We know they’re not much fun, but let’s dive into what causes menstrual cramps to learn how best to manage them.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Everything You Need to Know About Period Cramps


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Period cramps, known in the medical world as “dysmenorrhea,” are a very common and normal part of the monthly cycle. Though the experience has been around for as long as humans have, the word “dysmenorrhea” was first used in 1810, created using New Latin word parts that basically mean “difficult menstrual flow.” It’s estimated more than half of us experience period pain for one or two days each month.
It’s important to understand that menstrual pain exists on a scale and varies significantly from person to person. Some don’t experience any period pain at all, for others it’s light cramping, but for around 10 percent it’s so severe that it gets in the way of everyday life.
Let’s dive into what causes period cramps and how best to relieve them.
Take a quiz
Find out what you can do with our Health Assistant
What causes period cramps? And why am I cramping so badly?
Menstrual cramps usually feel like a throbbing, cramping, or dull ache in the lower abdomen and back. The pain often comes on just before your period starts and can last throughout. For some, symptoms can also include diarrhea, nausea, vomiting, and headaches. So what causes these cramps in the first place?
Well, it’s pretty simple, really. Dysmenorrhea describes the pain often associated with menstruation, and there are two types: primary dysmenorrhea and secondary dysmenorrhea.
Primary dysmenorrhea is caused by hormone-like chemicals produced in your uterus called “prostaglandins.” They help it to contract in order to shed the lining (AKA your period).
You may also experience secondary dysmenorrhea. However, this pain is caused by other gynecologic conditions such as endometriosis, adenomyosis, or fibroids. Of these, the most common is endometriosis — a painful condition where tissue similar to uterine lining grows in the tubes and ovaries. This tissue also breaks down and bleeds as hormones change, but it can sometimes become trapped, and, in some cases, painful scar tissue can form.
Secondary dysmenorrhea typically lasts longer than regular menstrual cramps. Pain can begin a few days before your period starts, and it sometimes intensifies over time.
If you’re concerned about your period pain, it’s a good idea to make an appointment with your doctor or health care professional. If necessary, they can run some tests that might put your mind at ease or recommend treatment that could help.
Why are some people more prone to period cramps?
From length to heaviness and cramps, everyone has a different experience when it comes to periods.
“Some people do have more painful periods than others, and this may be due to a buildup of prostaglandins, which can cause stronger contractions,” Caroline Overton, consultant gynecologist and spokesperson for the Royal College of Obstetricians and Gynaecologists, tells Flo.
However, there are some factors that can put you at a higher risk of painful periods.
Research by the University of Queensland found that you are much more likely to experience painful period cramps if you have a family history of dysmenorrhea. Lifestyle factors also seem to be at play here too — their research also found that stress was closely associated with dysmenorrhea.
Another study from the same university found that women who smoke may be more likely to experience menstrual pain. The link between the two is not exactly clear, but it could be related to a reduced amount of oxygen available to the uterus.
Why are my cramps so bad this month?
Ever noticed your cramps sometimes vary from month to month? It could have something to do with fluctuating hormone levels, Overton says.
“Each month marks the start of a new process of hormone production from the ovaries,” she explains. “Estrogen is the dominant hormone before ovulation, and progesterone becomes the dominant hormone after ovulation.” So it’s natural for pain and symptoms to vary from one cycle to the next as levels of these hormones fluctuate.
Periods can change as you get older, too. “For example, in your 40s, it is common for periods to become heavier and closer together as you approach perimenopause, due to the natural age-related hormonal changes that occur during this time,” Overton says.
Again, if you’re experiencing a change in your periods and/or struggling with symptoms, it’s best to speak to your doctor or health care professional for advice and support.
What can make period pain worse?
Maintaining a healthy weight may be important for managing period pain. Research from the University of Queensland found that both underweight and overweight people who menstruate were more likely to experience painful period cramps.
“Diet can affect periods, and in some cases those who are significantly underweight can see their periods stop altogether,” says Overton. “Stress can also impact the length of a woman’s cycle, and sometimes stop periods altogether.”
The good news is there are a number of things you can do to help support your monthly cycle. Eating a balanced healthy diet rich in healthy fats like oily fish, nuts, and seeds, as well as plenty of fruit and vegetables may ease the pain you have around your period. However, a study published by the European Journal of Obstetrics & Gynecology and Reproductive Biology has highlighted that your diet doesn’t necessarily make period cramps any worse.
Drink plenty of water and, as ever, consume alcohol and caffeine in moderation. “If your periods are very heavy, it might be worth taking an iron supplement during your period to replace the iron being lost with the period blood,” Overton says. Consult a medical professional to find out if that’s the right course of action for you. They’ll be able to advise you on the right dose and whether you need blood tests.
Make exercise a part of your weekly routine, too. Exercise releases endorphins, also known as feel-good or happy hormones, which can help with stress management — but that doesn’t have to be at the gym. “Many people don’t feel like exercising during a painful period, but keeping active can help relieve pain and discomfort,” Overton says.
Try something low impact like swimming, cycling, or taking a lunchtime walk instead. Most importantly, listen to your body and do what feels right for you — if you feel like powering through a HIIT class, that’s fine too.

What are the best ways to relieve period cramps?
“Period pain can usually be relieved by taking simple over-the-counter painkillers, such as paracetamol [acetaminophen], and this can be combined with non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen,” Overton says.
NSAIDs work by reducing the production of prostaglandins. They work best when taken one to two days before your period starts. Additionally, using a hot water bottle or heating pad can be very effective at relieving the pain.
Give yourself enough time to rest and try to do some (gentle) exercise. This could be a good time to indulge in some self-care, too. Try taking a relaxing hot bath or practicing relaxation techniques like meditation or mindfulness.
“Anyone experiencing pain that is not relieved by simple painkillers and interferes with their daily lives and activities, like having days off work or school, should speak to a healthcare professional, as this might be a symptom of other conditions,” explains Overton.
You may be prescribed oral contraceptives to help with long-term management of painful period cramps — they can also help reduce the amount of prostaglandins produced. If you’ve tried using over-the-counter medication to manage your pain, you might be prescribed stronger NSAIDs, such as diclofenac, etodolac, fenoprofen, and flurbiprofen.

How much period pain is normal? And what should you do if your cramps suddenly get worse?
Remember, everyone’s cycle is different, so what might be normal for you might not be normal for someone else. The bottom line is, period cramps shouldn’t significantly affect your day-to-day life.
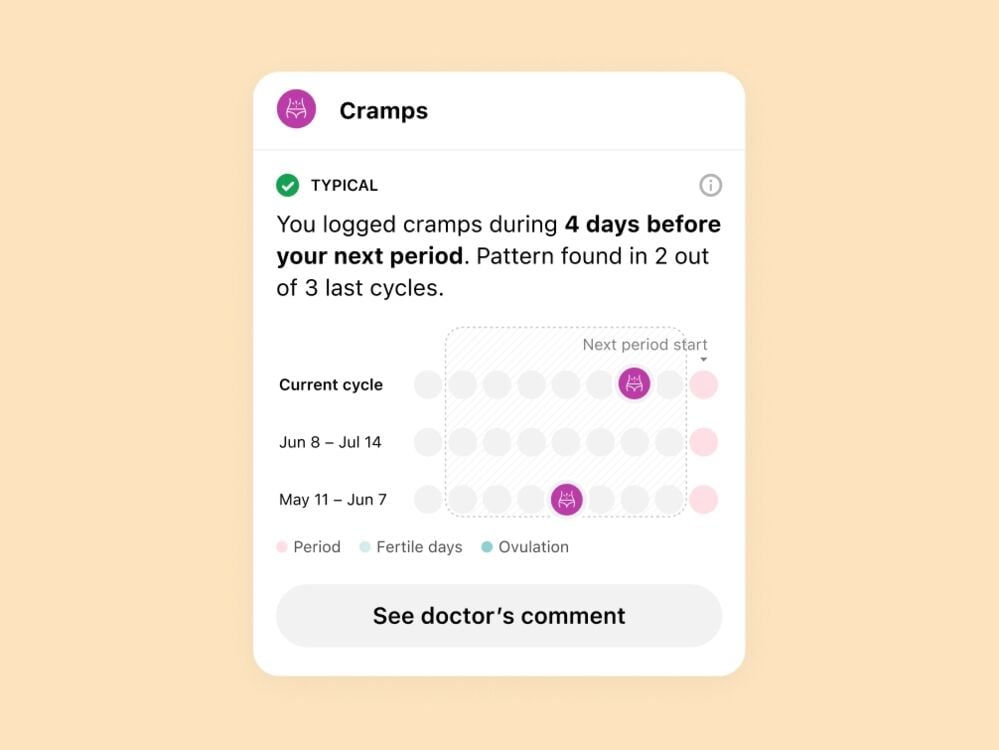
Keeping track of your symptoms with a period tracking app like Flo can be really useful for making sense of your cycle. You can also have your history of symptoms at-hand when you speak to your doctor or health care professional.
Period cramps: The takeaway
Period cramps vary significantly from person to person, depending on your menstrual cycle, and they can be impacted by a variety of lifestyle factors. Following a healthy diet and exercising regularly are good practices for maintaining an overall sense of well-being, but pain shouldn’t be regularly getting in the way of your everyday life.
If you’re concerned about period cramps, or you’ve noticed a change in the severity of pain, it’s a good idea to speak to a doctor, just to be sure about what’s going on for you.
The good news is treatment for both primary and secondary dysmenorrhea is available, so you don’t have to deal with it on your own.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Mariette. “Period Pain - Women’s Health Concern.” Women’s Health Concern, 15 Dec. 2020, www.womens-health-concern.org/help-and-advice/factsheets/period-pain. Accessed 11 Nov. 2021.
“Dysmenorrhea: Painful Periods.” ACOG, www.acog.org/womens-health/faqs/dysmenorrhea-painful-periods#:%7E:text=Dysmenorrhea%3A%20Discomfort%20and%20pain%20during,tubes%2C%20and%20other%20pelvic%20structures. Accessed 11 Nov. 2021.
“How Does Dysmenorrhea Affect Daily Life?” Medscape, 27 Aug. 2020, www.medscape.com/answers/253812-55117/how-does-dysmenorrhea-affect-daily-life. Accessed 11 Nov. 2021.
Osayande, Amimi S., and Suarna Mehulic. “Diagnosis and Initial Management of Dysmenorrhea.” American Family Physician, vol. 89, no. 5, 2014, pp. 341–46. American Family Physician, www.aafp.org/afp/2014/0301/p341.html. Accessed 11 Nov. 2021.
“Dysmenorrhea.” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/dysmenorrhea. Accessed 11 Nov. 2021.
“The Prevalence and Risk Factors of Dysmenorrhea.” Oxford Academic Epidemiologic Reviews, academic.oup.com/epirev/article/36/1/104/566554. Accessed 11 Nov. 2021.
Ju, Hong. “Smoking and Trajectories of Dysmenorrhoea among Young Australian Women.” Tobacco Control, tobaccocontrol.bmj.com/content/25/2/195. Accessed 11 Nov. 2021.
“A U-Shaped Relationship Between Body Mass Index and Dysmenorrhea: A Longitudinal Study.” NCBI, pubmed.ncbi.nlm.nih.gov/26218569. Accessed 11 Nov. 2021.
Balbi, Carlo, et al. “Influence of Menstrual Factors and Dietary Habits on Menstrual Pain in Adolescence Age.” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 91, no. 2, 2000, pp. 143–48. Crossref, doi:10.1016/s0301-2115(99)00277-8. Accessed 11 Nov. 2021.
Speer, Linda. “Dysmenorrhea.” American Family Physician, 15 Jan. 2005, www.aafp.org/afp/2005/0115/p285.html.




