Constantly drained? Fatigue is a common symptom of perimenopause, so if you’re in your late 30s to 50s, then here’s what you should know — including what helps.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Perimenopause and fatigue: Why does perimenopause make you so tired?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Recently, we’ve started talking about menopause more, but lots of us are in the dark about perimenopause — aka the four to eight years (on average) before our periods stop. And that means when we’re faced with sleepless nights, low energy, and all-round exhaustion, we don’t always realize perimenopause could be the reason or that there’s help available.
Here’s the thing: Perimenopause and menopause are different, despite people often using the terms interchangeably. Simply put, perimenopause is the years leading up to menopause (your last period) when your periods become irregular or less frequent due to a change in hormones. Like puberty, it’s a natural transition in your cycle and can begin anytime between your late 30s and 50s.
You’re then diagnosed as having gone through menopause when you haven’t had a period for 12 months (usually between the ages of 45 and 55).
Lots of the symptoms we associate with menopause — think hot flashes, night sweats, and brain fog — actually happen in perimenopause, thanks to fluctuating hormones. But what about fatigue?
Obstetrician and gynecologist and attending physician, Jersey Shore University Medical Center, New Jersey, US, Dr. Angela Jones says this kind of fatigue affects around 50% of perimenopausal women. Let’s find out more.
Key takeaways
- Almost half (46%) of perimenopausal women experience fatigue.
- Perimenopause fatigue can mean you feel extreme tiredness.
- It can be connected to night sweats, which interrupt your sleep.
- If it’s impacting your quality of life, there are ways to manage and treat it.
Why does perimenopause cause fatigue?
During perimenopause, your levels of estrogen begin to fluctuate unevenly, and this can lead to symptoms in some women. But does this fluctuation cause fatigue?
More research is needed to be sure, but what we do know is the two are connected by another common symptom experienced by more than 80% of us: hot flashes. Experts believe these are brought on by that change in hormone levels during perimenopause. Hot flashes are that sudden feeling of heat that creeps up through the chest, neck, and face. When hot flashes happen at night (night sweats), they can mess with your sleep, and “this leads to fatigue in the days that follow,” says Dr. Jones.
Take a quiz
Find out what you can do with our Health Assistant
Is it normal to feel so tired?
Yes, it’s common to feel exhaustion during perimenopause. In fact, up to 46% of perimenopausal women experience fatigue.
How long does the tiredness last?
There’s no hard and fast rule here — everyone’s different. Fatigue can persist after menopause, and Dr. Jones says that if action isn’t taken to help alleviate your symptoms, it may last for years. So it’s well worth taking a look at her tips below and talking to your doctor about treatment options that can help.
What does perimenopause fatigue feel like?
Fatigue is defined as, and typically feels like, extreme tiredness, but there’s no universal experience of perimenopause fatigue. Dr. Jones says that most women describe feeling “exhausted and worn out.” You may have trouble getting up in the morning, making it through the day, or concentrating, and your eyes and entire body may feel tired.
It’s not just a physical thing, though. “Feelings of depression and anxiety are not unheard of during this transitional period,” Dr. Jones explains. You may experience angry outbursts or periods of sadness, plus other changes in mood brought on by a lack of sleep. But you don’t have to cope with this on your own; support and treatment are available.
Talking to friends about how you’re feeling can make a big difference, especially if they’re around the same age. You might find that they’re experiencing perimenopause symptoms themselves, and you can support each other by meeting up for a chat or messaging.
Being open about what you’re experiencing with family members and, if you feel comfortable, your boss and colleagues can also lessen the load. Suggest practical ways that they can help, such as picking up chores that need doing at home or moving meetings so that you can have regular breaks.
Book an appointment with your doctor, too. They will be able to provide advice, pull together a personalized treatment plan, and direct you to support services, should you need them.

Causes of perimenopause fatigue
Along with the hormonal changes we’ve already touched on, you might also be experiencing:
Life stress: Normal scenarios that occur in your 40s and 50s can also have an impact. You might be part of the sandwich generation, meaning you’re “juggling multiple responsibilities including demanding jobs, raising children, and caring for aging parents,” which can increase stress and sleepless nights, says Dr. Jones.
Depression and anxiety: As well as a lack of sleep helping to contribute to the development of depression and anxiety, fluctuating hormone levels increase the chances of both, too. If left untreated, depression and anxiety can get worse, and experiencing these in a more severe way can lead to increased fatigue. It’s a vicious cycle. The good news is your doctor can help, so don’t be afraid to reach out to them.
Physical changes: The physical symptoms you might experience, such as hot flashes and night sweats, can lead to fatigue. With your body going through so many changes, Dr. Jones says it’s no wonder that the majority of women feel exhausted during perimenopause.
Perimenopause fatigue: How to manage it
Fortunately, perimenopause fatigue can be successfully managed — and Dr. Jones recommends starting with some easy lifestyle tweaks. “Generally speaking, making these lifestyle modifications should help considerably,” she says. You’re probably doing a few of these already, but why not try increasing them?
Improve your bedtime routine
“Go to bed at the same time every night, and keep the bedroom quiet, cool, and dark. Put phones on ‘do not disturb’ or turn them over so that the light from the screen doesn’t disturb you,” she says. These are all good sleep hygiene practices that should help you get a more restful and restorative night’s sleep.
Exercise regularly
That means 150 minutes of moderate-intensity physical activity (anything that gets your heart rate up enough to burn three to six times as much energy as you do sitting down, e.g., walking or cycling quickly). It also means two days of muscle-strengthening activity per week (like lifting weights, dancing, or a yoga class) to improve your energy levels. “Focus on strength training, core-building exercises, and those that improve flexibility,” Dr. Jones says. “Building muscle mass will help you lose any unwanted weight gain [due to lower estrogen levels], too.”
Drink more water
Did you know that drinking enough water to stay hydrated can improve your chances of getting good quality sleep? We know that’s not always easy, so up your intake by choosing fruits and vegetables with a high water content, such as watermelon, cucumber, and cauliflower.
Practice relaxation techniques
Practicing relaxation techniques could be beneficial for your mental health. Even if you only have five minutes to spare, you could try:
- Deep breathing
- Self-massage
- Meditation
Or you could participate in:
- Yoga classes
- Tai chi
- Aromatherapy
Cut back on caffeine and alcohol
We get it — another double espresso feels like a no-brainer after a bad night. But too much caffeine increases your chances of another bad night. Why? Well, caffeine works by boosting dopamine signaling in your brain to make you feel more awake and alert. That’s fine during the day, but caffeine stays in your system for up to 10 hours. Experts agree that having more than 600 mg of caffeine a day (around four to seven cups of coffee) is too much and could likely affect your sleep. Just be sure to cut down gradually because you might experience withdrawal symptoms.
Drinking alcohol can have a similar impact on your sleep, with research suggesting that drinking it before bed can lead to disrupted and poor-quality sleep.
Eat a more varied diet
Eating foods that are high in protein (e.g., chicken, eggs, nuts, and yogurt), good fats (such as avocado and oily fish), iron (e.g. red meat, green leafy veggies, and dried fruit like apricots), and fiber (such as fortified breakfast cereals, whole wheat bread, and lentils) can boost your energy levels.
Take medication if you need to
“If you’re ever in doubt or the lifestyle modifications aren’t working, I’d suggest having a physician weigh in,” says Dr. Jones. They can help with a tailored treatment plan and prescribe medication that makes a real difference to your quality of life. This might include:
Birth control for perimenopause: “Low-dose birth control pills [also known as combined oral contraceptives] are an easy and common way to minimize these hormonal fluctuations” and improve fatigue, says Dr. Jones. They could also have the added bonus of helping to ease other symptoms, such as hot flashes and night sweats. First, visit your healthcare provider to figure out the underlying cause of the fatigue. They’ll be able to talk you through your options and make sure any new contraception won’t interfere with medication that you’re already taking.
Hormone treatments: Hormone therapy (HT), also known as hormone replacement therapy, can help ease mood swings during perimenopause, menopause depression, and other perimenopause symptoms that may be contributing to your sense of exhaustion, overwhelm, and fatigue.
When to see your doctor and what to say
It’s a good idea to reach out to your doctor if perimenopause fatigue is having a severe impact on your life or if you’re worried or have any questions.
It might help to prepare for your appointment by pinpointing when the fatigue started and making a list of any other symptoms you’re experiencing, plus any treatments you’ve tried. You might also want to ask your doctor questions, including whether you’ll need any tests, what treatment options are available, and what else you can do to help reduce your symptoms.
During the appointment, your doctor can figure out what’s going on, talk you through the different treatment options available, and provide the support you need.
It’s also important to reach out to your doctor right away if you’re experiencing fatigue alongside other symptoms, such as a fever or unintended weight loss.
What else could it be?
Fatigue usually isn’t something serious, but in some cases, it could be a sign of a health condition, such as autoimmune issues (including celiac disease, rheumatoid arthritis, or chronic fatigue syndrome), heart disease, cancer, diabetes, or even a simple infection. That’s why it’s important to see a health care professional if your fatigue persists or shows up alongside any other symptoms. They’ll help you identify the underlying cause and work with you on a treatment plan.
More FAQs
What are the symptoms of low estrogen?
The symptoms of low estrogen that are associated with perimenopause include mood changes, brain fog, hot flashes, night sweats, weight gain, irregular periods, heavier or lighter periods, needing to pee more often, insomnia and trouble sleeping, vaginal dryness, painful sex, and joint pain.
Does perimenopause fatigue ever go away?
As Dr. Jones explains: “Perimenopause is due to the change in hormones. Your hormones will continue to change after menopause, meaning you might continue to experience fatigue after perimenopause. However, lifestyle changes and medication such as HT are available, which could help to relieve fatigue.
What is the best vitamin for perimenopause fatigue?
Supplements aren’t recommended as a treatment option for perimenopause fatigue. “As long as you’re consuming a healthy, well-balanced diet and getting regular exercise, rest, and hydration, you should get all the vitamins you need,” says Dr. Jones.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Allen, Rebecca H., and Carrie A. Cwiak. Contraception for Midlife Women. NAMS Practice Pearl, The North American Menopause Society, 24 Sep. 2015, www.menopause.org/docs/default-source/professional/contraception-practice-pearl.pdf.
Bansal, Ramandeep, and Neelam Aggarwal. “Menopausal Hot Flashes: A Concise Review.” Journal of Mid-Life Health, vol. 10, no. 1, Jan.–Mar. 2019, pp. 6–13, journals.lww.com/jomh/fulltext/2019/10010/menopausal_hot_flashes__a_concise_review.3.aspx.
“Caffeine: How to Hack It and How to Quit It.” Cleveland Clinic, my.clevelandclinic.org/health/articles/15496-caffeine-how-to-hack-it-and-how-to-quit-it. Accessed 3 Nov. 2023.
Colrain, Ian M., et al. “Alcohol and the Sleeping Brain.” Handbook of Clinical Neurology, vol. 125, 2014, pp. 415–31, www.ncbi.nlm.nih.gov/pmc/articles/PMC5821259/.
“Depression (Major Depressive Disorder).” Mayo Clinic, 14 Oct. 2022, www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007.
“Fatigue.” Cleveland Clinic, my.clevelandclinic.org/health/symptoms/21206-fatigue. Accessed 3 Nov. 2023.
Harlow, Siobán D., et al. “Executive Summary of the Stages of Reproductive Aging Workshop +10: Addressing the Unfinished Agenda of Staging Reproductive Aging.” Climacteric, vol. 15, no. 2, Apr. 2012, pp. 105–14, www.tandfonline.com/doi/full/10.3109/13697137.2011.650656.
“Here’s How to Prevent Dehydration.” Cleveland Clinic, 21 Aug. 2023, health.clevelandclinic.org/how-to-prevent-dehydration/.
“Hot Flashes.” Mayo Clinic, 20 May 2022, www.mayoclinic.org/diseases-conditions/hot-flashes/symptoms-causes/syc-20352790.
“How Much Physical Activity Do Adults Need?” Centers for Disease Control and Prevention, www.cdc.gov/physicalactivity/basics/adults/index.htm. Accessed 3 Nov. 2023.
“How to Fall Asleep Faster and Sleep Better.” NHS, www.nhs.uk/every-mind-matters/mental-wellbeing-tips/how-to-fall-asleep-faster-and-sleep-better/. Accessed 3 Nov. 2023.
“How to Improve Your Strength And Flexibility.” NHS, www.nhs.uk/live-well/exercise/strength-and-flexibility-exercises/how-to-improve-strength-flexibility/. Accessed 3 Nov. 2023.
“Menopause.” NHS, www.nhs.uk/conditions/menopause/. Accessed 3 Nov. 2023.
“Menopause.” World Health Organization, 17 Oct. 2022, www.who.int/news-room/fact-sheets/detail/menopause.
“Menopause Symptoms FAQs.” The North American Menopause Society, www.menopause.org/for-women/expert-answers-to-frequently-asked-questions-about-menopause/menopause-symptoms-faqs. Accessed 3 Nov. 2023.
“Menopause: Symptoms.” NHS, www.nhs.uk/conditions/menopause/symptoms/. Accessed 3 Nov. 2023.
“Perimenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21608-perimenopause. Accessed 3 Nov. 2023.
“Perimenopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666.
“Relaxation Techniques: Try These Steps to Reduce Stress.” Mayo Clinic, 28 Apr. 2022, www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/relaxation-technique/art-20045368.
Rosinger, Asher Y., et al. “Short Sleep Duration Is Associated with Inadequate Hydration: Cross-Cultural Evidence from US and Chinese Adults.” Sleep, vol. 42, no. 2, Feb. 2019, doi.org/10.1093/sleep/zsy210.
Silver, Nazanin E. “Mood Changes during Perimenopause Are Real. Here’s What to Know.” The American College of Obstetricians and Gynecologists, Apr. 2023, www.acog.org/womens-health/experts-and-stories/the-latest/mood-changes-during-perimenopause-are-real-heres-what-to-know.
“Staying Active.” Harvard T.H. Chan School of Public Health, www.hsph.harvard.edu/nutritionsource/staying-active/. Accessed 3 Nov. 2023.
Taylor-Swanson, Lisa, et al. “The Dynamics of Stress and Fatigue across Menopause: Attractors, Coupling, and Resilience.” Menopause, vol. 25, no. 4, Apr. 2018, pp. 380–90,
www.ncbi.nlm.nih.gov/pmc/articles/PMC5866170/.
“The Menopause Years.” The American College of Obstetricians and Gynecologists, Dec. 2018, www.acog.org/womens-health/faqs/the-menopause-years.
“The Reality of Menopause Weight Gain.” Mayo Clinic, 8 July 2023, www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/menopause-weight-gain/art-20046058.
“Water and Healthier Drinks.” Centers for Disease Control and Prevention, www.cdc.gov/healthyweight/healthy_eating/water-and-healthier-drinks.html. Accessed 3 Nov. 2023.
History of updates
Current version (15 November 2023)
Published (17 November 2023)
In this article
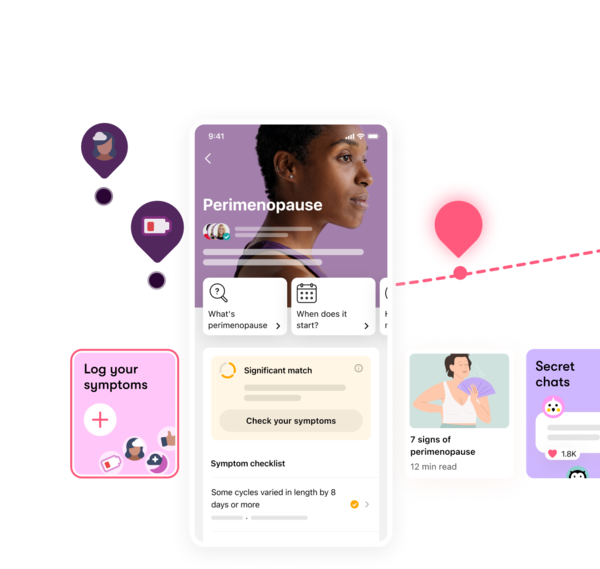
Track your perimenopause journey in the Flo app
-
Log symptoms and get tips to manage them
-
Learn what to expect with expert-led articles and videos
-
Connect with others who can relate to how you're feeling




