IUD cramps can be unpleasant, but they are common and usually temporary. Our Flo expert explains what’s normal and when to speak to your doctor.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
IUD cramps: What’s normal and how to ease the pain


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
When it comes to the pros and cons of birth control, intrauterine devices (IUDs) have a lot going for them.
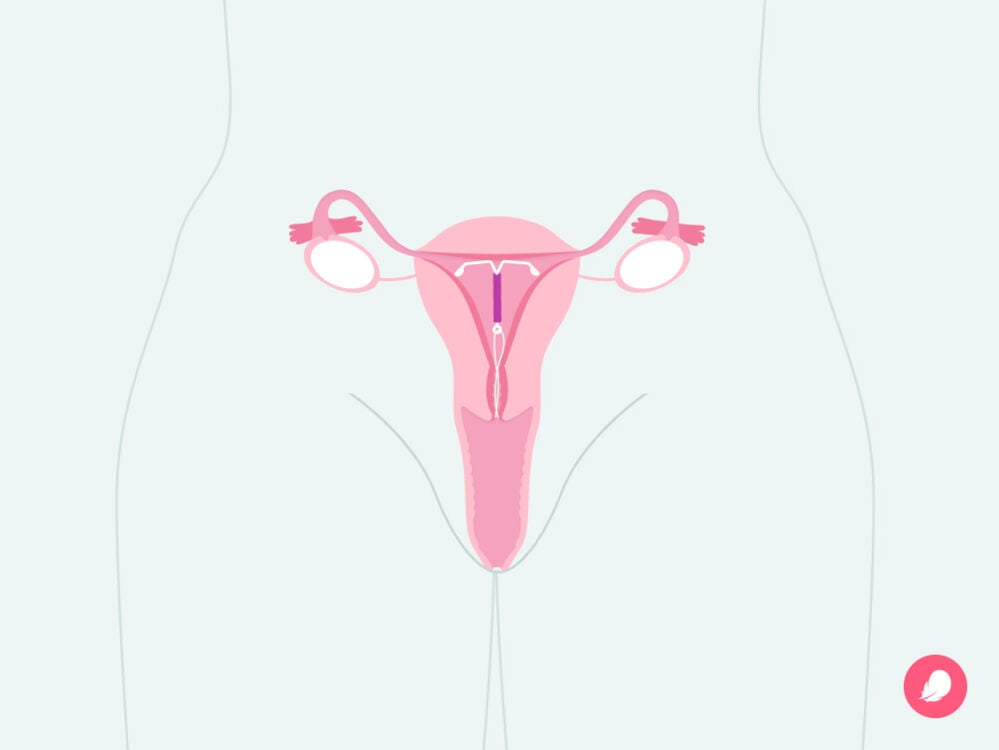
The small, T-shaped device is inserted in your uterus by your health care provider. They are one of the most effective kinds of birth control, with a pregnancy rate of less than 1%. Once they’re in, they can prevent pregnancy for three to 10 years (depending on the brand) without you having to do a thing. You can also wave goodbye to birth control pill reminders.
However, like with other types of contraception, IUDs can have negative side effects too (and it’s important to remember that they won’t protect you against sexually transmitted infections [STIs]). Among the most common side effects of IUDs is cramping. Understanding what’s normal — and what’s not — can help you navigate your IUD experience with confidence.
Key takeaways
- It’s common to have cramps for up to three to six months after you’ve had an IUD fitted.
- Any pain that goes on longer than this is not normal, and you should get in touch with your doctor.
- IUD cramps can range from mild to intense. Regular painkillers and a heating pad can help you manage the pain.
Why you might experience cramping with an IUD
So if IUD cramps are a common side effect, what causes them? Well, IUD cramps can happen during and after insertion as your cervix needs to open to let the device through. Plus, one particular type of IUD — the copper IUD — can make periods heavier and more painful. For some women, these effects on their period lessen over time. IUD cramps can also be caused by the device becoming displaced at any point.
These cramps shouldn’t interrupt your day-to-day life, so if you’re experiencing cramping or lower back pain that’s severe or persistent, abnormal bleeding, or dizziness, get in touch with your doctor.
What to expect from IUD insertion
If you haven’t had an IUD inserted yet, you might be wondering what to expect from the appointment. And with all this talk of cramping and IUD pain, it’s understandable if you feel a little nervous. Your doctor can help you decide if an IUD is the best option for you. They may also suggest doing a pregnancy or STI test first.
So, let’s break down what happens at these appointments:
- First, your health care provider should walk you through every step of the insertion so you understand what they are doing and when.
- Your doctor may offer you pain relief ahead of your IUD being fitted.
- Your doctor may also measure the depth of your uterus. If you’re reading this and wondering how they could do this, it’s quite easily explained. Your health care provider will use a thin device called a speculum to help gently widen your vagina and make sure the cervix is visible. If you’ve had a Pap smear test before, this may feel similar. Then, they will use a different tool to measure the depth of your uterus.
- After that, your doctor will carefully put the IUD in place inside your uterus.
This whole procedure should take no longer than five minutes. If at any point you’re confused or want your doctor to stop, then you’re absolutely within your rights to say so. They will be able to pause and answer any of your questions or concerns.
Since everyone’s experience of IUD insertion can be slightly different, it’s hard to know what to expect. However, Dr. Katharine Claire DeGeorge, associate professor of family medicine at the University of Virginia, US, explains, “It’s very common to have cramping that feels like menstrual cramps in the days and weeks after IUD placement as your body gets used to having the IUD in your uterus. Your body can recognize the presence of something in the uterus and can respond by cramping.”
Cramping during and after IUD insertion
Understanding what happens when your IUD is fitted can help to explain when and why you might feel cramping during and after IUD insertion. Some people say they start feeling cramping:
- When their doctor measures the depth of the uterus before their IUD is fitted
- When their IUD is placed
- When their appointment is over, and they’re recovering at home
After your IUD is fitted, the pain can range from sore to more intense. You might feel it more in your abdomen or lower back as a pulsing low-level pain. But it shouldn’t be worse than your typical period cramps, according to Dr. DeGeorge.
You might also notice that the pain stops a day or two after the procedure. For others, though, the pain can continue for up to three to six months. It’s important that you speak to your doctor if your IUD is causing bad cramping — they’re on hand to help.
How to help IUD cramps
The prospect of cramping isn’t a pleasant one, but the good news is there are things you can do before (and during) your IUD fitting appointment to help prevent pain.
First up, “Take an NSAID about 30 minutes beforehand,” says Dr. DeGeorge. NSAID stands for nonsteroidal anti-inflammatory drugs — and is just the medical term for common over-the-counter pain relief like aspirin or ibuprofen.
“During the procedure, try to relax. Imagining you are sinking your pelvis into the table can really help,” she explains. “You can also help avoid cramping by coming to the appointment rested and healthy.” So, if you can, spend the hours before your appointment doing the things that make you feel most relaxed — maybe that’s watching your favorite show or doing some yoga. Whatever helps.
Remember to share any concerns you have with your doctor, too. They are there to support you.
Then, after your appointment, you can continue to take pain relief medication when you need to. You can also try using a heating pad to ease any cramps or have a warm bath. If the cramping you’re experiencing feels intense or unbearable, then call your health care provider. They will be able to advise you on your best next step.
Take a quiz
Find out what you can do with our Health Assistant
Longer-term IUD cramping
We now know that cramping can be a common side effect after you’ve had an IUD fitted. It can also be different depending on the type of IUD you get. The copper IUD, for example, is known to sometimes cause more painful and heavier periods for the first few months. However, if longer-term IUD cramping lasts for more than three to six months, it’s something you need to get checked out.
“Cramping for longer than three months after placement or severe cramping at any point may be a sign that the IUD has dislodged and is not in the correct place,” says Dr. DeGeorge. It may also be a sign that your IUD doesn’t fit the shape of your uterus properly. Speak to your health care provider about the pain you’re experiencing. They may recommend that you have your IUD refitted or taken out.
When to get medical advice for IUD pain
While it may be common, cramping and pain after you’ve had an IUD fitted isn’t something you have to deal with by yourself. If you’re uncomfortable in the hours, days, or weeks after the procedure, then don’t hesitate to reach out to your doctor. They may be able to recommend pain relief medication or ways to soothe your cramps at home.
Remember: “If the cramps are severe, last more than three months, or if at any point they are associated with heavy bleeding, pus-like discharge, or abnormal odor, you should see your doctor right away,” Dr. DeGoerge says. “These could be signs that the IUD is not in the correct position or of infection.”
Similarly, if you feel lightheaded or dizzy or experience light bleeding or spotting, then speak to your health care provider.
More FAQs
Is it OK to feel your IUD with your fingers?
It is OK to feel your IUD strings with your fingers, but as your IUD is placed high up in your uterus, you won’t be able to feel the device. Make sure you wash your hands first, and then carefully place one finger inside your vagina to find your cervix, which will feel hard and rubbery. The strings should be coming through your cervix.
How do you know if your IUD is out of place?
If your IUD falls out of place, you may not notice, but you might experience pain or bleeding. You may also notice if you cannot feel your IUD strings, the strings feel much longer than before, or you feel the hard plastic part of the IUD. If any of the above happens, you should call your doctor.
Can cramping move your IUD?
Cramps can be unpleasant and worrying, but there is no evidence to suggest that cramps can move your IUD. A dislodged IUD can cause pain rather than the other way around.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Appendix D: Contraceptive Effectiveness.” Centers for Disease Control and Prevention, 25 Apr. 2014, www.cdc.gov/mmwr/preview/mmwrhtml/rr6304a5.htm.
Casey, Frances E. “Intrauterine Devices (IUDs).” MSD Manual Consumer Version, Oct. 2023, www.msdmanuals.com/home/women-s-health-issues/family-planning/intrauterine-devices-iuds.
“Hormonal IUD (Mirena).” Mayo Clinic, 20 Aug. 2022, www.mayoclinic.org/tests-procedures/mirena/about/pac-20391354.
Hubacher, David, et al. “Side Effects from the Copper IUD: Do They Decrease over Time?” Contraception, vol. 79, no. 5, May 2009, pp. 356–62, www.ncbi.nlm.nih.gov/pmc/articles/PMC2702765.
“Intrauterine Device (IUD).” Cleveland Clinic, my.clevelandclinic.org/health/treatments/24441-intrauterine-device-iud. Accessed 4 Mar. 2024.
IUD Aftercare Instructions. University of Washington Department of Obstetrics and Gynecology, www.uwmedicine.org/sites/stevie/files/2018-11/IUD-Aftercare-Instructions.pdf. Accessed 4 Mar. 2024.
“Know the Facts: #GYT.” Centers for Disease Control and Prevention, www.cdc.gov/std/sam/gyt/knowthefacts.htm. Accessed 4 Mar. 2024.
Lanzola, Emily L., and Kari Ketvertis. “Intrauterine Device.” StatPearls, StatPearls Publishing, 26 June 2023, www.ncbi.nlm.nih.gov/books/NBK557403.
“Long-Acting Reversible Contraception (LARC): Intrauterine Device (IUD) and Implant.” The American College of Obstetricians and Gynecologists, Apr. 2023, www.acog.org/womens-health/faqs/long-acting-reversible-contraception-iud-and-implant.
“Prostaglandins.” Cleveland Clinic, my.clevelandclinic.org/health/articles/24411-prostaglandins. Accessed 4 Mar. 2024.
Roy, Subir, and S. T. Shaw Jr. “Role of Prostaglandins in IUD-Associated Uterine Bleeding—Effect of a Prostaglandin Synthetase Inhibitor (Ibuprofen).” Obstetrics and Gynecology, vol. 58, no. 1, July 1981, p. 101-06, journals.lww.com/greenjournal/abstract/1981/07000/role_of_prostaglandins_in_iud_associated_uterine.19.aspx.
Trobough, G. E. “Pelvic Pain and the IUD.” The Journal of Reproductive Medicine, vol. 20, no. 3, Mar. 1978, pp. 167–74, pubmed.ncbi.nlm.nih.gov/347074.
“What Are the Side Effects of IUDs?” Drugs.com, 17 Jan. 2024, www.drugs.com/medical-answers/side-effects-iuds-3439694.
“What Should I Expect after a Mirena IUD Removal?” Drugs.com, 13 Feb. 2024, www.drugs.com/medical-answers/expect-after-mirena-iud-removal-3572407.




