Gynecological cancer describes cancers that start in the cervix, uterus, vulva, vagina, or ovaries. Symptoms and treatment options for each of these cancers can look pretty different. Here, an OB-GYN outlines what you need to know about the different gynecological cancers.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
5 main types of gynecological cancer: What you should know

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.

If you or someone you know is going through a difficult time, remember that there are ways to get help. Here are some support services and resources in your country.
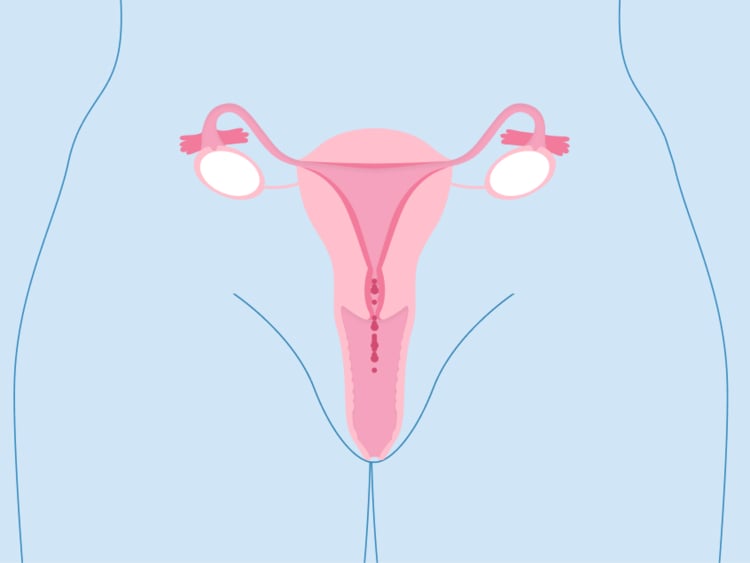
Find out moreGynecological cancer is the broad term that describes all of the cancers that start in the female reproductive organs. These include the cervix, uterus, vulva, vagina, and ovaries. Depending on where the cancer starts, symptoms can look pretty different.
“Most cancers in the body do not develop in the same way or along the same timeline. There are no screening tests for ovarian, uterine, vaginal, and vulva cancer, so it is important to pay attention to your body,” says OB-GYN (obstetrician and gynecologist) Dr. Barbara Levy. “If you are experiencing new symptoms, you should report them to your health care professional.”
It’s estimated that there will be around 115,130 new cases of gynecological cancer diagnosed in the US in 2022. Changes to your reproductive health can be scary, but it’s important to remember that you’re not alone. Your health care provider is there to answer any questions or concerns you may have.
Here, Dr. Levy explains the signs and symptoms associated with the five main types of gynecological cancer and what tests are available for detecting them so you know what to expect.
Cervical cancer: Signs and diagnosis
Cervical cancer describes any cancer that starts in the cervix — the thin neck that connects your vagina to your uterus. The American Cancer Society estimates that in 2022, 14,100 new cases of invasive cervical cancer will be diagnosed. Nearly all cervical cancers are caused by an infection from certain types of human papillomavirus (HPV).
HPV is the name for more than 100 different types of virus. It’s passed through skin-to-skin genital contact during vaginal, anal, or oral sex. Most people will contract HPV at some point in their lives, but don’t worry — most cases are harmless and clear naturally.
Symptoms of cervical cancer can include:
- Vaginal bleeding between periods or after sex
- Pain during sex
- Pain in your lower back or abdomen
- Changes in your vaginal discharge
If you start to notice these symptoms, then don’t panic. They can be linked to a whole range of other conditions (that have nothing to do with cancer), and the best thing to do is reach out to your medical professional to get to the bottom of what’s going on.
If you’re 21 years old in the US or 25 in the UK, then it’s likely that you’ll have been invited for your first Pap smear. Cervical cancer is the only gynecological cancer that can be prevented through screenings. “Cervical screenings can find changes in cells that happen years before cancer develops,” says Dr. Levy. “Those changes are easy to treat, and when treated in a timely fashion, they will never progress to cancer.” That’s why it’s so important to make sure you attend these appointments when you’re invited for them.
During your screening, your health care provider will insert a speculum (a medical device that looks a bit like a duck’s beak) into your vulva. They will then insert a swab to collect some cells from the cervix. The whole process is very quick — usually less than five minutes.
It can be uncomfortable, but it shouldn’t hurt. If you have any concerns about pain, talk to your medical professional. They may use a smaller instrument or find another alternative for you. Results can take a few weeks to process, and if your test shows any abnormalities, then your medical practitioner may invite you back for a colposcopy.
During a colposcopy, your health care provider will insert a speculum into your vagina again. They will then look at your cervix and vagina with a microscope with a light on the end. They may take a small sample of cells to be tested in a laboratory. This test should take no longer than 30 minutes.
Attending your Pap smear and any follow-up tests is really crucial, but it’s totally normal to feel nervous. There’s no need to be embarrassed. If you have any worries, then speak to your health care provider before the appointment. They will be able to walk you through the procedure and answer any of your questions.
Ovarian cancer: Signs and diagnosis
Ovarian cancer develops in the glands that hold and release eggs for fertilization, on either side of the uterus. In 2022, it’s estimated that around 19,880 people in the US will receive a new diagnosis of ovarian cancer. Ovarian cancer is often diagnosed in the later stages (stages 3 and 4).
“We used to say that there are no signs of ovarian cancer, but research has suggested that new onset of abdominal bloating, pelvic pressure, and fullness is present in a large percentage of people with ovarian cancer,” says Dr. Levy. If you notice any new symptoms or if symptoms become persistent, then reach out to your medical professional.
Other symptoms of ovarian cancer can include:
- Pain in your belly or pelvis
- Not feeling hungry or getting full very quickly
- Needing to urinate more often
- Unexplained weight loss
- Back pain
- Constipation or diarrhea
Many of these symptoms are incredibly common and can be linked to other conditions, like irritable bowel syndrome (IBS). If you already have a condition, like IBS, that can cause bloating and pain and you notice a difference or worsening in your symptoms, then try not to panic. Reach out to your health care provider for advice.
They may conduct a pelvic exam where they feel your ovaries and uterus for size, shape, and consistency by pressing down on your abdomen. They may also take some blood for testing. Further tests might include an ultrasound and a transvaginal scan (where a finger-sized device is inserted into the vagina).
Uterine cancer: Signs and diagnosis
Uterine cancer affects the uterus — the part of the reproductive system where a fertilized egg can grow into a baby. “Abnormal bleeding is an early sign of uterine cancer, predominantly in women after menopause,” says Dr. Levy. It’s the most common of the five gynecological cancers, and the American Cancer Society estimates that 65,950 new cases will be diagnosed in the US in 2022.
Other symptoms of uterine cancer include:
- Unusually heavy periods
- Bleeding between periods
- A change in discharge
- Pain after sex
- A lump in the belly or pelvis
Your cycle will differ from that of your loved ones, so the keyword here is “unusual.” If you experience anything that doesn’t feel right, it’s a good idea to get it checked out. And you can monitor any changes to your period and cycle by using Flo’s tracker.
Your health care provider will take a medical history from you. They may ask you about your normal cycle lengths and what your period is typically like. They may also conduct a pelvic exam to feel for any changes in your uterus. Following that, you may be referred to a specialist for more tests, which could be an ultrasound or transvaginal scan, a blood test, or a biopsy.

Vaginal cancer: Signs and diagnosis
The vagina is the tube that connects your vulva to your uterus. Vaginal cancer is very rare. In 2019, 1,368 women were diagnosed with it in the United States.
Symptoms of vaginal cancer can include:
- Lumps, ulcers, or other skin changes in the vagina
- Bleeding after sex when you’re not on your period
- Bleeding between periods
- Needing to urinate more often
- Longer, heavier periods
Changes in your cycle and irregular bleeding can indicate hormone fluctuations or heightened stress levels. So try not to worry if you’ve identified some changes. Your health care provider should be able to support you and advise you on what to do next.
“Vaginal cancer may be picked up during cervical cancer screening since the swabs to pick up cervical cells will pick up vaginal cells as well,” says Dr. Levy. Tests for vaginal cancer involve looking inside the vagina, and your health care provider may recommend a colposcopy.
Vulvar cancer: Signs and diagnosis
Vulvar cancer can affect your external genitals — your labia, clitoris, and glands. “Vulvar cancer is a skin cancer. There will be growths, itching, or sores on the skin,” says Dr. Levy. It accounts for 6% of diagnoses of cancer in the female reproductive organs, and it’s estimated that there will be 6,330 new diagnoses in the US in 2022.
You may be more susceptible to experiencing vulvar cancer if you’re over 50, if you have a strain of HPV, or if you smoke. It’s a rare form of cancer, making up just 0.6% of cancer cases in women in the US.
Symptoms of vulvar cancer include:
- Itching, pain, soreness, or tenderness in the vulva
- Changes to the consistency or color of the skin around your vulva
- Lumps or growths around your vulva
- Irregular bleeding or spotting between periods
- Blood in your discharge
- A burning sensation when you urinate
- New moles or changes to preexisting moles or birthmarks around your vulva
Noticing changes in your reproductive health can be scary, but it’s so important to know that your health care provider is there to answer any of your questions or worries. Your OB-GYN may take a full medical history from you before conducting an external examination. They will look for any changes to the skin around your vulva and may take a sample of cells to be examined in a laboratory.
If the results of your biopsy highlight that the cells may be cancerous, then your medical professional may conduct a colposcopy. They may also offer you a CT or MRI scan.
"If you are anxious or nervous discussing gynecological problems, write down your questions and concerns and bring the list to your appointment.”
Treatment for gynecological cancer
Your treatment options for gynecological cancer can vary depending on which kind of gynecological cancer you have and at what stage it’s detected. It’s totally normal to feel daunted by the prospect of treatment, so it could be helpful to bring a loved one to your appointment. They can provide support and ask questions on your behalf.
Treatments may be used separately or alongside one another.
- Surgery: Your health care provider may remove the cancerous tissue during an operation. This is generally only offered if the cancer is in its earlier stages and hasn’t spread.
- Chemotherapy: Your medical professional may advise a course of chemotherapy. Medicines are offered in the form of a drip or pills to kill or shrink the cancerous cells.
- Hormone therapy: This is when hormones or hormone-blocking drugs are used to shrink and treat cancer.
Your health care provider should include you in every conversation about your treatment plan, give you space to ask questions about any side effects, and outline how treatment may fit into your wider lifestyle and plans to have a family.
5 main types of gynecological cancer: The takeaway
Cervical cancer is currently the only gynecological cancer that can be detected and prevented through screening. That’s why attending your Pap smear and logging any changes in your reproductive health is so crucial.
“Pay attention to your body. Sudden, unique symptoms should be reported to your doctor,” says Dr. Levy, especially if you notice they’re not going away. “If you are anxious or nervous discussing gynecological problems, write down your questions and concerns and bring the list to your appointment.” Your health care provider should give you the space to discuss your symptoms and verbalize any worries you have.
Catching cancer early makes it easier to treat so you can have the best possible outcome. If you do find yourself going through a cancer diagnosis, it’s important to remember that you’re not alone. Organizations like the Foundation for Women’s Cancer in the US and The Eve Appeal in the UK are dedicated to supporting people who have been diagnosed with gynecological cancers and their loved ones, so make sure you find the support you need.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Cancer Facts and Figures 2022.” American Cancer Society, https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf. Accessed 6 July 2022.
“Basic Information About Ovarian Cancer.” Centers for Disease Control and Prevention, 30 Mar. 2022, https://www.cdc.gov/cancer/ovarian/basic_info/index.htm. Accessed 6 July 2022.
“Key Statistics for Cervical Cancer.” American Cancer Society, https://www.cancer.org/cancer/cervical-cancer/about/key-statistics.html. Accessed 6 July 2022.
“What Is a Colposcopy?” NHS, https://www.nhs.uk/conditions/colposcopy/. Accessed 6 July 2022.
Dilley, James, et al. “Ovarian Cancer Symptoms, Routes to Diagnosis and Survival - Population Cohort Study in the ‘No Screen’ Arm of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS).” Gynecologic Oncology, vol. 158, no. 2, Aug. 2020, pp. 316–22. Accessed 6 July 2022.
“Human Papillomavirus (HPV).” NHS, https://www.nhs.uk/conditions/human-papilloma-virus-hpv/. Accessed 6 July 2022.
“Key Statistics for Endometrial Cancer.” American Cancer Society, https://www.cancer.org/cancer/endometrial-cancer/about/key-statistics.html. Accessed 6 July 2022.
“Key Statistics for Vulvar Cancer.” American Cancer Society, https://www.cancer.org/cancer/vulvar-cancer/about/key-statistics.html. Accessed 6 July 2022.
“Symptoms: Ovarian Cancer.” NHS, https://www.nhs.uk/conditions/ovarian-cancer/symptoms/. Accessed 6 July 2022.
“Tests and Next Steps: Ovarian Cancer.” NHS, https://www.nhs.uk/conditions/ovarian-cancer/tests-and-next-steps/. Accessed 6 July 2022.
“Key Statistics for Ovarian Cancer.” American Cancer Society, https://www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html. Accessed 6 July 2022.
Proietto, Anthony. “Gynaecological Cancer Surgery.” Best Practice & Research. Clinical Obstetrics & Gynaecology, vol. 20, no. 1, Feb. 2006, pp. 157–72. Accessed 6 July 2022.
Reed, Nicholas S., and Azmat H. Sadozye. “Update on Chemotherapy in Gynaecological Cancers.” The Obstetrician & Gynaecologist, vol. 18, no. 3, July 2016, pp. 182–88. Accessed 6 July 2022.
“Signs and Symptoms of Ovarian Cancer.” American Cancer Society, https://www.cancer.org/cancer/ovarian-cancer/detection-diagnosis-staging/signs-and-symptoms.html. Accessed 6 July 2022.
“Signs and Symptoms of Vaginal Cancer.” American Cancer Society, https://www.cancer.org/cancer/vaginal-cancer/detection-diagnosis-staging/signs-symptoms.html. Accessed 6 July 2022.
“Signs and Symptoms of Vulvar Cancers and Pre-Cancers.” American Cancer Society, https://www.cancer.org/cancer/vulvar-cancer/detection-diagnosis-staging/signs-symptoms.html. Accessed 6 July 2022.
Sjoquist, Katrin M., et al. “The Role of Hormonal Therapy in Gynecological Cancers: Current Status and Future Directions.” International Journal of Gynecological Cancer, vol. 21, no. 7, Oct. 2011, pp. 1328–33. Accessed 6 July 2022.
“Genital HPV Infection: Basic Fact Sheet.” Centers for Disease Control and Prevention, 8 June 2022, https://www.cdc.gov/std/hpv/stdfact-hpv.htm. Accessed 6 July 2022.
“Symptoms: Cervical Cancer.” NHS, https://www.nhs.uk/conditions/cervical-cancer/symptoms/. Accessed 6 July 2022.
“Tests for Ovarian Cancer.” American Cancer Society, https://www.cancer.org/cancer/ovarian-cancer/detection-diagnosis-staging/how-diagnosed.html. Accessed 6 July 2022.
“Uterine Cancer.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/16409-uterine-cancer. Accessed 6 July 2022.
“Vaginal and Vulvar Cancers Statistics.” Centers for Disease Control and Prevention, 1 June 2022, https://www.cdc.gov/cancer/vagvulv/statistics/index.htm. Accessed 6 July 2022.
“Vaginal Cancer.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/15579-vaginal-cancer. Accessed 6 July 2022.
“Overview: Vulval Cancer.” NHS, https://www.nhs.uk/conditions/vulval-cancer/. Accessed 6 July 2022.
“Diagnosis: Vulval Cancer.” NHS, https://www.nhs.uk/conditions/vulval-cancer/diagnosis/. Accessed 6 July 2022.
“Vulvar Cancer.” Johns Hopkins Medicine, 8 Aug. 2021, https://www.hopkinsmedicine.org/health/conditions-and-diseases/vulvar-cancer. Accessed 6 July 2022.
“Overview: Womb (Uterus) Cancer.” NHS, https://www.nhs.uk/conditions/womb-cancer/. Accessed 6 July 2022.
“Symptoms: Womb (Uterus) Cancer.” NHS, https://www.nhs.uk/conditions/womb-cancer/symptoms/. Accessed 6 July 2022.

