-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Heavy Menstrual Bleeding: Why Is My Period So Heavy?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
As if mood swings, cramps, backache, and headaches weren’t enough to make your period your least favorite time of the month, there’s also the blood loss.
Because we are all so different, our periods are too. Some of us have a heavy start to our period which then tails off, while others have heavy or light bleeding throughout. Period length also varies from person to person. And 25% of women and people who menstruate have blood loss so severe that it’s categorized as heavy menstrual bleeding (HMB).
Here, we’ll explain what HMB actually is and discuss the signs, symptoms, and causes. If you’re suffering from HMB, take comfort in the fact that there are plenty of treatment options available that can hopefully provide you with some relief.
Take a quiz
Find out what you can do with our Health Assistant
What is considered heavy menstrual bleeding?
HMB, which used to be called “menorrhagia,” is prolonged or excessive heavy bleeding during periods that can be so bad it can interfere with your daily life. It can be nerve-wracking when you’re just not sure why your periods are so heavy, and HMB can make you dread getting your period each month.
If you have HMB, your menstrual flow can be heavy enough to require changing your pad or tampon every hour for several hours in a row. You might also have cramps so severe it makes it difficult to do your usual daily activities. It can be hard to go to work, play sports, or even socialize because you’re in pain or worrying about leaking.
It’s important to remember that HMB can affect anyone, and nothing you have done is causing this heavy bleeding. Though the causes can’t always be determined, it’s important to be aware of the condition because it could be happening as a result of an underlying issue. For example, HMB has been linked to iron-deficiency anemia, which can make you feel exhausted and short of breath, so figuring out if you have it can help you manage how you’re feeling.
How can you tell if you have heavy menstrual bleeding?
There are some common symptoms and signs that may indicate your flow is heavy, so if you’re experiencing one or more of the below, it’s possible you might have HMB:
- You soak through one or more tampons or pads an hour for several hours in a row.
- You have to use two kinds of period products, like a tampon and a pad at the same time.
- You have to get up at night to change your period products.
- Your periods last longer than seven days.
- You pass blood clots that are 1 inch (2.5 centimeters) or larger during your periods.
- Your periods soak through your bedding or clothes.
- You have to restrict your everyday activities because of heavy menstrual bleeding.
- You experience symptoms and signs of iron-deficiency anemia, including shortness of breath, fatigue, or tiredness.
The average person loses between 30 and 40 milliliters, or two to three tablespoons, of blood during menstruation. However, people suffering from HMB can lose up to 80 milliliters each month.
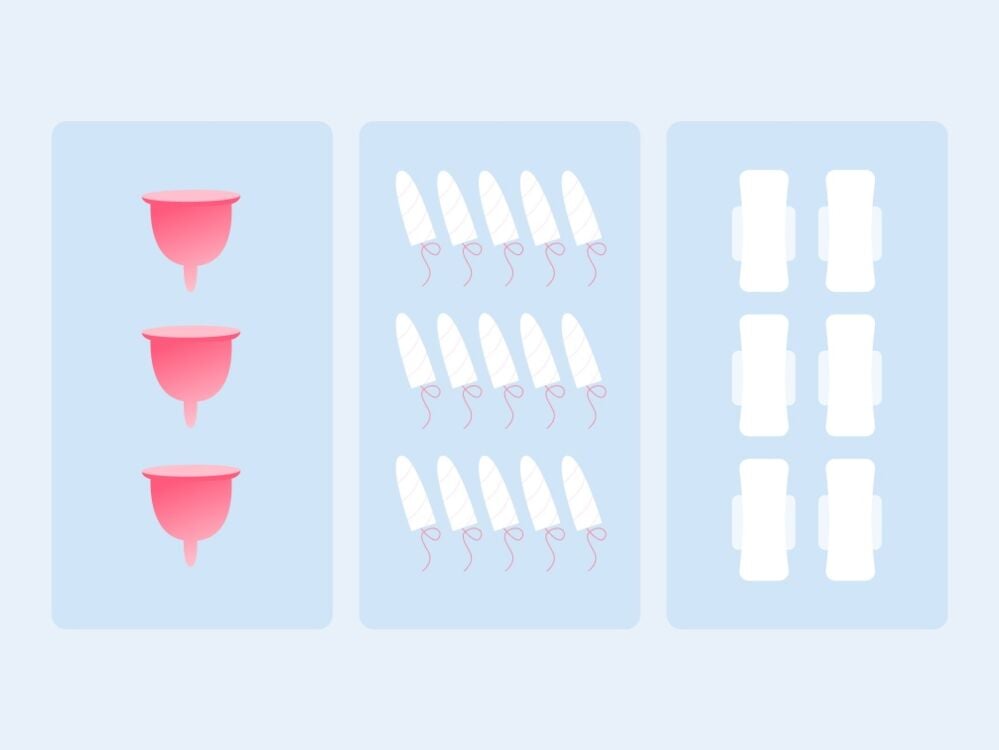
To give you an idea of how much 80 milliliters is, a menstrual cup can hold up to around 30 milliliters of menstrual blood; a regular-absorbency tampon absorbs up to five milliliters; and a standard pad absorbs about 15 milliliters.
Measuring blood loss can be tricky because your menstrual fluid also contains a mix of mucus and uterine tissues, which can add to the volume of your overall fluid loss. One way to work out if you have HMB is to measure your flow. Speak to your health care professional about the best way to do this.
What causes heavy menstrual bleeding?
There are a variety of factors that can cause heavy menstrual bleeding, including age. These are some of the most common:
- Hormonal imbalance: Hormonal imbalance caused by things like obesity, polycystic ovarian syndrome (PCOS), thyroid problems, and insulin resistance can cause excess buildup of your endometrial lining, which is then shed as heavy menstrual bleeding.
- Polyps: These tiny benign growths are sometimes present in the uterine cavity and cervical canal.
- Uterine fibroids: These benign (noncancerous) tumors present in the uterus and may appear during the childbearing years. They can cause HMB.
- Adenomyosis: This is when the inner lining of the uterus embeds in the muscles of the uterus, which can cause HMB.
- Intrauterine device (IUD) or coil: HMB is one of the common side effects of using a non-hormonal intrauterine device.
- Complications of pregnancy: Sometimes a single epidose of HMB is the result of a miscarriage or ectopic pregnancy.
- Cancer: Cancers of the uterus and cervix can both cause HMB, especially in perimenopausal people.
- Bleeding disorders: HMB can sometimes be a side effect of von Willebrand’s disease (a disorder in which there is a deficiency or impairment of an essential blood-clotting factor).
- Medicines: Certain medicines — including anticoagulants (for example, warfarin), anti-inflammatory medicines, and hormonal medicines such as progestins and estrogen — can sometimes cause HMB.
- Other medical conditions: HMB may occur along with various other medical conditions, including pelvic inflammatory disease (PID) and kidney, thyroid, and liver disease.
Treatment: How to stop heavy menstrual bleeding
If you think you might have HMB, make an appointment to see your health care professional for a checkup. Often, they’ll ask you questions about your periods and general health. They might also perform a physical examination.
After this, they’ll be able to suggest a variety of treatments to help, which can include:
Medications
Your health care provider may prescribe tranexamic acid to stop clots from breaking down after they’re formed. The contraceptive pill could also help regulate your menstrual cycles and reduce prolonged or heavy menstrual bleeding, and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may help reduce blood loss and relieve painful cramps.
Iron supplements may also be prescribed if you develop signs and symptoms of anemia.
A hormonal intrauterine device may also help reduce blood loss and cramping because it releases a type of progesterone that affects the lining of the uterus.
Procedures
There are several medical procedures that can be prescribed to manage HMB in certain cases. Your doctor will take into account your age and medical history when prescribing these:
Dilation and curettage (D&C): This is a surgical procedure that removes the topmost layer of the endometrium (the lining of your uterus) to reduce heavy menstrual bleeding.
Endometrial resection or ablation: In these two procedures, some or all of the uterine lining is removed utilizing different techniques to control heavy menstrual bleeding.
Operative hysteroscopy: In this surgical procedure, a specialized tool makes it possible to see the uterus from the inside in order to remove fibroids and polyps, correct uterine abnormalities, and remove the uterine lining to control HMB.
Hysterectomy: This is a major surgical procedure where the whole uterus is removed. After this procedure, you won’t be able to get pregnant and won’t get periods. Hysterectomy is used in very rare cases and only when other methods don’t work.
Heavy menstrual bleeding – The takeaway
Heavy menstrual bleeding can be frustrating and difficult to live with. But once you figure out if you have it, there are plenty of options available to help you manage the pain and side effects.
If your periods are making life difficult every month, make an appointment with your doctor. They will be able to help you put a plan in place.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Magnay, Julia L et al. “Pictorial methods to assess heavy menstrual bleeding in research and clinical practice: a systematic literature review.” BMC women’s health vol. 20,1 24. 10 Feb. 2020, doi:10.1186/s12905-020-0887-y. Accessed Dec. 1.
“Heavy Menstrual Bleeding.” Centers for Disease Control and Prevention, 20 Dec. 2017, www.cdc.gov/ncbddd/blooddisorders/women/menorrhagia.html. Accessed Dec. 1.
“Menorrhagia (Heavy Menstrual Bleeding).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 1 July 2020, www.mayoclinic.org/diseases-conditions/menorrhagia/diagnosis-treatment/drc-20352834. Accessed Dec. 1.
“Heavy Periods.” NHS Choices, NHS, 7 June 2018, www.nhs.uk/conditions/heavy-periods/. Accessed Dec. 1.
Herman, Malou C et al. “Diagnosis of heavy menstrual bleeding.” Women’s health (London, England) vol. 12,1 (2016): 15-20. doi:10.2217/whe.15.90. Accessed Dec. 1.
“Heavy Periods: Overview.” InformedHealth.org [Internet]., U.S. National Library of Medicine, 4 May 2017, www.ncbi.nlm.nih.gov/books/NBK279294/. Accessed Dec. 1.
Holland, Kimberly. “How Much Blood Do You Lose on Your Period?” Healthline, 31 May 2018, www.healthline.com/health/how-much-blood-do-you-lose-on-your-period. Accessed Dec. 1.
Magnay, Julia L et al. “A systematic review of methods to measure menstrual blood loss.” BMC women’s health vol. 18,1 142. 22 Aug. 2018, doi:10.1186/s12905-018-0627-8. Accessed Dec. 1.




