The terms are often used interchangeably, but menopause and perimenopause are actually two separate things. Here’s how to tell the difference.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Perimenopause vs menopause: What’s the difference?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Have you started having hot flashes, brain fog, or trouble sleeping and noticed a change to your cycles? It may not be on your radar yet, but if you’re somewhere between your late 30s and your 50s and you notice any of these symptoms, it could be the first step on your journey toward menopause, also known as perimenopause.
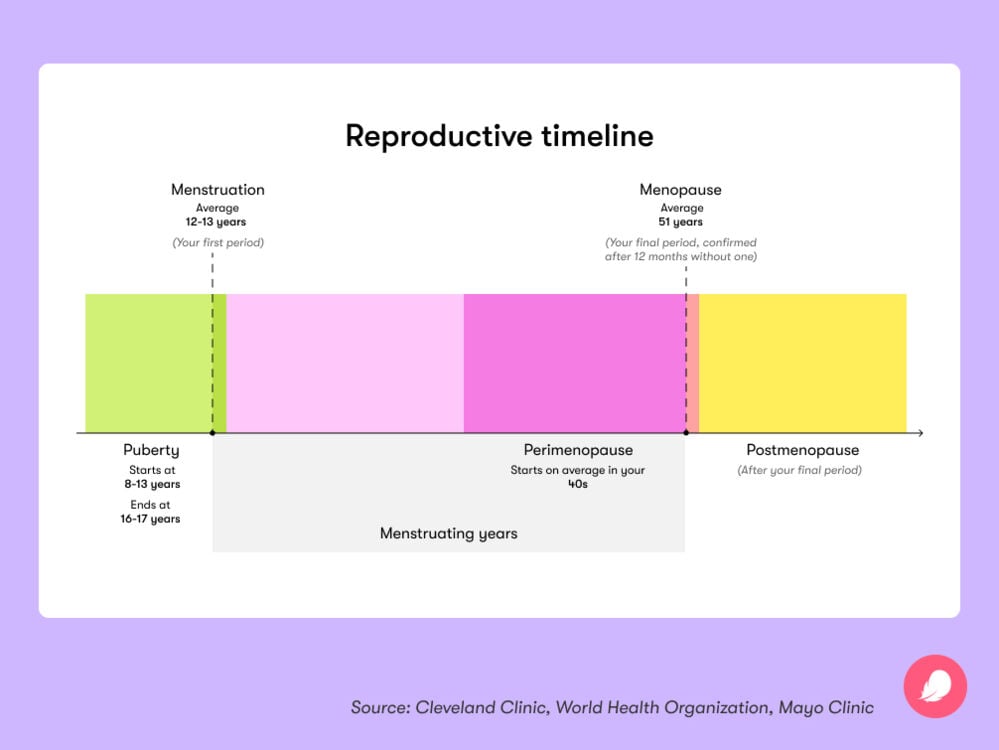
You might be familiar with the idea that having no period for a year means you’ve reached menopause. But did you know there can be other signals during the transition to menopause? In fact, symptoms can begin four to eight years before your periods stop altogether, thanks to gradual changes to your hormones.
Of course, these unusual symptoms might be caused by reasons other than perimenopause. Brain fog or difficulty sleeping could be due to premenstrual syndrome (PMS), for example, or hot flashes could be caused by thyroid disease. But perimenopause and, later, menopause is something everyone with a female reproductive system will go through, so it’s worth understanding what goes on. As always, if you have any questions or concerns about any health issue, always reach out to your doctor for a checkup.
Key takeaways
- Perimenopause refers to the years leading up to menopause. It can start any time between your late 30s and your 50s.
- You’re classed as having gone through menopause when you haven’t had a period for 12 months.
- Perimenopause symptoms can include changes to your periods, hot flashes, night sweats, mood swings, brain fog, and sleep problems.
- Some people have difficulty with symptoms, while others don’t, but many treatment options can help, so don’t lose hope.
What’s the difference between perimenopause and menopause?
Confusingly, the two terms are often used as one and the same thing, but perimenopause and menopause are two different things.
“Perimenopause is the several years leading up to menopause where hormone changes can cause symptoms,” explains Dr. Allison K. Rodgers, reproductive endocrinologist, obstetrician, and gynecologist, Fertility Centers of Illinois, US.
During this time, your periods might start to get closer together or further apart, they could become heavier or lighter, and you might notice other symptoms, including hot flashes, night sweats, and mood swings.
After a year without a period, you have gone through menopause, signaling the end of your menstrual cycle for good. “The definition of menopause is one year without a period,” explains Dr. Rodgers.
When is menopause likely to happen?
The life stage of transitioning into menopause — aka perimenopause — can begin anywhere between your late 30s and 50s, but it most often happens in your 40s. Your experience of perimenopause will be unique, but it can last a while. “Perimenopause can last a long time, often several years,” says Dr. Rodgers. The average time is four years, but it can last up to eight years.
You’re diagnosed as having gone through menopause when you haven’t had a period for 12 months, and this usually happens between the ages of 45 and 55. From then on, you are postmenopausal. “The average age of menopause is 51 years old,” says Dr. Rodgers. “However, there can be a lot of variability from person to person as to when that last period comes.”
Take a quiz
Find out what you can do with our Health Assistant
It can be hard to keep track of irregular periods and other symptoms when you’re going through perimenopause. That’s where Flo can help. In the app, you can log symptoms like hot flashes and mood swings alongside tracking your periods. You’ll then get a cycle report each month so you can understand your body better.
What are the symptoms of perimenopause?
Everyone is unique when it comes to perimenopause, so no two people have the exact same symptoms. Because we have hormone receptors in lots of places in our bodies, this perimenopausal change in estrogen levels can affect us anywhere from head to toe. How intense it is and how long it can last also differs from person to person, meaning some have trouble dealing with their symptoms, while others don’t.
If you recognize any of the following signs of perimenopause and feel you need support, reach out to your doctor, who can discuss treatment options with you. Remember, you don’t have to put up with it.
Irregular cycles
According to Dr. Rodgers, one of the first signs of perimenopause is a shortening of your cycle. “This happens because you are ovulating earlier in your cycle,” she explains. If you are someone who always had 28-day cycles, ovulating on day 14, you may notice that you start ovulating earlier and earlier. So you could start ovulating around day 10 and have a 24-day cycle.”
Hot flashes
Hot flashes are a common perimenopause symptom. If you get them, you’ll probably be familiar with the sudden, uncomfortable episodes of intense heat around your head, neck, chest, or upper back. Palpitations, sweating, and reddening of the skin are often noticed, too. Hot flashes, also known as vasomotor symptoms (VMS), are such a common symptom, in fact, that more than 80% of women will experience them, at some point during perimenopause or postmenopause. “Hot flashes and night sweats typically start right around or before the period but extend to other times of the cycle as perimenopause gets closer to menopause,” says Dr. Rodgers.
Sleep disturbances
Disrupted sleep is also common in perimenopause. You might struggle to drift off, or you might wake up and find it hard to settle. Perhaps unsurprisingly, research has also found a direct link between VMS at night — also known as night sweats — and sleep disturbances. If you wake up in the night burning up, it’s easy to see why this might disturb your sleep.
Dry skin
You may have already been warned about one unwelcome perimenopause symptom that many people experience: vaginal dryness. And thanks to declining hormones, your skin and eyes can also dry out during perimenopause.
Brain fog
If it feels like you’ve been sleepwalking through life lately, you’re not alone. According to research, between 41% and 44% of women experience some degree of memory problems during the menopause transition. If you notice a lack of focus, forgetfulness, and difficulty concentrating, perimenopause brain fog could be to blame.
Mood swings
Are you feeling tearful or cranky, but your period isn’t due anytime soon? About four in 10 women have mood disturbances during perimenopause. Think of it as similar to PMS, with symptoms including irritability and mood swings. If you’re generally not feeling like yourself, it may well be due to perimenopause.
How to treat symptoms during perimenopause
Perimenopause is a natural transition toward the end of your years of ovulating, and fluctuating hormones are a normal part of the process. However, if the resulting symptoms are causing some disruption to your life, then it’s important to seek out ways to help.
A number of treatment options are available to help you feel like yourself again. These differ according to which symptoms you’re experiencing and how severe they are. Some of the main perimenopause treatment options include:
- Hormone therapy: Also known as hormone replacement therapy or HRT, this is considered to be the most effective treatment for hot flashes, night sweats, and vaginal dryness. “Hormonal treatments typically include estrogen, which can be given by pills, vaginal rings or inserts, or skin patches,” explains Dr. Rodgers.
- Antidepressants: Certain antidepressants typically used to treat mood disorders are another option to help with hot flashes and night sweats if you can’t take estrogen. “Nonhormonal options can include selective serotonin receptor inhibitors (SSRIs) which can reduce symptoms,” says Dr. Rodgers.
- Birth control: If you’re already using combined hormonal contraceptive pills (not the progesterone-only ones), then your doctor might tell you to keep taking them in the early stages of perimenopause. They can help to steady your fluctuating hormone levels, which in turn may help to dial down perimenopause symptoms.
- Vaginal moisturizer: Regularly applying this inside your vagina can help to encourage its walls to make more natural lubrication, providing relief from vaginal dryness.
- Vaginal lubes: If you experience pain during sex, using lube is a great way to stop the discomfort from mild to moderate vaginal dryness and chafing.
- Lifestyle changes: For many people, simple lifestyle changes can help with symptoms. “I recommend regular exercise, good sleep hygiene, and yoga or meditation,” says Dr. Rodgers. “I also recommend limiting caffeine, alcohol, and [quitting] tobacco.”
- Keep cool: Struggling with VMS? “If you suffer from night sweats and hot flashes, you can dress in layers and sleep with your window open or with a fan to avoid overheating at night,” adds Dr. Rodgers.
If you’d like to explore treatments for your symptoms, reach out to your doctor. They can offer advice to help you decide which option is best for you. Chatting with like-minded people in the Secret Chats forums on the Flo app may also offer useful support because it’s always helpful to remember you’re not the only one going through it.
More FAQs
What makes perimenopause worse?
Experts aren’t entirely sure why some people experience perimenopause symptoms more intensely than others. Everyone is unique, and we all react differently to hormones. If you are concerned, speak to your doctor for support and advice.
Will your hot flashes stop after menopause?
Most people stop having hot flashes within a few years of their last period, according to Dr. Rodgers. “For others, it can last longer,” she says. The good news is they usually become less severe as time goes on.
“If you are on estrogen treatment, when you stop it, you will have hot flashes because of the withdrawal from the estrogen,” adds Rodgers. How long these symptoms last will depend on the person taking it. If you’re thinking about stopping hormone therapy, it’s recommended that you gradually reduce your dose to minimize withdrawal rather than stopping suddenly.
How long does postmenopause last?
You’re diagnosed as having gone through menopause when you haven’t had a period for 12 months. From then on, you are postmenopausal for the rest of your life. This means that you’ll no longer have a monthly period, and you will no longer be able to get pregnant naturally because your ovaries will have stopped releasing eggs.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Abraham, Cynthia. “Experiencing Vaginal Dryness? Here’s What You Need to Know.” The American College of Obstetricians and Gynecologists, Oct. 2020, www.acog.org/womens-health/experts-and-stories/the-latest/experiencing-vaginal-dryness-heres-what-you-need-to-know.
Augoulea, Areti, et al. “Psychosomatic and Vasomotor Symptom Changes during Transition to Menopause.” Menopause Review, vol. 18, no. 2, June 2019, pp. 110–15.
Baker, Fiona C., et al. “Sleep and Sleep Disorders in the Menopausal Transition.” Sleep Medicine Clinics, vol. 13, no. 3, Sep. 2018, pp. 443–56, https://doi.org/10.1016/j.jsmc.2018.04.011.
Bansal, Ramandeep, and Neelam Aggarwal. “Menopausal Hot Flashes: A Concise Review.” Journal of Mid-Life Health, vol. 10, no. 1, Jan.–Mar. 2019, pp. 6–13, DOI: 10.4103/jmh.JMH_7_19.
Chen, Peng, et al. “Role of Estrogen Receptors in Health and Disease.” Frontiers in Endocrinology, vol. 13, 18 Aug. 2022, p. 839005, www.ncbi.nlm.nih.gov/pmc/articles/PMC9433670/.
Conde, Délio Marques, et al. “Menopause and Cognitive Impairment: A Narrative Review of Current Knowledge.” World Journal of Psychiatry, vol. 11, no. 8, Aug. 2021, pp. 412–28, DOI: 10.5498/wjp.v11.i8.412.
Coslov, Nina, et al. “‘Not Feeling like Myself’ in Perimenopause: What Does It Mean? Observations from the Women Living Better Survey.” Menopause, vol. 31, no. 5, 25 May 2024, pp. 390–98, pubmed.ncbi.nlm.nih.gov/38531011/.
Delamater, Lara, and Nanette Santoro. “Management of the Perimenopause.” Clinical Obstetrics and Gynecology, vol. 61, no. 3, Sep. 2018, pp. 419–32, DOI: 10.1097/GRF.0000000000000389.
“Hot Flashes.” Cleveland Clinic, my.clevelandclinic.org/health/articles/15223-hot-flashes. Accessed 11 June 2024.
“Hot Flashes.” Mayo Clinic, 12 Dec. 2023, www.mayoclinic.org/diseases-conditions/hot-flashes/symptoms-causes/syc-20352790.
Martin, Kathryn A., and Robert L. Barbieri. “Treatment of Menopausal Symptoms with Hormone Therapy.” UpToDate, 20 Nov. 2023, www.uptodate.com/contents/treatment-of-menopausal-symptoms-with-hormone-therapy.
“Menopause 101: A Primer for the Perimenopausal.” The North American Menopause Society, www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal. Accessed 11 June 2024.
“Menopause: Symptoms.” NHS, www.nhs.uk/conditions/menopause/symptoms/. Accessed 11 June 2024.
“Menopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/menopause/symptoms-causes/syc-20353397.
“Menopause.” World Health Organization, 17 Oct. 2022, www.who.int/news-room/fact-sheets/detail/menopause.
Penckofer, Sue, et al. “Does Glycemic Variability Impact Mood and Quality of Life?” Diabetes Technology and Therapeutics, vol. 14, no. 4, Apr. 2012, pp. 303–10, https://doi.org/10.1089/dia.2011.0191.
“Perimenopausal Bleeding and Bleeding after Menopause.” The American College of Obstetricians and Gynecologists, Oct. 2020, www.acog.org/womens-health/faqs/perimenopausal-bleeding-and-bleeding-after-menopause.
“Perimenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21608-perimenopause. Accessed 11 June 2024.
“Perimenopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666.
Pinkerton, Joann V. “Menopause.” MSD Manual Consumer Version, July 2023, www.msdmanuals.com/en-gb/home/women-s-health-issues/menopause/menopause.
“Postmenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21837-postmenopause. Accessed 11 June 2024.
Potter, N., and N. Panay. “Vaginal Lubricants and Moisturizers: A Review into Use, Efficacy, and Safety.” Climacteric, vol. 24, no. 1, Feb. 2021, pp. 19–24, doi: 10.1080/13697137.2020.1820478.
“Premenstrual Syndrome (PMS).” Mayo Clinic, 25 Feb. 2022, www.mayoclinic.org/diseases-conditions/premenstrual-syndrome/symptoms-causes/syc-20376780.
“Puberty.” Cleveland Clinic, my.clevelandclinic.org/health/articles/22192-puberty. Accessed 11 June 2024.
“Selective Serotonin Reuptake Inhibitors (SSRIs).” Mayo Clinic, 17 Sep. 2019, www.mayoclinic.org/diseases-conditions/depression/in-depth/ssris/art-20044825.
“Sleep Problems and Menopause: What Can I Do?” National Institute on Aging, www.nia.nih.gov/health/menopause/sleep-problems-and-menopause-what-can-i-do. Accessed 11 June 2024.
“Stress.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/11874-stress. Accessed 11 June 2024.
SWAN Fact Sheet: Depression in Women – From Midlife and across the Menopause Transition (Perimenopausal Depression). www.swanstudy.org/wps/wp-content/uploads/2023/04/SWAN-Fact-Sheets-Depression.pdf.
Thurston, Rebecca C., and Hadine Joffe. “Vasomotor Symptoms and Menopause: Findings from the Study of Women’s Health across the Nation.” Obstetrics and Gynecology Clinics of North America, vol. 38, no. 3, Sep. 2011, pp. 489–501, https://doi.org/10.1016/j.ogc.2011.05.006.
“Vaginal Dryness after Menopause: How to Treat It?” Mayo Clinic, 14 May 2024, www.mayoclinic.org/diseases-conditions/menopause/expert-answers/vaginal-dryness/faq-20115086.
“What Is Menopause?” National Institute on Aging, www.nia.nih.gov/health/menopause/what-menopause. Accessed 11 June 2024.
“When to Take Hormone Replacement Therapy (HRT).” NHS, www.nhs.uk/medicines/hormone-replacement-therapy-hrt/when-to-take-hormone-replacement-therapy-hrt/. Accessed 11 June 2024.
Zouboulis, C. C., et al. “Skin, Hair and Beyond: The Impact of Menopause.” Climacteric, vol. 25, no. 5, Oct. 2022, pp. 434–42, doi: 10.1080/13697137.2022.2050206.
History of updates
Current version (14 June 2024)
Published (18 June 2024)
In this article

Track your perimenopause journey in the Flo app
-
Log symptoms and get tips to manage them
-
Learn what to expect with expert-led articles and videos
-
Connect with others who can relate to how you're feeling




