Vaginismus causes painful sex, but you don’t need to put up with it. A sex therapist and an OB-GYN talk us through the signs, symptoms, and causes if you think you might have it, along with different treatment options
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Vaginismus: How do I know if I have it?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Almost three out of four women will experience painful sex (we’re specifically talking penetrative sex here) at some point in their lives — be it through a simple lack of desire or arousal or a gynecological condition. In many cases, the issue is only temporary and can be easily resolved.
For some people, though, painful penetration — caused by trying to insert a penis, sex toy, or even a tampon — can be a long-term issue. And it’s one that leads many people to avoid penetration altogether.
If you can relate or have ever experienced what feels like an involuntary tightening of your vagina that makes penetration really difficult, you might want to learn more about vaginismus.
Take a quiz
Find out what you can do with our Health Assistant
What is vaginismus?
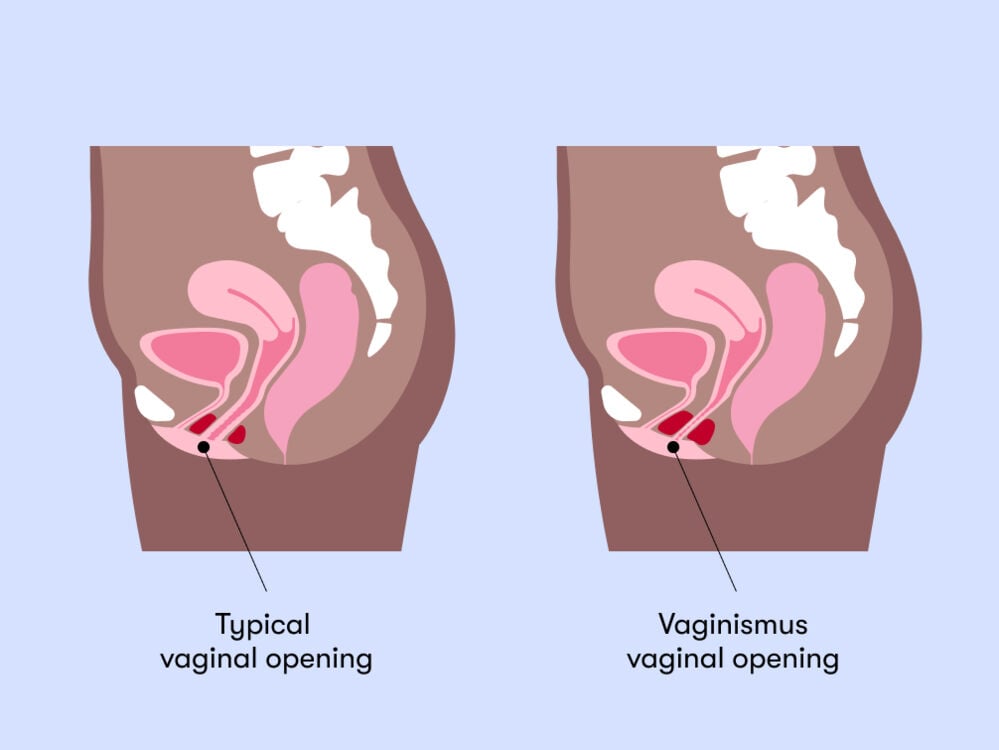
Vaginismus is a condition in which the muscles at the entrance to the vagina (also known as pelvic floor muscles) suddenly tighten up at the moment of penetration. It’s totally involuntary and can make penetration incredibly painful and/or downright impossible, especially if you're having sex for the first time.
“When I see people with vaginismus who have male sexual partners, they’ll say that when they first tried vaginal penetration, it was like the penis was hitting a wall,” explains sex therapist Jordan Rullo, Ph.D. “That is the most common phrase I hear: It is not possible to penetrate. There’s a wall there.”
In addition to physical symptoms, obstetrician and gynecologist Sara Twogood, M.D., says people with vaginismus may also experience “fear or anxiety about pain in anticipation of genital contact.”
That means the condition isn’t only triggered by penetrative sex. Some people with vaginismus may tense up during medical exams or struggle to insert a tampon. They also might experience symptoms in some situations but not in others. And it might be something they’ve always dealt with or that starts happening later in life.
What causes vaginismus?
Reasons vary from person to person, and there can also be a few things in play at once. “There are no direct correlations such as ‘You get this infection, and that leads to vaginismus,’” Dr. Twogood says.
“But there are some risk factors that increase the chance of developing vaginismus — history of sexual trauma or assault, chronic vulvar infections, and vulvar skin disorders.”
In some cases, the condition develops after a difficult medical experience like traumatic childbirth. A study published in the Journal of Sexual Medicine found the condition to be more common in participants who were also prone to anxiety. But sometimes, there isn’t a reason a person can put their finger on at all.
"You need an accurate diagnosis, so don’t take no for an answer"
How common is vaginismus?
A study published in Sexual Medicine, an official journal of the International Society for Sexual Medicine, found it affects 5% to 17% of women in clinical settings. But the problem is, we don’t know exactly how common it is in general since many people never get a diagnosis.
This could be for a number of reasons.
Vaginismus is still relatively unheard of. Fortunately, that’s changing (albeit slowly), with recent shows like Sex Education, Masters of Sex, and Unorthodox featuring characters with the condition. And since the pain of women and everyone with a vagina has long been dismissed and normalized, many people simply accept it as part of life.
Do I have vaginismus?
If you think you may have the condition, here are the next steps.
1. Stop having painful sex
“If you’re having painful sex, stop. And that sounds like such a simple message. But so many women I see are having painful sex, and they think [it’s] just life,” Rullo says. But it’s not, and you don’t have to continue experiencing it.
2. Seek support
To get the treatment you need, the first step is to visit your gynecologist or health care provider. They may ask to examine you to rule out other possible causes.
3. Be prepared to advocate for yourself
“So many women are dismissed, under-diagnosed, or don’t even seek treatment,” Rullo explains. “I cannot tell you the number of women I’ve seen in my office who have said, ‘Well, this happened from when I first tried to have penetrative sex, but [I was told to] just relax, have a glass of wine, and [it’ll] be fine.’”
Rullo says she isn’t sharing these experiences to put anyone off from seeking help — quite the opposite. It’s critical to advocate for yourself if you’re dealing with sexual pain, even if it means seeing a few different health care providers, she says. “You need an accurate diagnosis, so don’t take no for an answer,” Rullo adds.
Vaginismus treatment
Once vaginismus is diagnosed, you might need to try a few different types of therapy. The goal is to manage your feelings around penetration and reduce fear and anxiety while gradually getting used to the physical sensations.
“As a psychologist, my treatment protocol involves three things,” Rullo explains ….
1. Relaxing the mind
Relaxing the mind might involve talk therapy, such as cognitive behavioral therapy (CBT) or trauma-focused therapy if appropriate.
2. Relaxing the muscles
This could be pelvic floor exercises, along with the use of dilators. These are tube-shaped objects of different sizes, which you insert into the vagina. You begin with the very smallest and work up to the next size once you’re comfortable.
There are also physical therapists who specialize in pelvic floor muscle dysfunction that you can be referred to for more assistance. It’s important to recognize that this process takes time and consistency.
3. Sensate focus
Sensate focus is “a kind of exposure therapy in which you learn to be comfortable with physical touch,” she says. Sensate-focused exercises are suitable for people who have learned to avoid all types of physical intimacy. The idea is to get used to touching a partner without penetration, safe in the knowledge that this kind of contact isn’t going to hurt.
If the pain continues, there are other treatment options.
Medication for vaginismus
“Options include topical medications like topical estrogen, lidocaine, or compounded prescriptions like gabapentin,” Dr. Twogood says.
“Other options include antidepressants and neuropathic pain medications. We try one or two medications at a time and give them time to work. Then we adjust from there.”
However, medication use isn’t common.
Vaginismus: The takeaway
For anyone with vaginismus, the key takeaway is not to despair or lose hope. That same Sexual Medicine study that looked into how common the condition is in clinical settings also found that 71% of vaginismus patients reported having pain-free sex after five weeks of following a treatment program.
So rest assured that it can be managed with the right care and attention.
And some parting advice from Dr. Twogood: “Be patient with yourself. There is no one easy fix, but there are lots of treatment options. With time and the right combination of medications and treatments for you, there can be relief.”


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“When Sex Is Painful.” American College of Obstetricians and Gynecologists, Aug. 2018, www.acog.org/womens-health/faqs/when-sex-is-painful.
Conforti, Celine. “Genito-Pelvic Pain/Penetration Disorder (GPPPD): An Overview of Current Terminology, Etiology, and Treatment.” University of Ottawa Journal of Medicine, vol. 7, no. 2, 2017, pp. 48–53. Crossref, https://doi.org/10.18192/uojm.v7i2.2198.
NHS Choices. “Vaginismus.” Nhs.Uk, 18 Nov. 2021, www.nhs.uk/conditions/vaginismus.
“Vaginismus.” National Library of Medicine, 3 June 2020, medlineplus.gov/ency/article/001487.htm.
Lamont, John A. “Dyspareunia and Vaginismus.” The Global Library of Women’s Medicine, 2009. Crossref, https://doi.org/10.3843/glowm.10430.
Banaei, Mojdeh, et al. “Bio-Psychosocial Factor of Vaginismus in Iranian Women.” Reproductive Health, vol. 18, no. 1, 2021. Crossref, https://doi.org/10.1186/s12978-021-01260-2.
Azim, Katharina A., et al. “Exploring Relationships Between Genito-Pelvic Pain/Penetration Disorder, Sex Guilt, and Religiosity Among College Women in the U.S.” The Journal of Sexual Medicine, vol. 18, no. 4, 2021, pp. 770–82. Crossref, https://doi.org/10.1016/j.jsxm.2021.02.003.
Watts, Gayle, and Daniel Nettle. “The Role of Anxiety in Vaginismus: A Case-Control Study.” The Journal of Sexual Medicine, vol. 7, no. 1, 2010, pp. 143–48. Crossref, https://doi.org/10.1111/j.1743-6109.2009.01365.x.
Pacik, Peter T., and Simon Geletta. “Vaginismus Treatment: Clinical Trials Follow Up 241 Patients.” Sexual Medicine, vol. 5, no. 2, 2017, pp. e114–23. Crossref, https://doi.org/10.1016/j.esxm.2017.02.002.




