Cramps during or just before a period are very common — almost everyone who has periods reports having menstrual pain. And that’s no exaggeration — studies have shown that anywhere from 16–91% of people who get periods have cramps, and they’re more common for people who are 20–24. Cramps that happen days or weeks after a period or at different times throughout the cycle can be normal, but they can also be a sign that something’s not right.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Cramps After Period: What It Could Mean


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
How long do period cramps last?
Cramps often begin just before a period starts. They can last for the whole period, but tend to be worse at the beginning and when the flow is heaviest. Most often, pain is felt in the lower abdomen and lower back, but it sometimes radiates to the thighs. Cramps can usually be improved with over-the-counter pain medication, exercise, and warm baths or hot water bottles.
Not everyone gets cramps, and some people have them for the first few years of having their period, and then they get better. Other people start out with pain-free periods and start getting cramps when they’re older. But a review of 15 studies conducted between 2002 and 2011 found that it’s more common for symptoms to decrease with age and after childbirth. The female reproductive system can be unpredictable!
Can you have menstrual cramps after your period?
In short, you can have some kind of menstruation cramps after a period, but it’s not common. Hormone-like substances in the body called prostaglandins are the main cause of menstrual cramps. Among other things, prostaglandins make the uterus contract. If these contractions are too strong, the muscles of the uterus don’t get enough oxygen, which causes pain. The uterus needs to contract to shed its lining — the endometrium. When this lining is shed, it comes out in the form of menstrual fluid (AKA your period), and the uterus is ready to start the cycle over again by building up a new lining. It’s normal for periods to sort of trail off and be followed by a day or two of “spotting” or darker discharge. While this is happening, it might cause cramps, but that’s pretty unusual.
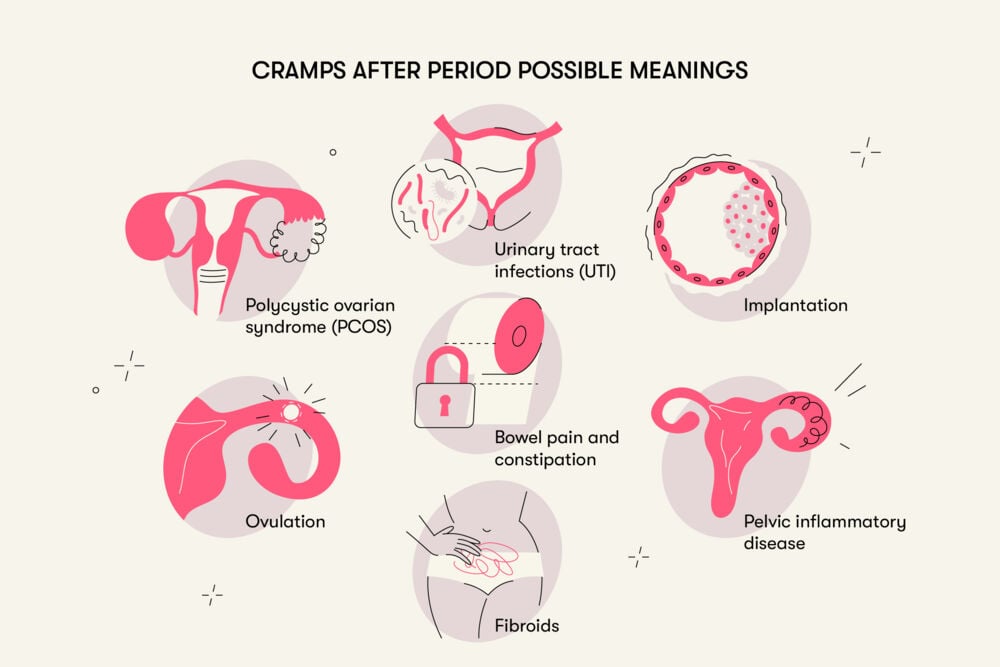
What could cramps after your period mean?
There are lots of different reasons someone might have period-type pains or lower abdominal cramps. But what can cramps not during a period mean?
Take a quiz
Find out what you can do with our Health Assistant
Ovulation: Ovulatory pain, or Mittelschmerz (German for middle pain), is quite common and affects more than 40% of people who get periods. Commonly, this pain appears after several years of getting periods. This pain is generally felt somewhere around the middle of the cycle, so someone with regular 28-day cycles might feel it around 14 days after their period started.
Not everyone has cramping or pain when they ovulate, and for those who do it usually doesn’t last very long. Often it only lasts a few minutes, but sometimes it’s a day or two. The pain can range from mild to severe, and it’s often on one side of the lower abdomen. This is because the pain is caused by a follicle in the ovary bursting to release an egg. People who have ovulation pain as a regular part of their cycle may get used to it and recognize it when it happens.
Implantation: If an egg is fertilized, the next step of this earliest stage of pregnancy is implantation. This is where the fertilized egg embeds into the soft uterine lining, triggering lots of changes in the uterus. Some — but not all — people have some cramping pain when this happens, and it can last up to a day or two.
Secondary dysmenorrhea: Dysmenorrhea is a blanket term for problems associated with periods. Secondary dysmenorrhea is what we call problems associated with the menstrual cycle that are not specifically related to menstruation. This term can cover conditions like fibroids, polyps, endometriosis, and other problems linked to the female reproductive system.
- Polycystic ovarian syndrome (PCOS): This is a condition where eggs form small cysts on the surface of the ovaries that aren’t released normally. Pain can be a secondary symptom of PCOS, particularly if it causes large cysts.
- Pelvic inflammatory disease (PID): This is a bacterial infection that can spread from the uterus to the uterine tubes and ovaries, and it can cause extremely serious illness. Symptoms can include lower abdominal pain, abnormal discharge or bleeding, and general flu-like illness.
- Fibroids: These are benign (non-cancerous) growths around or within the uterus that can cause cramping pains, as well as bloating, heavy periods, and constipation.
- IUD: Although this side effect is rare, it is one of the reasons people stop using IUDs for birth control. IUD pain is most often due to coil displacement.
Sometimes lower tummy pain that might feel a bit like period cramps is caused by something unrelated to the reproductive system.
Bowel pain and constipation can cause lower abdominal pain and tenderness. A study conducted in 2012 with more than 180,000 participants (both male and female) found that 14% of women had bowel pain or constipation, but it tended to get better after age 50. Another study — this one conducted in Brazil in 2020 — found that of the 195 women who participated, 34.5% had constipation.
Urinary tract infections can cause lower abdominal, pelvic, and back pain too. A study of more than 1,000 women conducted in Uzbekistan in 2020 found that about 9% of reproductive-age participants had a UTI at some point during the course of the study.
What can I do about cramping after my period?
Period pain is really common, and it can usually be treated at home. Cramping after a period is less common, but it often responds to the same treatment that regular period cramps do. However, managing the pain at home doesn’t mean you can’t consult a health care provider if you think that something is wrong.
What you can do yourself:
- Self-acupressure — A study conducted in 2011 with the participation of Iranian medical sciences students showed that self-massage had a positive effect for three hours afterwards.
- Physical exercise (including yoga and pilates) — The data from the results of 23 studies that involved 2,302 women showed the effectiveness of these methods. Low-intensity exercise and stretching was found to be significantly helpful in the group that didn’t take any medication. It was also moderately effective in the group of people who took ibuprofen for their pain. So either way, it could help!
- Warm baths or heat packs — Warmth relaxes the muscles of the abdomen and reduces spasms to relieve pain. Heat also improves blood circulation, reduces fluid retention, and relieves tension from constricted nerves. A 2007 study in Turkey of 193 women showed that heat on the lower abdomen had the same effectiveness of a single dose of analgesic medication.
- Simple over-the-counter pain medication — Medications like acetaminophen (paracetamol) or ibuprofen often help.
Some people find that exercise helps to relieve the cramps, even if it feels like the last thing you want to do at the time! Warm baths or heat packs can also help a lot. Make sure that any heat packs or hot water bottles are well wrapped so you don’t get burned. If these simple remedies don’t help the pain, or if you find that you’re regularly missing school, work, or daily life because of period-related problems, make sure to see a health care provider.
You know your body better than anyone, so you can tell when something is wrong. If something feels off to you or you have ongoing pain with no clear cause, unmanageable pain, or excessive bleeding, see your health care provider right away.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.




