From heating pads to surgery, there are lots of ways you can manage endometriosis. Here’s everything you need to know so you can make the right choices for yourself.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
The different endometriosis treatment options explained

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Endometriosis — it’s a pretty long name for a condition that affects around one in 10 women of reproductive age worldwide. That’s why you might have heard some people call it “endo” for short. That being said, you may not know much about this common gynecological condition or what the treatment options are for it, and that’s totally understandable.
One of the main symptoms associated with endometriosis is painful periods, but there are a number of treatment options out there that may help you manage these. Choosing the right option for you is really personal — depending on whether you want to become pregnant in the future and how severe your endometriosis is. Keep reading to learn all about the different endometriosis treatments.
What is endometriosis?
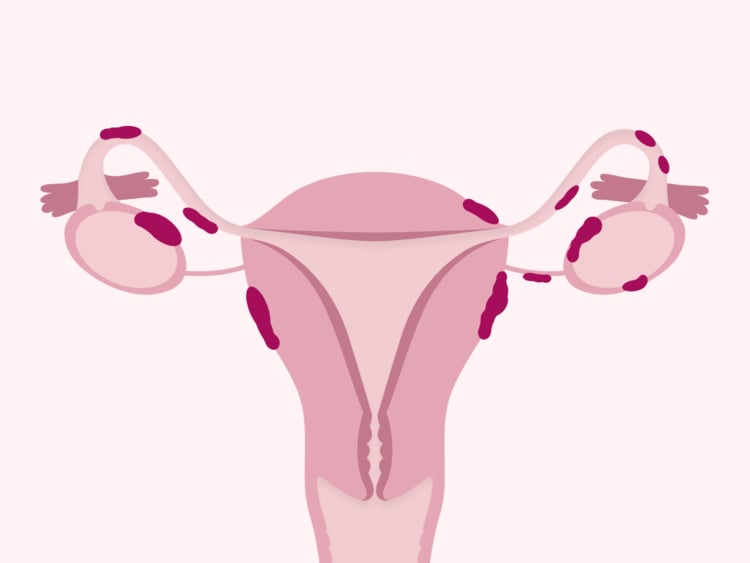
Before you learn about all the treatment options for endometriosis, it’s good to understand what it actually is. Endometriosis is a chronic condition (this means that the symptoms are persistent or long-lasting) where tissue similar to the lining of the uterus (sometimes called the endometrium) starts to grow in other places in the body. This tissue can grow on other reproductive organs like your ovaries and uterine (or fallopian) tubes, or sometimes it can spread further — growing on your bowels, rectum, and bladder. Less commonly, endometriosis tissue can also grow on other organs like your lungs and kidneys.
Just as the lining of your uterus reacts to fluctuations in your hormones (it builds up during your menstrual cycle and then falls away during your period), the endometrial tissue behaves in a similar way. It thickens, but when it falls away, it has no way of leaving your body. This can cause inflammation, swelling, and lesions, and your body reacts to this by releasing prostaglandins (which are hormone-like substances) that can cause severe pain. You can learn more about endometriosis using an app like Flo.
Painful periods are just one symptom associated with endometriosis, and they aren’t easy to live with. They aren’t just “normal” period cramps, and there are lots of different ways of treating endometriosis. Other symptoms linked to endometriosis include:
- Pain during or after sex
- Heavy periods
- Spotting and bleeding when you’re not on your period
- Difficulty conceiving
- Painful bowel movements
- Chronic fatigue
The many varied symptoms of endometriosis mean that it’s not always easy to diagnose. It’s estimated that it takes between eight and 12 years to diagnose endometriosis, but when you do have a diagnosis, you can start talking to your doctor about the treatment options that may best suit you.
Take a quiz
Find out what you can do with our Health Assistant
Endometriosis treatment options
Like other conditions, there’s no one-size-fits-all treatment for endometriosis, and what might be best for you will be totally different for someone else. It all depends on whether you want to get pregnant in the future and how severe your endometriosis is.
“Endometriosis isn’t difficult to treat for everyone. Most patients do well with traditional treatments, and advances in medicine have increased the response to medication,” says Dr. Allison Rodgers, obstetrician and gynecologist and reproductive endocrinologist, Fertility Centers of Illinois, US. There are a number of different ways you might manage your symptoms.
Hormone therapy
You might already know that you can take birth control to prevent pregnancy, but it can also be a way to treat conditions like endometriosis. Dr. Rodgers explains that hormone therapy is one of the most effective ways that you can treat endometriosis, and it may be the first thing your doctor suggests. It works by blocking or reducing the production of estrogen, which in turn reduces endometrial tissue growth.
Hormone therapy for endometriosis can come in different forms. These include:
- Birth control that has a combination of estrogen and progesterone, such as the pill. This works by suppressing ovulation and preventing periods.
- Birth control that only contains progestin (a synthetic version of progesterone), such as the hormonal coil. This works by making periods lighter or stopping them altogether.
- Gonadotropin-releasing hormone analogs — a medication that stops the hormone center of your brain (called the pituitary gland) from making follicle-stimulating hormone and luteinizing hormone, which in turn causes the ovaries to stop making estrogen and progesterone.
- Medication that contains hormones similar to testosterone (called androgens), which decrease the production of estrogen and progesterone, in turn decreasing the growth of endometriosis tissue.
Surgical treatments
If your endometriosis is more widespread or you have more severe symptoms, your doctor might suggest that you consider a surgical treatment option. This might sound daunting, but try not to worry. A number of different procedures are used to diagnose and manage endometriosis, and they range from being very minimally invasive to more extensive. You don’t need to know the ins and outs of each procedure before speaking to your doctor — they should be able to answer all of your questions and walk you through what each involves. Here’s a brief overview of some surgical treatments for endometriosis:
- Laparoscopy: Laparoscopic surgery is the most common surgical option used to both diagnose and treat endometriosis. It’s sometimes called keyhole surgery as it involves making small incisions in your abdomen and inserting a tiny tube with a light and camera (this is the laparoscope). Your doctor will then be able to see where you have endometrial tissue and may even be able to remove it by burning it off (known as fulguration or ablation) or cutting it out (excision). As this procedure shouldn’t impact your reproductive organs, you should still be able to get pregnant in the future. This is sometimes called a fertility-sparing option.
- Laparotomy: This procedure is similar to laparoscopy but involves making a bigger incision in the abdomen so your doctor can remove the endometrial tissue. Laparotomies are also classed as fertility-sparing.
- Hysterectomy: This is a more invasive surgery when your uterus is removed. In some other cases, you may also have your uterine tubes and your ovaries removed too. It’s classed as a treatment option as you’re removing the organs where the endometrial tissue is growing. However, your doctor should only present this as an option if you don’t want to be pregnant in the future, as you won’t be able to carry a baby after having a hysterectomy.
Whether you’re looking at keyhole surgery or a hysterectomy, all surgery can feel scary. Dr. Rodgers explains that you should feel totally supported by your health care professional. “If your doctor is recommending surgery, ask why, and it’s never a bad idea to get another opinion about management options if you have questions or your gut is telling you something different,” she says.
Pain medication to manage chronic pain
While hormone therapies and surgery can help to manage the growth of your endometriosis, your doctor might also suggest different medicines which may help you to manage the symptoms associated with endometriosis.
Endometriosis can cause pain that ranges from uncomfortable to debilitating, and it can really impact your quality of life, so finding a pain management treatment is really important. Pain management for endometriosis varies depending on the severity of your symptoms, but they can include:
- Non-steroidal anti-inflammatory drugs that can reduce pain and inflammation
- Over-the-counter painkillers
- Stronger prescription painkillers for severe cases

Nonmedical therapies and at-home remedies
Currently, there aren’t any nonmedical therapies presented in the standard treatment options for endometriosis. There isn’t a lot of research into how exercise or lifestyle changes may help you manage your symptoms, although some studies have looked into how heating pads may alleviate some of your symptoms.
There also isn’t much research into the benefits of using supplements to treat the symptoms of endometriosis, so the best thing to do before you start any new medication or supplement is to speak to your doctor. Similarly, you might have read online that your diet can help manage and treat endometriosis symptoms. Although your overall diet can impact your general wellbeing, there’s no real evidence to show that diet can improve endometriosis.
“Unfortunately, there is no science that says a specific diet will help endometriosis,” adds Dr. Rodgers. “While we don’t understand everything yet about endometriosis, estrogen, or more specifically, the ratio of estrogen to progesterone, can fuel the growth of endometriosis. Some patients want to try cutting out other ‘inflammatory foods’ such as gluten, dairy, or sugars and may feel better, but there is no science that supports cutting foods out or having a specific diet.”
How to decide which treatment is the best for you
There’s a lot to consider before you start any new treatment, but you’re not alone. “Your doctor should put together a treatment plan that is individualized to your needs. This is a personal discussion with your doctor to decide if medicine is right for you and what type. Often, we try to minimize side effects and maximize outcomes. It’s often a bit of trying different things to see what works for you,” explains Dr. Rodgers. “Typically, patients start with hormonal medications like birth control pills as this is often successful without many side effects.”
Advocating for yourself in a medical environment can feel scary, but your doctor is on your side. If you don’t feel fully listened to or supported, then don’t be afraid to seek a second opinion. Finding a way to manage your endometriosis should feel like a team effort, and your doctor should be there to give you the guidance and support you need. And you can use an app like Flo to understand more about endometriosis, too.
Can endometriosis be cured completely?
When you’re exploring the different treatment options for endometriosis, your doctor should explain that while it may improve your quality of life and slow down the growth of your endometriosis, it won’t cure it altogether. This is because, right now, endometriosis can’t be cured completely as the cause of the condition is still unknown. However, researchers are working to change this.
What happens if endometriosis is left untreated, and will it go away by itself?
Now that you know the different treatment options for endometriosis, you might be curious as to what happens if you don’t treat the condition at all. While you should never feel rushed into making a decision about which treatment option may be right for you, Dr. Rodgers explains that if left untreated, endometriosis can “increase risks of scar tissue, damage pelvic organs such as ovaries, and increase pain.”
You might have heard that the condition can go away on its own, and Dr. Rodgers says that can happen in one case — when you reach menopause. “When the ovaries run out of eggs and more or less go to sleep, symptoms improve,” she says. “This stops the menstrual cycle and lowers estrogen and progesterone hormones, and endometriosis has no more fuel to grow and goes away.” However, it’s so important that you don’t wait to access the treatment you need.
Can you get pregnant if you have endometriosis?
The idea that endometriosis can cause scar tissue on your reproductive organs may particularly worry you if you’d like to become pregnant in the future. You’re absolutely not alone in wondering how the condition may impact your fertility. Dr. Rodgers explains that, “many people with endometriosis get pregnant.” It’s estimated that 60% to 70% of people with endometriosis will go on to have children without using fertility treatment. However, for other people, it can be a little bit more complicated.
Scar tissue from endometriosis could damage the organs involved in conception, such as your uterus, ovaries, and uterine tubes, and it may also block sperm from reaching the egg. While this may sound incredibly disheartening, you shouldn’t lose hope, and your doctor will be able to outline all of your fertility options.
Fertility treatment related to endometriosis
If you’re trying to have a baby and you have endometriosis, then there are lots of things you can do. Your doctor will be able to explain what assisted reproductive technologies (ART) are — such as intrauterine insemination or in vitro fertilization (IVF).
IVF may be a really good option for you if you have endometriosis. One study found that after one to four IVF treatments, including frozen embryo transfer, almost 70% of women with stage one or two endometriosis were pregnant. In addition, more than half of women with stage three to four endometriosis were pregnant (compared to around 80% of women without endometriosis).
When you start to explore the different fertility treatment options, it can feel really daunting, and there can be a number of barriers, such as cost and access to clinics. If you aren’t sure if ART is for you, then don’t be afraid to speak to your doctor. They may refer you to a specialist to answer all of your questions, so you can make the best decision for you.
Endometriosis treatment: The takeaway
While there currently isn’t a total cure for endometriosis, there are a number of treatment options that may help you manage your symptoms and improve your quality of life. When you’re presented with a long list of options, it’s easy to feel daunted, but don’t worry. Your doctor should work with you every step of the way to figure out which is best for you based on the symptoms you have, how widespread your endometriosis is, and if you want to get pregnant in the future.
You can learn more about endometriosis and the symptoms associated with it using an app like Flo, and it’s so important to remember that the pain you’re experiencing isn’t something you just have to “put up with.” Endometriosis pain isn’t the same as normal period cramps, and you know your body best. Understanding some of your treatment options may help you to feel a little bit more in control as you advocate for yourself in your doctor’s office.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Bulletti, Carlo, et al. “Endometriosis and Infertility.” Journal of Assisted Reproduction and Genetics, vol. 27, no. 8, Aug. 2010, pp. 441–47.
“Endometriosis.” Mayo Clinic, 24 July 2018, www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656.
“Endometriosis.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/10857-endometriosis. Accessed 28 Mar. 2023.
“Endometriosis.” The American College of Obstetricians and Gynecologists, www.acog.org/womens-health/faqs/endometriosis. Accessed 28 Mar. 2023.
“Endometriosis.” NHS, www.nhs.uk/conditions/endometriosis/. Accessed 28 Mar. 2023.
“Endometriosis.” World Health Organization, www.who.int/news-room/fact-sheets/detail/endometriosis. Accessed 28 Mar. 2023.
“Endometriosis: Guideline of European Society of Human Reproduction and Embryology.” European Society of Human Reproduction and Embryology, www.eshre.eu/Guideline/Endometriosis. Accessed 28 Mar. 2023.
“Endometriosis Surgery.” Cleveland Clinic, my.clevelandclinic.org/health/treatments/4620-endometriosis-surgery. Accessed 28 Mar. 2023.
“Endometriosis Treatment & Management.” Medscape, 25 Jan. 2022, emedicine.medscape.com/article/271899-treatment.
Fjerbæk, Agnete, and Ulla B. Knudsen. “Endometriosis, Dysmenorrhea and Diet—What Is the Evidence?” European Journal of Obstetrics, Gynecology, and Reproductive Biology, vol. 132, no. 2, June 2007, pp. 140–47.
“Fulguration.” Cleveland Clinic, my.clevelandclinic.org/health/treatments/22098-fulguration. Accessed 28 Mar. 2023.
“Hormone Treatments.” Endometriosis UK, www.endometriosis-uk.org/hormone-treatments. Accessed 28 Mar. 2023.
“Hormone Treatments for Endometriosis.” Endometriosis UK, www.endometriosis-uk.org/hormone-treatments-endometriosis. Accessed 28 Mar. 2023.
“Hysterectomy - Why It’s Necessary.” NHS, www.nhs.uk/conditions/hysterectomy/why-its-done/. Accessed 28 Mar. 2023.
Kuivasaari, Paula, et al. “Effect of Endometriosis on IVF/ICSI Outcome: Stage III/IV Endometriosis Worsens Cumulative Pregnancy and Live-Born Rates.” Human Reproduction, vol. 20, no. 11, Nov. 2005, pp. 3130–35.
“Pain Relief for Endometriosis.” Endometriosis UK, www.endometriosis-uk.org/pain-relief-endometriosis. Accessed 28 Mar. 2023.
Parasar, Parveen, et al. “Endometriosis: Epidemiology, Diagnosis and Clinical Management.” Current Obstetrics and Gynecology Reports, vol. 6, no. 1, Mar. 2017, pp. 34–41.
“Prostaglandins.” Your Hormones, www.yourhormones.info/hormones/prostaglandins/. Accessed 28 Mar. 2023.
Tanbo, Tom, and Peter Fedorcsak. “Endometriosis-Associated Infertility: Aspects of Pathophysiological Mechanisms and Treatment Options.” Acta Obstetricia et Gynecologica Scandinavica, vol. 96, no. 6, June 2017, pp. 659–67.
Zanelotti, Austin, and Alan H. Decherney. “Surgery and Endometriosis.” Clinical Obstetrics and Gynecology, vol. 60, no. 3, Sep. 2017, pp. 477–84.




