Follow our step-by-step guide to checking your cervix to increase your chance of pregnancy.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
How to find (and check) your cervix

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
When you’re trying to conceive (TTC), it’s easy to become a little obsessive looking for tips for getting pregnant. Luckily, from tracking ovulation to monitoring your basal body temperature, there are plenty of ways you can maximize your chances of getting pregnant every month.
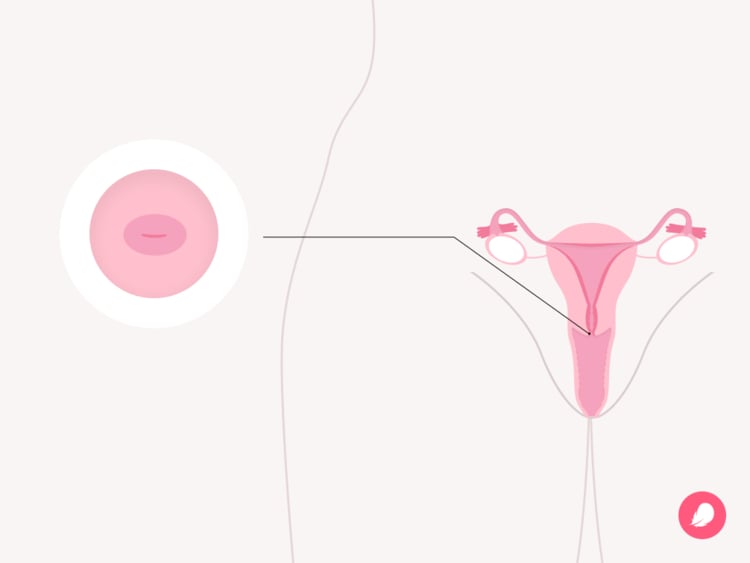
Using an ovulation-tracking app like Flo is a great way to better understand how your menstrual cycle works. But you might not realize that your body also gives off subtle clues every month that can give you a head start. It’s a little-known fact that your cervix — the small, donut-shaped canal that connects your uterus to your vagina — actually changes position throughout your menstrual cycle.
Admittedly, your cervix is located pretty deep inside your body, so it’s not visible to the human eye. That means other methods of ovulation tracking (such as keeping an eye on the way your cervical mucus changes or monitoring your temperature) are recommended as easier ways to keep track of what’s going on inside. But if you know what to feel for, learning how to check the location and texture of your cervix can also help you figure out where you are in your cycle. And being able to pinpoint your fertile window could potentially increase your chance of becoming pregnant.
Here, obstetrician and gynecologist Dr. Sara Twogood, Cedars-Sinai Medical Group, California, US, shares everything you need to know about how to check your cervix. But if you have any questions or concerns about anything to do with your reproductive health, always reach out to your doctor for advice.
Key takeaways
- Your cervix changes position and texture a number of times throughout your menstrual cycle.
- Learning how to track these changes can be one way to give you some important clues about your fertile window, the six days of each cycle in which you could conceive.
- If you think you might be pregnant, ask your doctor for advice before you examine yourself. Self-checks are not recommended during pregnancy.
What is your cervix?
If you’re not sure what or where your cervix is, don’t worry. You’re not the only one, and it’s possible to get pregnant without fully understanding how every part of your reproductive system works. But because extra knowledge can’t hurt, it may be helpful to know that your cervix is a tube-shaped organ located at the bottom of your uterus. And it plays an important role in your ability to get pregnant and carry a baby.
“The cervix is often called the neck of the uterus,” explains Dr. Twogood. “It’s the connecting organ from the vagina to the uterus.” But it’s much more than just a tube. As well as providing an exit point for fluids such as period blood and mucus (which you’ll know as your discharge) to pass through, it has other jobs. This multitasking organ protects your uterus by preventing objects such as tampons, diaphragms, or sex toys from entering you any further. It also helps sperm cells travel from your vagina through to your uterus for pregnancy, thanks to cervical mucus.
Your cervix plays a central role in childbirth, too. During pregnancy, it forms a mucus plug that stops bacteria and infection from reaching your baby. And when the time comes, contractions cause your cervix to open (dilate) so your baby can move down the birth canal and make their way into the world.
Why does your cervix change position during your cycle?
Are you trying to conceive or simply curious about your body? It takes time and patience to check your cervix, but charting its movements throughout the month can give you some important clues about where you are in your cycle and your fertile window. “The cervix changes both position and texture during the menstrual cycle,” says Dr. Twogood. “This is related to the different hormones at play at different times in the cycle.”
You won’t feel it happening, but your shifting cervix is designed to encourage pregnancy. “[It changes] to help get sperm into the uterus and uterine tubes to optimize the chances of getting pregnant,” explains Dr. Twogood.
So, how exactly does it adjust? Let’s run through all the cervical changes that happen throughout your cycle.
Cervical position during your period
On day one of your cycle — when your period starts — your cervix moves downward, helping the blood to flow out. “During your period, the cervix is lower in the vagina/pelvis,” explains Dr. Twogood. It may also be “slightly firm and open to allow blood to exit from the uterus into the vagina and then out of the body altogether,” she explains.
Cervical position during ovulation
Your cervix will then move back up just before ovulation into a prime position for conception. If you have an average 28-day menstrual cycle, this might happen about 14 days before the start of your next period. “During ovulation, the cervix is soft and higher in the vagina and pelvis,” says Dr. Twogood. “The cervical os (the opening to the cervix) is more open to allow sperm easier access into the uterus and uterine tubes.”
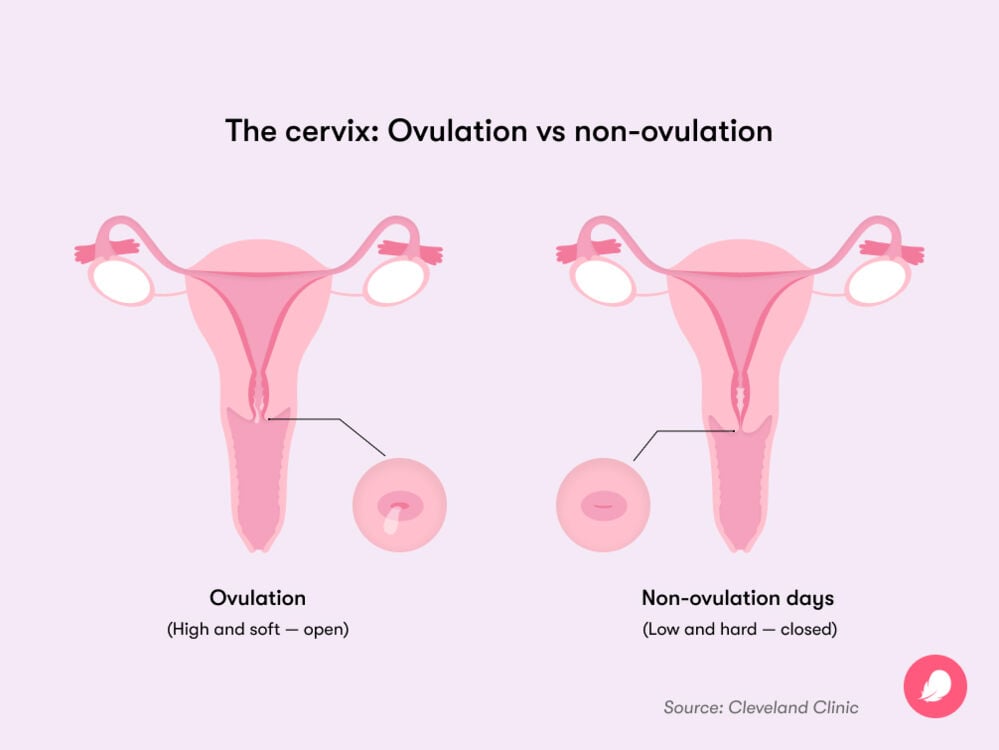
Cervical position after ovulation
Your cervix usually drops back down again once ovulation is complete in order to start the cycle again, explains Dr. Twogood. By this stage, it might feel firmer and drier, and the opening to your uterus might become tightly closed.
Why you might have your cervix checked by a doctor
As we know, checking your cervix yourself is one way to keep track of where you are in your cycle (although you might prefer to follow other, more obvious methods, like keeping an eye on your cervical mucus). But having your cervix checked by a health care professional is also a routine procedure for a number of possible reasons:
- A cervical screening, also known as a Pap test or smear, is important for checking the health of your cervix and to help prevent cervical cancer. It’s offered to women and people with a cervix at some point in your 20s, roughly every three to five years, depending on where you live. This is not something that you can do yourself, so reach out to your doctor if you want to find out more about getting a Pap.
- Your doctor might check your cervix during late pregnancy to find out if you’re dilated or if your body is preparing for labor with a softer cervix, says Dr. Twogood.
- Your health care professional will also check your cervix to see how things are progressing during labor. “When labor symptoms are present or suspected (like painful contractions), checking the cervix can help know how far along someone is in labor,” says Dr. Twogood.
Take a quiz
Find out what you can do with our Health Assistant
How to check your cervix (a step-by-step guide)
If you’re trying to conceive, you might choose to check your cervix regularly to track your ovulation. It takes time and patience to check your cervix, and you’ll need to do it for at least a couple of months to spot any subtle changes throughout your menstrual cycle. It’s also worth keeping a record so it’s easier to monitor your findings.
Wash your hands
To get started, make sure that your hands are clean to prevent the spread of bacteria. “First, wash your hands with soap and water,” advises Dr. Twogood. You may also want to trim your nails to prevent scratches while feeling for your cervix.
Check your timing
If you’re sexually aroused, it can be harder to check your cervix. Your vagina tends to relax and open during sexual excitement, lifting your cervix farther away from your vaginal opening and making it difficult to reach. For best results, don’t try to check your cervix immediately after or during sex.
Get into a comfortable position
It’s much easier to check your cervix if you’re comfortable, so choose a quiet spot where you won’t be disturbed and experiment with different positions. You might find that standing or kneeling (similar to when you insert a tampon) will help you find the spot.
Lubricate
If you’re not used to penetration or you feel at all uncomfortable, it’s fine to use lubrication such as products that are used for sex, says Dr. Twogood.
Insert your finger into your vagina
Take a few deep breaths, try to relax, and start slowly. “Place one to two fingers inside the vagina and keep going until something that feels like a ball or a different consistency is felt,” says Dr. Twogood.
Feel your cervix
The cervix will feel firm to touch or just slightly different to the rest of the skin inside your vagina, explains Dr. Twogood. And if you can’t feel anything at all, take your time. “Sometimes, people have to go deeper than they expect or go to one side more than the other — this is all normal! It’s usually about the firmness of the cartilage on the tip of the nose,” she adds.
Try again
Can’t find it or not sure what you’re feeling? It often takes practice. Keep in mind that it may be more difficult to locate your cervix, depending on where you are in your cycle. Trying again will help you to compare at different points in your cycle.
Take notes
Make a note of the location and feel of your cervix throughout your menstrual cycle. It may also help to record the consistency of your cervical mucus, which you’ll notice in your undies. This changes in texture, volume, and color, depending on where you are in your cycle. Over time, spotting patterns in these changes may help you to better understand your fertile window and when you will be most likely to get pregnant.
Get to know your body and prepare for getting pregnant
While there’s never a guarantee when you’re trying to get pregnant, getting to know the different ovulation-tracking methods is a good place to start. Learning about your cycle and the signs of ovulation using an app like Flo can help reassure you that you’re doing the right things at the right time to get pregnant.
But don’t forget to pay attention to how you feel. Trying to conceive for any length of time can take its toll on your emotions. If you’re finding things difficult, remember that many of us have been through it too, and you are not alone. Try sharing how you feel with your loved ones or chat with like-minded people on Flo’s safe Secret Chats space about what you’re going through.
Frequently asked questions about checking your cervix
How do you know if you’re touching your cervix?
Learning how to check your cervix is a process of trial and error, as the location and texture of your cervix can change depending on where you are in your cycle. After inserting your finger into your vagina, once you reach a barrier that prevents you from going any further, this is your cervix. If you’re still not sure, as a general rule, remember “it feels different than the rest of the vagina,” says Dr. Twogood.
Can you tell you’re pregnant by checking your cervix?
You can’t reliably tell if you’re pregnant by touching your cervix, says Dr. Twogood. “It’s rare for people to use cervical checking as their primary way of tracking their menstrual cycle,” she explains. “There are other more reliable ways to know about an early pregnancy, such as a late period and a home pregnancy test.”
What’s done during a pelvic exam?
A pelvic exam is a routine examination carried out by your health care professional to check for any unusual changes in your pelvic organs. Your doctor will gently insert a gloved finger or two into your vagina to check for abnormalities and then examine your uterus and ovaries by touching your abdomen with their other hand. This exam shouldn’t be painful, though it may be a little uncomfortable. If you are feeling pain during this exam, let your health care professional know right away. And if you have any concerns, make sure to ask — there are no silly questions.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Cervical Mucus.” Cleveland Clinic, https://my.clevelandclinic.org/health/body/21957-cervical-mucus. Accessed 20 July 2022.
“Cervix.” Cleveland Clinic, https://my.clevelandclinic.org/health/body/23279-cervix. Accessed 21 Aug. 2024.
Hilz, Max J. and Ruihao Wang. “Physiology and Pathophysiology of Female Sexual Function.” Primer on the Autonomic Nervous System (Fourth Edition), edited by Italo Biaggioni, et al. Academic Press, 2023, pp. 247–52.
“Mucus Plug.” Cleveland Clinic, https://my.clevelandclinic.org/health/symptoms/21606-mucus-plug. Accessed 25 Sep. 2024.
“Ovulation.” Cleveland Clinic, https://my.clevelandclinic.org/health/articles/23439-ovulation. Accessed 17 Feb. 2023.
“Pelvic Exam.” Cleveland Clinic, https://my.clevelandclinic.org/health/diagnostics/17343-pelvic-exam. Accessed 25 Sep. 2024.
“Pregnancy Tests.” Cleveland Clinic, my.clevelandclinic.org/health/diagnostics/9703-pregnancy-tests. Accessed 8 Oct. 2024.
“Stages of Labor and Birth: Baby, It’s Time!” Mayo Clinic, 23 July 2024, www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/stages-of-labor/art-20046545.
“Symptoms of Pregnancy: What Happens First.” Mayo Clinic, 13 Mar. 2024, www.mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/symptoms-of-pregnancy/art-20043853.
Witt, Barry. “Trying to Get Pregnant? Here’s When to Have Sex.” The American College of Obstetricians and Gynecologists, Aug. 2023, www.acog.org/womens-health/experts-and-stories/the-latest/trying-to-get-pregnant-heres-when-to-have-sex.




