reason you’re given urine tests and blood pressure checks so regularly throughout pregnancy. As we now know, both high blood pressure and “proteinuria” (basically, protein in your pee) are the most common signs of preeclampsia. But they can easily pass unnoticed unless you’re specifically tested for them, which is why it’s important to attend all the appointments you’re invited to.
Some people may experience more overt symptoms of preeclampsia, though. Some of these symptoms may overlap with typical pregnancy symptoms. But as preeclampsia tends to strike later in pregnancy (the majority of cases occur between 30 and 35 weeks), you should see a health care professional if you think something unusual is happening. In particular, speak to a medical expert as soon as possible if you notice any of the following symptoms:
- Severe headaches
- Changes in sight (such as blurred or temporary loss of vision or light sensitivity)
- Shortness of breath
- Pain in your upper belly, usually under your ribs
- Sudden weight gain
- Edema (when tiny blood vessels in your body start to leak fluid, usually in your hands, arms, feet, ankles, and legs)
- Nausea or vomiting alongside any of the other symptoms
Sofie, 38, from the Cotswolds in the UK, was diagnosed with preeclampsia while in labor. The delayed diagnosis came because the only signs she experienced in the lead up were a little swelling and slightly raised blood pressure at around 34 weeks. “It was nothing drastic, so I was advised to just keep an eye on it.” At 38 weeks and five days, Sofie went into labor, which is when she was diagnosed with preeclampsia officially.
How does preeclampsia develop in pregnancy?
Often, just as Sofie experienced, preeclampsia has very few obvious symptoms. However, in a small number of preeclampsia cases, some people can become very unwell, which is more common when the diagnosis comes at an earlier stage of the pregnancy.
This is what happened to Abbie, 28, from Worcestershire in the UK. Abbie recalls noticing she had swollen hands and feet and a headache that wouldn’t go away after taking paracetamol at around 22 weeks into pregnancy. After raising concerns with her health care provider, Abbie was referred for tests and later diagnosed.
Troublingly, in these early diagnosis scenarios, the longer the baby stays in the uterus, the better the prospects are for them — but the more serious health implications it can have for you. “Preeclampsia can be mild or severe, and it’s a real balance between keeping the baby in and keeping both mother and child healthy,” says Abbie.
Preeclampsia treatment
Experts agree the only way to “cure” preeclampsia is to deliver the baby — even sometimes before you’re full term — as it can be safer that way. That’s not generally an issue if it’s detected in the later stages of pregnancy (as most cases are), as your health care provider can prescribe medication to help your baby’s lungs develop in time for an earlier birth. It also doesn’t mean you can’t still have a vaginal delivery, although a cesarean section may be recommended.
If preeclampsia is diagnosed earlier on, this can be slightly more complicated. However, as we now know, this is very uncommon. One study found that less than 1% of the women they assessed (who had never had preeclampsia before) delivered their babies before 34 weeks of pregnancy. So try not to worry too much about this happening. If this were to happen to you, you would be carefully monitored by your medical team, and every attempt would be made to prolong your pregnancy as long as it was safe. You may be given medication to lower your blood pressure (your doctor will discuss with you exactly what medication is needed), and in some cases, you may be brought into the hospital until your baby can be delivered.
For Sofie, her midlabor preeclampsia diagnosis meant she was unable to carry out her original birth plan, which had involved being in the birthing pool. “I wanted a water birth, so I initially got in the pool, but my blood pressure almost immediately started rising, so I had to come out again,” she says, adding that she was given medication to bring it back down.
Being in the middle of labor, Sofie wasn’t too fazed by the change of plans since she was more focused on delivering her baby in the safest way possible for them both. After a few more hours of contractions, Sofie welcomed a baby boy, Rafferty. They both stayed in the hospital for three days while her blood pressure came down before being sent home with two weeks’ worth of blood pressure medication.
" I had to relearn how to appreciate my body after preeclampsia. But I know there’s nothing I could have done differently"
Abbie, one of the less common cases where preeclampsia was diagnosed far earlier in her pregnancy, was taken into the hospital and monitored closely from there. “The baby was still kicking, and his heartbeat was fine. However, he was measuring a few weeks small,” Abbie tells Flo. “I was admitted into the hospital, given steroids to help his lung development, and attached to a drip to prevent seizures.”
Very sadly, it was decided that there was too much risk attached to Abbie continuing on with her pregnancy, and she was sent for an emergency cesarean section at 24 weeks and five days. Heartbreakingly, her son, Jude, passed away 32 days later.
It’s very important to remember that Abbie’s situation is one of the rare ones. Most people who are diagnosed with preeclampsia, just like Sofie, go on to have healthy babies and regain their own full health, too, as preeclampsia generally stops after labor, and blood pressure returns to normal. Despite this, it’s natural to feel overwhelmed if you’ve recently been diagnosed with preeclampsia, so make sure to lean on those around you. If you’re struggling and need some external support, reach out to organizations like the Preeclampsia Foundation in the US or Action on Pre-eclampsia in the UK.
Happily, Abbie went on to welcome a daughter — and she had an entirely healthy pregnancy the second time around. “She knows all about her big brother, Jude. He’s still in our lives,” says Abbie.
“It’s only when our bodies let us down that we criticize or question them. I had to relearn how to appreciate my body after preeclampsia. But being informed helps; logically, I know there’s nothing I could have done differently. I’d urge anyone with concerns to ask questions and to get checked, even if you feel silly. There’s never any harm in it.”


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Edema.” Mayo Clinic, 1 Dec. 2020, www.mayoclinic.org/diseases-conditions/edema/symptoms-causes/syc-20366493.
“Everything You Need to Know about Your Placenta.” Mayo Clinic, 3 Dec. 2022, www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/placenta/art-2004442.
“HELLP Syndrome.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21637-hellp-syndrome. Accessed 19 Dec. 2022.
Hernández-Díaz, Sonia, et al. “Risk of Pre-Eclampsia in First and Subsequent Pregnancies: Prospective Cohort Study.” BMJ, vol. 338, June 2009, p. b2255.
Karrar, Shahd A., and Peter L. Hong. “Preeclampsia.” StatPearls, StatPearls Publishing, 2022.
Khalil, A., et al. “Does COVID-19 Cause Pre-Eclampsia?” Ultrasound in Obstetrics & Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, vol. 59, no. 2, Feb. 2022, pp. 146–52.
“Low-Dose Aspirin Use during Pregnancy.” The American College of Obstetricians and Gynecologists. www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/07/low-dose-aspirin-use-during-pregnancy. Accessed 19 Dec. 2022.
Norwitz, Errol R. “Patient Education: Preeclampsia (Beyond the Basics).” UpToDate, 2021.
“Preeclampsia.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/17952-preeclampsia. Accessed 19 Dec. 2022.
“Preeclampsia.” Mayo Clinic, 15 Apr. 2022, www.mayoclinic.org/diseases-conditions/preeclampsia/symptoms-causes/syc-20355745.
“Pre-Eclampsia.” British Heart Foundation, www.bhf.org.uk/informationsupport/conditions/pre-eclampsia. Accessed 19 Dec. 2022.
“Preeclampsia.” March of Dimes. www.marchofdimes.org/find-support/topics/pregnancy/preeclampsia. Accessed 19 Dec. 2022.
“What Is Pre-Eclampsia and What Are the Warning Signs?” NHS, 2020, https://www.nhs.uk/conditions/pre-eclampsia/.

