A Flo expert shares why endometriosis can make ovulation pain worse and the best treatment options for relieving discomfort.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Does endometriosis cause ovulation pain?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Ovulation is a big moment in your menstrual cycle. It’s when your ovaries release an egg into your uterine (or fallopian) tubes. The majority of people don’t notice ovulation happening, but for up to 40% of us, egg release can lead to pain or discomfort called mittelschmerz.
Ovulation pain is usually mild, but it can sometimes indicate a health condition like endometriosis. Here, fertility doctor Dr. Tiffany Jones from Texas, US, shares what you need to know about the link between endometriosis and ovulation pain.
Key takeaways
- Up to 4 in 10 of us experience ovulation pain, or mittelschmerz. Our ovaries releasing an egg can sometimes cause a little discomfort, but in most people, the pain is usually mild, and it should be over within 48 hours.
- Ovulation pain, especially if it’s long-lasting or severe, can sometimes indicate a health condition like endometriosis. Although endometriosis is associated with painful periods, it can cause pain at other points in your cycle, too.
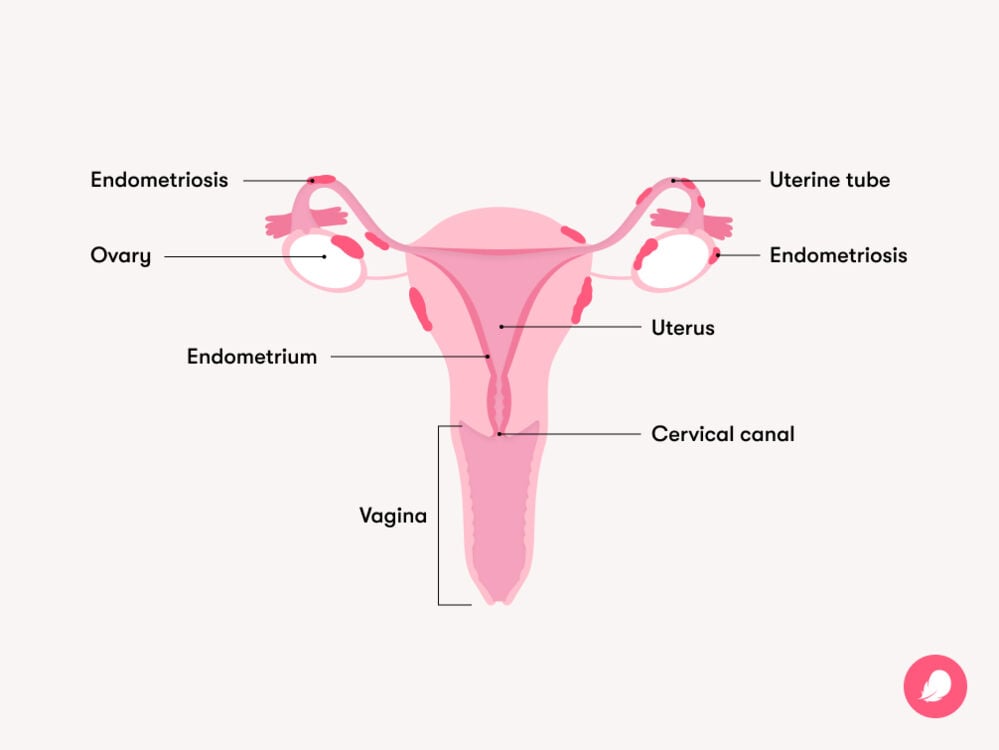
- Endometriosis happens when tissue like the lining of your uterus grows in other places in the body. Because this tissue responds to the hormones that control your menstrual cycle, it can lead to inflammation, pain, and swelling as your hormone levels change.
- If pain is getting in the way of your life — wherever it occurs in your cycle — see your doctor. You don’t need to just live with it.
- A cycle-tracking app like Flo can help you log symptoms like cramping or pain so you can see if there’s a pattern around when they happen in your cycle.
Why endometriosis can cause ovulation pain
Endometriosis affects around 1 in 10 of us. It’s a condition where tissue similar to the lining inside your uterus (called the endometrium) grows in places it doesn’t usually, like your ovaries or uterine tubes. It’s often associated with painful periods and pelvic pain and can sometimes make getting pregnant more difficult — though there are lots of treatment options.
“As the endometriosis is under exactly the same hormonal control as your uterus, it can cause tremendous inflammation and lead to bloating and cramping,” explains Dr. Jones.
And these symptoms might not be confined to when you have your period, she adds. Some people with endometriosis notice pain when they ovulate, too.
Ovulation pain might happen with endometriosis because:
- Endometriosis can lead to inflammation in your pelvis. That’s because there is endometrial-like tissue in your pelvis that shouldn’t be there. When ovulation occurs, the tissue can flare up, which can further irritate this already sensitive area and cause pain.
- Endometriosis can sometimes cause scar tissue to form between organs (called adhesions). During ovulation, the natural movement of your ovaries and uterine tubes can tug on these adhesions, resulting in sharp pain.
- Endometriosis can lead to the formation of blood-filled cysts on the ovaries, known as endometriomas or “chocolate cysts.” These cysts can cause the ovaries to enlarge and become tender. And ovulation can aggravate these cysts, too.
Where you might feel pain caused by endometriosis
Endometriosis pain can be really different from one person to the next, which is part of what makes the condition tricky to diagnose, says Dr. Jones. But her patients often describe the pain in a few different ways.
“Most of the time when I talk to patients, especially when they have confirmed endometriosis, it can be a sharp, ongoing, very intense pain and can even lead to nausea and vomiting,” she says. “But others describe it as a low, cramping-type pain.”
You’re most likely to feel endometriosis pain in your lower belly or back. But some people with endometriosis feel pain in other places like their bowel, chest, neck, or diaphragm, depending on where the endometriosis might be growing.
Where you feel pain could be a clue as to where the condition has developed, says Dr. Jones. So, tell your doctor as much as you can about the type of pain you’re feeling and where you’re feeling it.
Take a quiz
Find out what you can do with our Health Assistant
Signs that ovulation pain might be caused by endometriosis
Ovulation pain tends to be mild and typically only lasts up to 48 hours. You might notice a dull, nagging, cramping pain on one side of your body that starts halfway through your menstrual cycle.
But ovulation pain due to endometriosis might be more severe and last longer than a couple of days. Other signs of endometriosis can include:
- Painful or heavy periods
- Painful sex
- Pain when you pee
- Pain when you poop
- Pain accompanied by vomiting or diarrhea
It’s always best to see your doctor if you’re concerned you might have endometriosis.
How to ease the pain of endometriosis
While endometriosis can be debilitating, there are lots of things you can do to take control of the pain. Managing endometriosis often requires a few different approaches and should always be guided by your doctor, but there are plenty of options that can relieve discomfort, says Dr. Jones. Your health care provider can recommend a treatment for endometriosis that best suits your needs if you do have the condition. Here are some of the pain relief options they might suggest:
Over-the-counter medication
“Typically, we’d recommend anti-inflammatory pain relievers as first-line treatment for endometriosis,” says Dr. Jones. Medicines like ibuprofen and naproxen can relieve pain and inflammation caused by endometriosis. But check with your doctor first whether they’re right for you because they may not be suitable for everyone.
Self-care
Being gentle with yourself is also really important if you have endometriosis, but some people find light exercise (think yoga or a walk) can help with the pain. You might find taking a warm bath or applying a heating pad to your belly or back provides relief, too.
Medical options
There are lots of treatment options your doctor might recommend, such as prescription pain relief, birth control, or hormonal therapy that puts a pause on your cycle. “I have endometriosis patients who do not have pain when they’re on birth control or medicines that shut down their cycle completely,” says Dr. Jones. But only your health care provider can tell you what might be suitable for you, so schedule an appointment to discuss your options.
Medications can be really helpful for endometriosis. But in more severe cases, your doctor might recommend surgery for endometriosis. If this is suggested for you, you’ll be given plenty of space to learn more about what the procedure would involve so you can make a decision on whether it’s the right route for you.
When to see a doctor
The bottom line is that pain that gets in the way of your life isn’t normal. Although ovulation pain is quite common, it’s always worth telling your doctor about it if:
- The pain is severe or lasts more than a couple of days
- Ovulation pain is getting in the way of your normal day-to-day activities
- You have pain during sex or when you pee or poop
Even if you don’t think you’re experiencing problems with periods and ovulation, Dr. Jones recommends scheduling an annual check-up with your obstetrician and gynecologist. They’ll be able to tell you if what you’re experiencing is typical or not and whether you have any signs of a health condition that might need treating.
“The conversation should always be open to any concerns that you have,” she says. “Some people experience painful periods and think that’s how it’s supposed to be and never say anything because they have an internal barometer that this is normal. But it’s not.”
Frequently asked questions about endometriosis and ovulation pain
When is endometriosis most painful during your menstrual cycle?
Endometriosis is most commonly linked with pelvic pain and painful periods. Endometriosis pain often peaks during — and just before — your period. But it can also flare up around ovulation and linger throughout the cycle because of hormonal changes and inflammation, says Dr. Jones.
Keeping track of your symptoms using an app like Flo can help you spot what’s usual for you throughout your cycle — and give you the information you need to have a confident conversation with your doctor about your health.
Can endometriosis cause an upset stomach during ovulation?
Although diarrhea isn’t a recognized symptom of ovulation, it’s possible to experience bowel symptoms during ovulation, as hormonal changes can also impact our gut. Hormone-like substances called prostaglandins play a key role in ovulation. And some links have been made between prostaglandins and an upset stomach — though there’s more evidence for this happening during your period rather than at ovulation.
Endometriosis can also impact your gut throughout your cycle as it might grow near your bowel. Pain when you poop is a possible symptom of endometriosis, so it’s always worth mentioning to your doctor.
How do gynecologists check for endometriosis?
Only a health care provider can diagnose endometriosis. An obstetrician and gynecologist will likely start with a physical exam, including a pelvic exam. But the only way to confirm for sure that it’s endometriosis is through a keyhole surgical procedure called laparoscopy. That’s when a thin telescope is inserted through a small cut in your belly. It gives doctors a clear view of your pelvic organs so they can see if there’s any endometriosis in that area.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Armour, Mike, et al. “Exercise for Dysmenorrhoea.” Cochrane Database of Systematic Reviews, vol. 9, no. 9, Sep. 2019, doi:10.1002/14651858.CD004142.pub4.
Brott, Nathan R., and Jacqueline K. Le. “Mittelschmerz.” StatPearls, StatPearls Publishing, 2023, www.ncbi.nlm.nih.gov/books/NBK549822/.
Drabble, Sarah J., et al. “Constellations of Pain: A Qualitative Study of the Complexity of Women’s Endometriosis-Related Pain.” British Journal of Pain, vol. 15, no. 3, Aug. 2021, pp. 345–56, doi:10.1177/2049463720961413.
“Endometriosis.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/10857-endometriosis. Accessed 5 Sep. 2024.
“Endometriosis.” Mayo Clinic, 30 Aug. 2024, www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656.
“Endometriosis.” NHS, www.nhs.uk/conditions/endometriosis/. Accessed 5 Sep. 2024.
“Endometriosis.” The American College of Obstetricians and Gynecologists, Feb. 2021, www.acog.org/womens-health/faqs/endometriosis.
“Here’s the Deal with Period Poops.” Cleveland Clinic, 29 Oct. 2021, health.clevelandclinic.org/why-do-you-poop-more-on-your-period.
Maddern, Jessica, et al. “Pain in Endometriosis.” Frontiers in Cellular Neuroscience, vol. 14, Oct. 2020, https://doi.org/10.3389/fncel.2020.590823.
Nezhat, Camran, et al. “Optimal Management of Endometriosis and Pain.” Obstetrics and Gynecology, vol. 134, no. 4, Oct. 2019, pp. 834–39, doi:10.1097/AOG.0000000000003461.
“Ovarian Endometrioma.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/22004-ovarian-endometrioma. Accessed 5 Sep. 2024.
“Ovulation Pain.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/9134-ovulation-pain-mittelschmerz. Accessed 15 Aug. 2024.
“Ovulation Pain.” NHS, www.nhs.uk/conditions/ovulation-pain/. Accessed 17 Feb. 2023.
“Painful Periods.” The American College of Obstetricians and Gynecologists, Oct. 2020, www.acog.org/womens-health/faqs/painful-periods.
“Prostaglandins.” Cleveland Clinic, https://my.clevelandclinic.org/health/articles/24411-prostaglandins. Accessed 5 Sep. 2024.
“Where Can You Feel Endometriosis Pain?” Cleveland Clinic, 27 June 2022, health.clevelandclinic.org/endometriosis-pain.




