Mention "uterine polyps" to most women and you’ll draw a blank stare. It’s not a condition with which many women are familiar, but polyps aren’t rare. According to some estimates, as many as 10% of women without visible symptoms are diagnosed with uterine polyps (also known as endometrial polyps). The polyps are also a very common cause of abnormal vaginal bleeding.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Causes of Uterine Polyps, a Common Reason for Bleeding During Menopause


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Being diagnosed with uterine polyps can be a worrying time for a woman and it’s natural to have concerns about cancer. Although the majority of cases are completely benign and non-cancerous, some endometrial polyps do develop into cancer at a later stage. For this reason, it’s important for women to be aware of the condition and its treatment.
What are uterine polyps?
Many women are unaware of uterine polyps until being diagnosed by a healthcare provider. This can be an anxious time and it’s natural to have some worries about the condition. If you’re in this position, or even if you’re not, one of the best things you can do is to make yourself aware of the condition and its symptoms.
Uterine polyps are small tissue growths on the inside of the womb (also called the uterus). Since these growths come from the endometrium — the lining of the womb — they are also called endometrial polyps.
Uterine polyps can vary enormously in size: some are as small as a sesame seed, while others are as large as a golf ball. It’s also possible to have a single polyp or many and most polyps stay within the womb. In some cases however the polyp may pass through the cervix (neck of the womb) and into the vagina.
It’s common for the condition to be symptom-free, and so many women will be completely unaware that they have polyps.
It will be stressful to find out that you have endometrial polyps, but remember that most cases are entirely benign (non-cancerous). Having polyps does not mean that you have cancer, but you should be aware that some polyps later become cancerous.
After diagnosis, your healthcare provider will be able to offer you advice on the range of treatment options that are available to you. They will also be able to talk to you about the risk of developing cancer later.
Some factors can increase the risk of developing endometrial polyps:
- obesity
- high blood pressure
- menopause
- taking tamoxifen, a breast cancer drug

Can uterine polyps cause bleeding during menopause?
Although many women with endometrial polyps experience no symptoms, the most common sign is bleeding. For a postmenopausal woman, vaginal bleeding may mean that one or more polyps have developed. If you are concerned that this is the case, seek advice from a trusted healthcare provider — they will be able to offer expert counsel on the most appropriate investigations.
Causes of recurrent uterine polyps
In some cases, women experience a recurrence of endometrial polyps and a return of symptoms. If this happens you will need to resume treatment, either by medication or surgery.
Take a quiz
Find out what you can do with our Health Assistant
Diagnosis of endometrial polyps
We still don’t know exactly what causes endometrial polyps, but hormone levels may play a part in how they develop. During your menstrual cycle, the level of estrogen in your body rises and falls and this is what causes the lining of your womb to develop in preparation for a fertilized egg.
Overactivity in the development of the lining results in a uterine polyp. Most commonly they affect women right before and during menopause. This means that you are more likely to be diagnosed with polyps in your 40s and 50s when estrogen levels in your body are fluctuating. In some cases, younger women can also develop polyps.
Uterine polyps may cause no symptoms, particularly if there is a single polyp or if they are small. The most common sign is bleeding but you may notice any combination of these other symptoms:
- irregular periods that vary in their timing and heaviness
- heavy periods
- bleeding or spotting between periods
- bleeding after menopause
- difficulty getting pregnant
The symptoms of uterine polyps can be identical to those of uterine cancer — even though most cases are benign, it’s important to take the condition seriously. Polyps are more likely to be a precursor to cancer in women who are postmenopausal.
Your doctor will also be careful to check if you have uterine fibroids rather than polyps. There are many similarities between polyps and fibroids, but a number of important differences. Unlike polyps that grow from the lining of the uterus, fibroids develop from the muscle of the wall of the uterus.
Fibroids can cause heavy bleeding but are also associated with symptoms like pain, constipation, and difficulty urinating. Fibroids can be investigated using the same methods as those that are used for endometrial polyps.
There are a number of different methods available to further investigate endometrial polyps. Your doctor will be able to explain which of these is available and most suitable for you:
- Ultrasound. A thin wand-like device will be inserted into your vagina and produce an image of your womb. Your doctor may also put a thin tube into your vagina and inject salt water into your uterus. This will inflate the uterus and make a better view of it during the ultrasound (it is called hysterosonography).
- Hysteroscopy. A thin flexible, lighted telescope, called a hysteroscope, will be inserted into your vagina and uterus. This will allow your doctor to see inside the womb and check for polyps. Your doctor can also remove any polyps that are found during the hysteroscopy.
- Endometrial biopsy. While examining your womb, your doctor may wish to use a plastic instrument to take a sample of the tissue from your endometrium. This sample will be sent to a laboratory and examined carefully for any signs of cancer.
- Curettage. This is a surgical procedure that is performed in an operating room. A metal instrument called a curette is used to take samples of tissue from polyps. The curette can also be used to remove the polyps.
Do not hesitate to ask your healthcare provider for advice if you are unclear about any aspect of these investigations.

Uterine polyp treatment
Your doctor will recommend the most appropriate course of action in your particular case. This can include any one of the following options:
Watchful waiting. If you have symptomless endometrial polyps that are benign, the doctor may choose to do nothing. You can wait and see if it goes away on its own. However, your doctor may still recommend that you remove the polyp if you are menopausal/perimenopausal or if you are thought to be at higher risk of uterine cancer.
Medication. A number of medications are available for the treatment of uterine polyps. They are called progestins and gonadotropin-releasing hormone agonists. They work by controlling your hormone levels (which may be affected by menopause or other factors). These drugs can reduce the size of polyps and improve symptoms like heavy bleeding. Unfortunately, these symptoms often return as soon as you stop taking the medication.
Uterine polyp removal surgery
In addition to the medical treatments mentioned above, your health professional will be able to advise you about surgical options that are available.
Endometrial polyps can be treated by the same methods as they are investigated. For example, polyps can be removed during a hysteroscopy or curettage. In cases where cancer cells are present, it may be necessary to remove the entire uterus in a procedure called a hysterectomy. This can be upsetting for many women, but your health professional will be able to offer the best and most expert advice in these cases.
The wide range of medical and surgical options available for the treatment of endometrial polyps can cause stress and confusion for many women. Remember that your doctor has your interests at heart — don’t hesitate to seek their advice about any aspect of your treatment. This way you can be confident that you’re receiving the best possible medical care.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
History of updates
Current version (17 February 2022)
Published (09 November 2018)
In this article
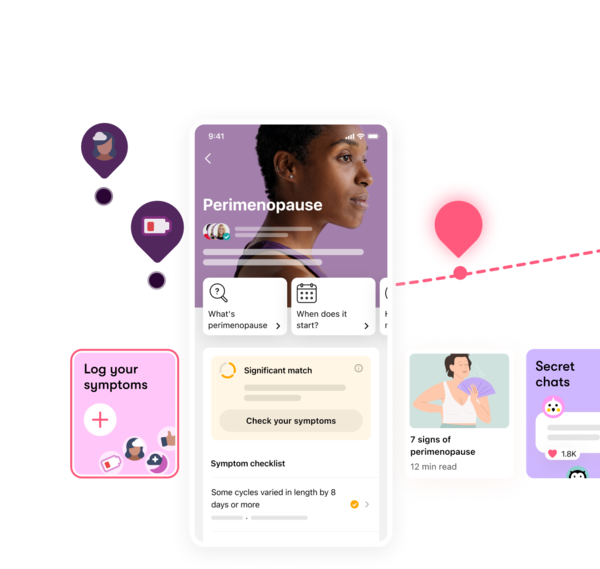
Track your perimenopause journey in the Flo app
-
Log symptoms and get tips to manage them
-
Learn what to expect with expert-led articles and videos
-
Connect with others who can relate to how you're feeling




