Fibroids won’t affect most pregnancies, but there’s a small possibility that complications can arise. Find out what the research says.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Uterine fibroids and pregnancy: Everything you need to know

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
If you’ve been diagnosed with a uterine fibroid or suspect you might have one, then it’s understandable to have concerns or questions. Maybe you’re wondering about your fertility or how it might affect a future pregnancy. Or maybe you want to know what a fibroid is exactly and what the treatment options are. We’re here to help.
Before we find out more, please know that uterine fibroids are common and benign (noncancerous). They also don’t increase your risk of developing uterine cancer.
Key takeaways
- Uterine fibroids are a common condition in which growths develop in or on the uterus.
- Fibroids are noncancerous and do not increase your uterine cancer risk.
- In most cases, fibroids have no symptoms. But common symptoms can include pain and heavy menstrual bleeding.
- In some cases, fibroids can affect pregnancy or fertility. However, many women can still get pregnant and have healthy babies with fibroids.
What are uterine fibroids?
Uterine fibroids are noncancerous muscle growths that develop in or around your uterus. That might sound scary, but rest assured, they’re incredibly common. In fact, as many as 70% of women will develop a fibroid at some point in their lifetime. And that number could be even higher since they often don’t cause any symptoms and go undiagnosed.
Fibroids can grow on their own or in a cluster. They vary greatly in size, ranging from 1 mm to 20 cm (8 in) in diameter or larger. For comparison, that means fibroids can be as small as a seed or as large as a watermelon.
How are uterine fibroids diagnosed?
To diagnose you with fibroids, your health care provider will usually carry out a pelvic exam to check for any obvious signs of the growths. If further investigation is needed, they may refer you for an ultrasound, to a specialist, or both.
However, it might surprise you to hear that fibroids are often picked up by chance during a routine pelvic exam or ultrasound, although this usually only happens when they are large enough to be felt or seen. Smaller fibroids may go undetected for long periods of time, especially if they don’t cause any symptoms.
Types of uterine fibroids
Take a quiz
Find out what you can do with our Health Assistant
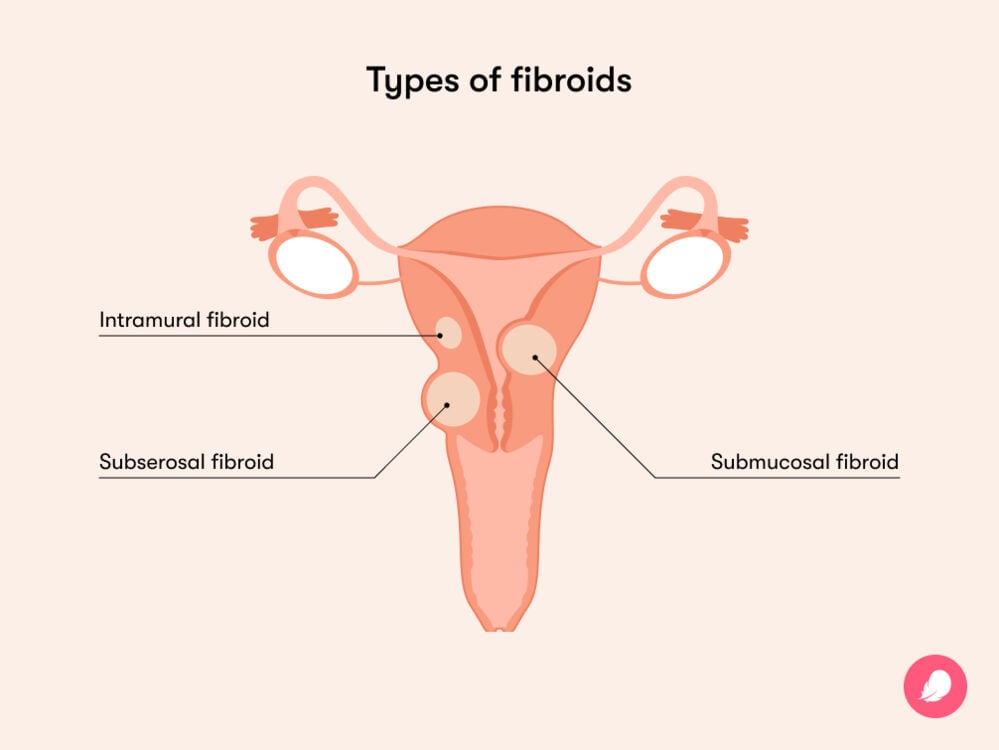
There are a number of different types of uterine fibroids, including:
- Intramural fibroids: These are the most common type. They grow in the muscle wall of the uterus.
- Subserosal fibroids: These grow under the lining of the outer surface of the uterus and can become quite large.
- Submucosal fibroids: This type often grows in the muscle layer beneath the inner lining of the uterus.
If you have a subserosal or submucosal fibroid, it’s worth knowing that they can also become pedunculated. This is a medical term meaning they have a stalk or a stem that attaches to the uterus, making them look a bit like mushrooms.
What causes uterine fibroids?
Experts don’t know exactly what causes fibroids, but there are a few theories.
One of these involves hormones, as both estrogen and progesterone seem to promote the growth of fibroids. This idea is backed up by the fact that fibroids tend to shrink or stop growing once a person reaches menopause and their hormone levels dip.
Another potential cause is gene changes. Researchers have found that uterine fibroids have gene changes that don’t appear in other cells of the uterine muscle. However, more research is needed to pinpoint the exact cause.
Who's at higher risk of developing fibroids?
Several risk factors have been found to impact your chances of developing fibroids:
- Genetics: A 2012 study found that having a family member with fibroids increases your risk, suggesting there’s a hereditary link at play.
- Race: Studies have found that fibroids are more common and symptoms tend to be more severe among African-American women. If you think you might be at an increased risk of developing fibroids, speak to your doctor about getting any tests or extra monitoring and the treatment options that might be available.
- Lifestyle: Diet, drinking alcohol, vitamin D deficiency, obesity, and a high body mass index have all been found to play a role in the development of fibroids.
If you think you might have an increased risk of developing uterine fibroids, it’s always best to reach out to your doctor for advice.

Symptoms of uterine fibroids
Since some uterine fibroids are small and have no symptoms, you might not even realize you have them. If you do experience symptoms, they may vary depending on the number of fibroids you have, their location, and their size. Symptoms can include:
- Heavy menstrual bleeding and longer periods
- Bleeding/spotting between periods
- Menstrual cramps
- Anemia (low iron due to heavy bleeding associated with fibroids)
- Pain during sex
- Pain in the lower back or abdomen and pelvic pain (when fibroids press on surrounding organs)
- Needing to pee more often or having difficulty emptying your bladder
- Swelling in your uterus or abdomen (in cases of big fibroids)
- Constipation
In some cases, it’s possible that fibroids could also cause miscarriages, although this is rare. If you’re pregnant and have fibroids, then try not to worry (easier said than done, we know). Researchers are still unclear on the exact link between them.
Some studies have found that fibroids larger than 4 cm could increase the risk of reproductive problems, and other studies have found that fibroids smaller than 5 cm had no impact at all.
More research is needed to understand this issue, but in the meantime, if you have any questions or concerns, then be sure to reach out to your health care provider.
Uterine fibroids and fertility
Most people who have uterine fibroids go on to have healthy pregnancies.
Rarely, however, uterine fibroids can be an initial cause of infertility, although this only affects around 2% to 3% of people with fibroids. Please don’t lose hope if this is the case for you. Experts say that most women can still get pregnant following treatment for fibroids. In fact, one study found that 75% of women got pregnant after a myomectomy (more on that below).
If you are trying to conceive and have symptoms of a possible fibroid, then it’s best to book a checkup with your health care provider. They’ll be able to investigate further and, if needed, discuss your options to maximize your chances of having a baby.
How to treat fibroids to potentially improve fertility
We now know that treating uterine fibroids before pregnancy may improve your fertility outcomes. But what exactly does that involve?
Fibroid treatment depends on a few factors, including the size and number of fibroids and the severity of your symptoms. Your health care provider will be able to discuss these with you and come up with a tailored plan for treatment. But since knowledge is power, here’s the lowdown on the most commonly available treatments for fibroids that can also preserve your fertility:
Myomectomy
A myomectomy involves removing fibroids from the uterus. There are three main ways of doing a myomectomy.
Hysteroscopic myomectomy
This procedure is considered to be minimally invasive. It involves inserting a hysteroscope (a narrow telescope with a light and camera that removes fibroid tissue) into the uterine cavity through the vagina and cervix, so no incisions are made. However, it’s only possible if you have submucosal fibroids.
Laparoscopic myomectomy
This procedure involves the fibroids being removed through small cuts made in your abdomen.
Abdominal myomectomy
This procedure also involves the fibroids being removed from your abdomen, but through larger cuts than in a laparoscopic myomectomy. Your doctor might recommend this if you have large fibroids, more than one fibroid, or if the fibroid has grown deep in the uterus.
How uterine fibroids may affect pregnancy
If you’re pregnant with fibroids, some possible complications can arise. These can sound frightening, so be sure to discuss any concerns with your doctor. They will be able to offer advice and answer any questions you may have, while developing a plan to closely monitor the fibroids during your pregnancy.
The complications can include:
- Placental abruption: This occurs when the placenta comes away from the wall of the uterus. One study found that this is three times more likely to happen when the pregnant person has fibroids.
- Preterm delivery: This is when you give birth before 37 weeks. One study found that women with fibroids have a 16% risk of this occurring, compared to women without fibroids, who have a 10% risk.
How are uterine fibroids treated during pregnancy?
First things first: As we’ve seen, 75% of women will go on to have a safe and healthy pregnancy after treating their fibroids with a myomectomy.
That being said, it’s possible that you could experience some of the complications listed above. If that happens, your doctor will be able to discuss your options with you and hopefully find a treatment plan that works for you.
There are a few treatment options available for fibroids during pregnancy. If they’re causing you a lot of pain, you might be prescribed certain medications to help relieve this.
Rarely, you might also be offered a myomectomy to remove the fibroid or fibroids. However, it’s worth noting that such surgeries are almost always avoided during pregnancy.
More FAQs
What do uterine fibroids look like?
Fibroids typically look like round growths. Pedunculated fibroids are attached to the uterus by a stalk or stem, giving them a mushroom-like appearance. Fibroids can range in number and size from a single nodule to a cluster of multiple growths.
Are uterine fibroids cancerous?
Uterine fibroids are benign growths, which means they are noncancerous. Having benign fibroids does not increase your risk of developing a cancerous fibroid or any other type of cancer.
Do fibroids grow after menopause?
It is extremely rare for fibroids to grow after menopause, with one study finding that only 0.5% of women developed a fibroid after menopause.
This is because fibroid growth is linked to hormones, and as hormone levels decline during menopause, fibroids will shrink rather than grow during this time. The good news is that any symptoms should also improve, too.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Eggert, Stacey L., et al. “Genome-Wide Linkage and Association Analyses Implicate FASN in Predisposition to Uterine Leiomyomata.” American Journal of Human Genetics, vol. 91, no. 4, Oct. 2012, pp. 621–28, www.cell.com/ajhg/fulltext/S0002-9297(12)00421-1.
Eltoukhi, Heba M., et al. “The Health Disparities of Uterine Fibroid Tumors for African American Women: A Public Health Issue.” American Journal of Obstetrics and Gynecology, vol. 210, no. 3, Mar. 2014, pp. 194–99, www.ncbi.nlm.nih.gov/pmc/articles/PMC3874080/.
“Fibroids.” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/uterine-fibroids. Accessed 20 Dec. 2023.
“Fibroids: Complications.” NHS, www.nhs.uk/conditions/fibroids/. Accessed 3 Aug. 2023.
“Fibroids: Diagnosis.” NHS, www.nhs.uk/conditions/fibroids/diagnosis/. Accessed 3 Aug. 2023.
“Fibroid Locations.” Mayo Clinic, www.mayoclinic.org/diseases-conditions/uterine-fibroids/multimedia/fibroid-locations/img-20006761. Accessed 11 Jan. 2024.
“Fibroids: Overview.” NHS, www.nhs.uk/conditions/fibroids/complications/. Accessed 3 Aug. 2023.
“Fibroids: Treatment.” NHS, www.nhs.uk/conditions/fibroids/treatment/. Accessed 3 Aug. 2023.
Freytag, Damaris, et al. “Uterine Fibroids and Infertility.” Diagnostics, vol. 11, no. 8, Aug. 2021, https://doi.org/10.3390/diagnostics11081455.
Khaw, Shen Chuen, et al. “Systematic Review of Pregnancy Outcomes after Fertility-Preserving Treatment of Uterine Fibroids.” Reproductive Biomedicine Online, vol. 40, no. 3, Mar. 2020, pp. 429–44, www.rbmojournal.com/article/S1472-6483(20)30003-1/fulltext.
Lai, Jasmine, et al. “Neonatal Outcomes in Women with Sonographically Identified Uterine Leiomyomata.” The Journal of Maternal-Fetal and Neonatal Medicine, vol. 25, no. 6, June 2012, pp. 710–13, pubmed.ncbi.nlm.nih.gov/22409539/.
Lee, Hee Joong, et al. “Contemporary Management of Fibroids in Pregnancy.” Reviews in Obstetrics and Gynecology, vol. 3, no. 1, 2010, pp. 20–27, www.ncbi.nlm.nih.gov/pmc/articles/PMC2876319/.
“Planning for Pregnancy When You Have Fibroids.” The University of Chicago Medicine, www.uchicagomedicine.org/conditions-services/obgyn/uterine-fibroids/pregnancy-fertility. Accessed 20 Dec. 2023.
“Uterine Artery Embolisation for Fibroids.” National Institute for Health and Care Excellence, 24 Nov. 2010, www.nice.org.uk/guidance/ipg367.
“Uterine Fibroids.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/9130-uterine-fibroids/. Accessed 3 Aug. 2023.
“Uterine Fibroids.” Mayo Clinic, 15 Sep. 2023, www.mayoclinic.org/diseases-conditions/uterine-fibroids/symptoms-causes/syc-20354288.
“Uterine Fibroids.” The American College of Obstetricians and Gynecologists, July 2022, www.acog.org/womens-health/faqs/uterine-fibroids.
“Radiofrequency Ablation for Pain Management.” Cleveland Clinic, my.clevelandclinic.org/health/treatments/17411-radiofrequency-ablation. Accessed 3 Aug. 2023.
“Removal of Myomas in Asymptomatic Patients to Improve Fertility and/or Reduce Miscarriage Rate: A Guideline (2017).” American Society for Reproductive Medicine, www.asrm.org/practice-guidance/practice-committee-documents/removal-of-myomas-in-asymptomatic-patients-to-improve-fertility-andor-reduce-miscarriage-rate-a-guideline-2017/. Accessed 20 Dec. 2023.
Sommer, Eva M., et al. “Effects of Obesity and Hormone Therapy on Surgically-Confirmed Fibroids in Postmenopausal Women.” European Journal of Epidemiology, vol. 30, no. 6, June 2015, pp. 493–99, www.ncbi.nlm.nih.gov/pmc/articles/PMC4485678/.
Stewart, E. A., et al. “Epidemiology of Uterine Fibroids: A Systematic Review.” BJOG: An International Journal of Obstetrics and Gynaecology, vol. 124, no. 10, Sep. 2017, pp. 1501–12, pubmed.ncbi.nlm.nih.gov/28296146/.
“What to Know about Uterine Fibroids after Menopause.” Cleveland Clinic, 24 June 2022, health.clevelandclinic.org/uterine-fibroids-after-menopause.
History of updates
Current version (12 January 2024)
Published (27 December 2018)
In this article
Get your personal guide to fertility
-
Learn how to read your body's ovulation signals
-
Find daily conception tips from our experts
-
Chat with others who are trying to get pregnant




