If you’ve ever wondered if endometriosis is the same as PCOS, then read on.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
PCOS vs endometriosis: What are the differences?

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
You might know that polycystic ovary syndrome (PCOS) and endometriosis are conditions that both affect the reproductive system. But aside from that — and the fact that they both have the potential to cause some unpleasant symptoms — there is very little crossover between them.
It can be uncomfortable and sometimes worrying to be faced with some of the symptoms they cause, no matter which condition you have. To help you understand each one properly, we spoke with obstetrician and gynecologist Dr. Allison Rodgers. Here, she helps break down all the similarities and differences in the “PCOS vs. endo” conflict and answers some key questions about both.
PCOS vs. endometriosis: What’s the difference?
Both PCOS and endometriosis affect the reproductive system of people of childbearing age, which usually means women and people who menstruate between the ages of 12 and 50.
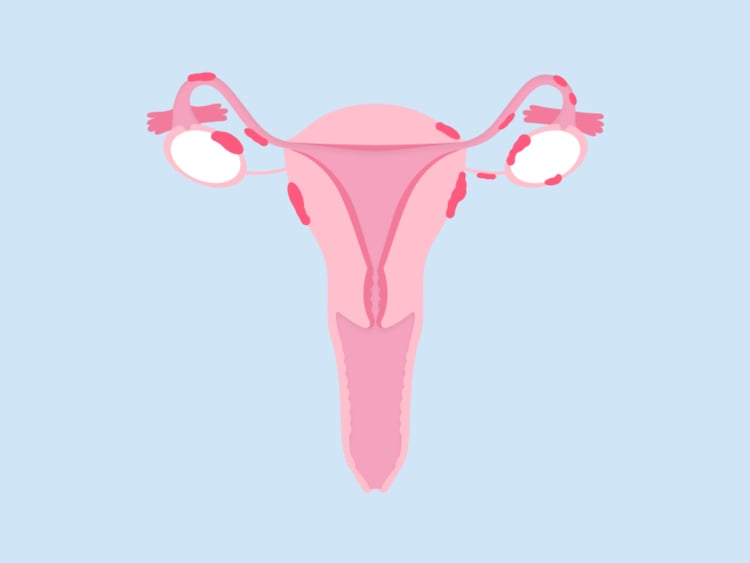
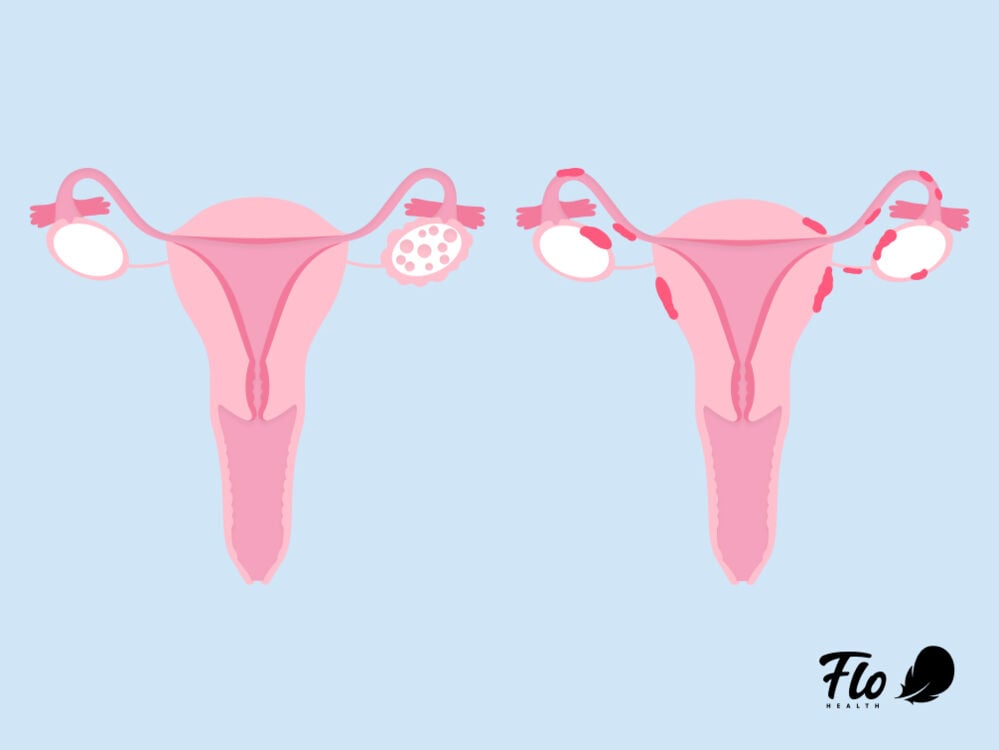
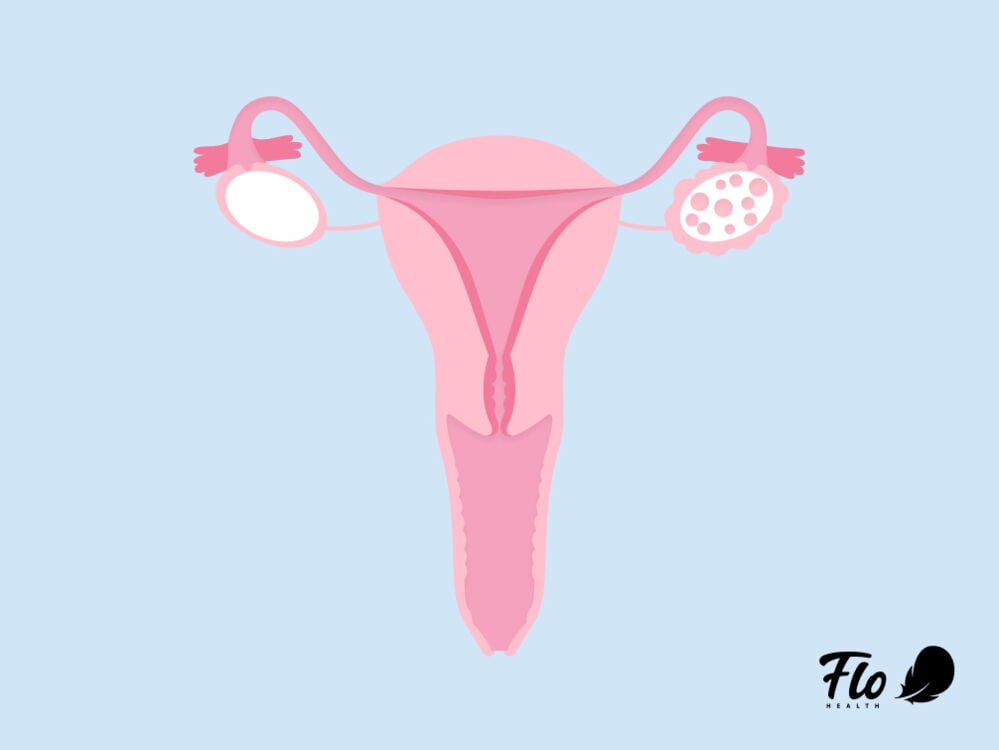
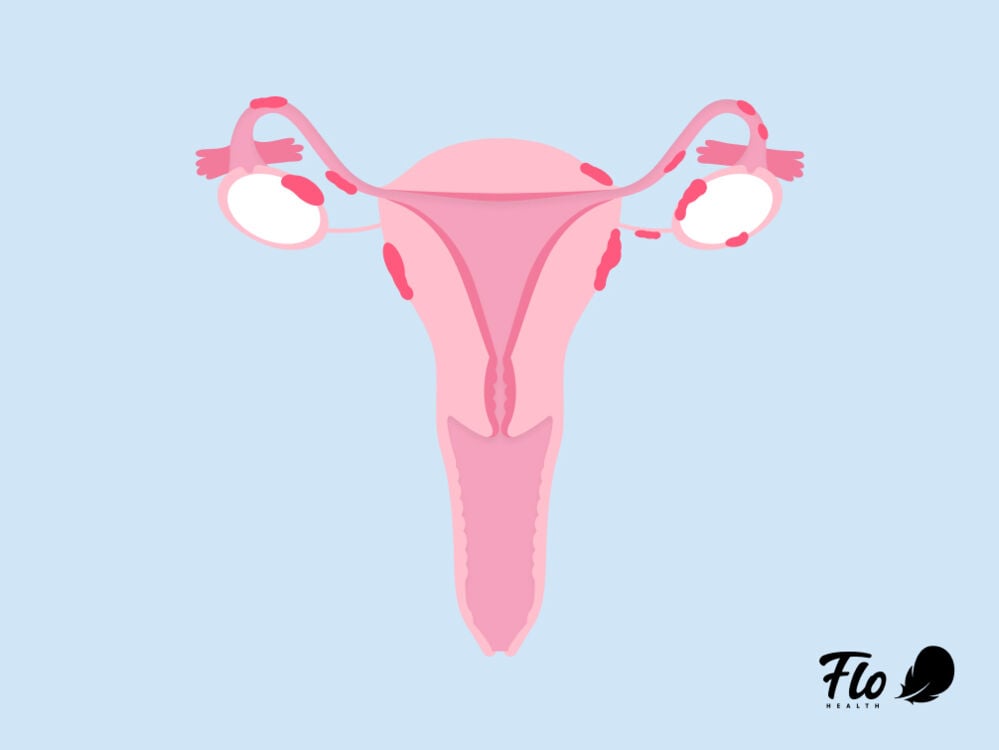
Endometriosis occurs when cells very similar to the ones that make up the lining of your uterus (sometimes called endometrial tissue) are found in patches elsewhere in the body. PCOS is a condition that affects your hormone levels and usually causes an imbalance in your androgen hormones, sometimes called male hormones.
Unfortunately, both are chronic conditions, so although the symptoms might not always surface early on and diagnosis can take a while, they’re usually long-lasting.
Here are some key things you should know about PCOS.
- It’s sometimes — but confusingly, not always — accompanied by small cysts forming in your ovaries, hence the name of the condition. Irregular periods can be the other key symptom of PCOS.
- It’s thought to be caused by a number of things, partly including a genetic predisposition, as some studies have shown that women who have it in their family are more likely to have it themselves. But like lots of female health issues, not much else is known about other causes just yet.
Take a quiz
Find out what you can do with our Health Assistant
Like PCOS, endometriosis also has a hormonal connection. It’s been found to trigger and be triggered by excess production of the female sex hormone estrogen. As we mentioned above, endometriosis is when cells similar to the ones that make up your uterine wall (endometrial tissue) are found in other parts of your body. Common places these cells can be found include the rest of the pelvis, the bowel, the bladder, or the ovaries.
There are various theories about what causes endometriosis — doctors haven’t honed in on a specific one yet — but it’s thought to be because of something called retrograde menstruation. “Certainly, everybody has a little bit of retrograde menstruation, where the blood goes backward through the fallopian [uterine] tubes,” explains Dr. Rodgers. “For people who do not have endometriosis, those glands and blood just get absorbed by the body. It’s no big deal. But for people with endometriosis, those glands are extra sticky, and they can stick to the tubes or the ovary, or they can stick to ligaments and organs in the pelvis.”
As you can see, there’s very little tying the two conditions together beyond an overarching hormonal factor. Some doctors argue that PCOS and endometriosis may actually be at either end of the spectrum when it comes to hormone levels.
“[Two things] they definitely both have in common [are] that neither of these conditions is anyone’s fault, and both are very treatable."
Which is more common: PCOS or endometriosis?
Both conditions are relatively common. PCOS is estimated to affect around 6% to 12% of women of childbearing age, while 10% to 15% of reproductive-aged women have endometriosis.
Can you have both PCOS and endometriosis?
The short answer is, yes. Although this isn’t common, sometimes you can be diagnosed with both PCOS and endometriosis. Studies suggest that approximately 7% of people who have endometriosis also have PCOS. It’s rare because PCOS usually causes you to have fewer periods, so that would mean blood makes its way back up your uterine tubes less frequently, explains Dr. Rodgers. But it can happen, especially during a heavy period.
Other studies suggest that “a significant proportion” of people who have PCOS and have struggled to conceive may also have “unrecognized endometriosis.” However, more research is needed here.
PCOS vs. endometriosis: Symptoms and diagnosis
Now, how do you tell if it’s PCOS or endometriosis? The answer usually lies in the symptoms.
PCOS symptoms
PCOS symptoms usually include at least two out of three of the following:
- Small cysts in the ovaries
- Changes to body hair, such as hair thinning on your head or excessive hair growth on some parts of the body
- A disrupted menstrual cycle or irregular periods — either skipping periods or experiencing very heavy, long periods
“Normally, to have a regular menstrual cycle, the pituitary gland in your brain needs to send a signal down to your ovary to create and release an egg. But for people with PCOS, that’s not happening normally,” says Dr. Rodgers, explaining how PCOS can affect your cycle.
Other symptoms of PCOS include:
- Acne
- Darker, velvety patches of skin around sensitive areas like your neck, groin, or underarms
- Weight gain (particularly in the midsection of your body)
A doctor can tell if you have PCOS based on which of the above symptoms you display, but they can also do a blood test or a pelvic exam to confirm the diagnosis.
Endometriosis symptoms
Endometriosis symptoms are different. They mainly include:
- Chronic pelvic pain and discomfort
- Severe pain during or after sex
- Pain when peeing or pooping
- Abnormally heavy bleeding
Symptoms can be worse (and sometimes debilitating) during your period because the endometrial cells located in other parts of your body can bleed and swell, just like the lining inside of your uterus does during a period.
Although a pelvic exam or MRI scan may give your doctor some idea of whether you might have endometriosis, they can only officially diagnose it through laparoscopic surgery. This involves looking inside your abdomen with a small camera to see if there’s abnormal tissue growth. This often means there are long delays in getting an endometriosis diagnosis, with the average wait being anywhere between 5 and 12 years.
What are the risk factors of endometriosis vs. PCOS?
While anyone can develop PCOS or endometriosis, there are some factors that may mean you’re at a higher risk of experiencing these conditions.
Some of the risk factors that have been linked to endometriosis include:
- If you started your period early (the average age to have your first period is around 12)
- If you have heavy periods that last longer than one week
- If someone in your family has endometriosis
- If you have any other condition that prevents your menstrual blood from leaving your body during your period
You might be more at risk of experiencing PCOS if:
- Someone in your family has PCOS
- You have insulin resistance (when your body can’t process insulin in the way it needs to)
- You have experienced weight gain
It’s important to remember that while these risk factors have been linked to PCOS and endometriosis, if you’re diagnosed with one of these conditions, it isn’t your fault. Your doctor will be able to give you any information or support that you need.
Can PCOS or endometriosis cause problems with fertility?
It’s clear that PCOS and endometriosis symptoms tend to be very different. But there is one way in which they’re similar: Both conditions can make it harder to get pregnant. Here’s why:
- With PCOS, getting pregnant can be trickier because your irregular cycle means you may sometimes skip ovulation (releasing an egg for fertilization), which is vital if you want to conceive.
- In endometriosis, conceiving can be more difficult if patches of endometrial cells have damaged your uterine tubes or your ovaries, which are key reproductive organs. The inflammation you can experience as a result of endometriosis may make it harder to get pregnant.
But if you have either PCOS or endometriosis and hope to have children one day, don’t be disheartened. Many people with these conditions manage to get pregnant and go on to have healthy babies. You can read more about getting pregnant with PCOS here and endometriosis here.
Does endometriosis or PCOS cause complications during pregnancy?
In some cases, either condition may also cause some disruption to your pregnancy. But that certainly isn’t the case with everyone, and sometimes it just means you require a little more care and attention from a doctor who specializes in endometriosis and PCOS.
PCOS and pregnancy
With PCOS, there is an increased risk of gestational diabetes and high blood pressure during pregnancy. This is because it’s a hormonal condition linked to insulin resistance (when your body produces insulin, a hormone designed to regulate blood sugar, but doesn’t use it effectively), so it can cause some bigger-picture changes to your body, explains Dr. Rodgers. Similarly, if you’re currently taking medication, your doctor may talk to you about stopping it or adjusting it during pregnancy. Your doctor should explain your options to you before you make any changes.
PCOS patients are also at an increased risk of preterm labor and birth (where the baby arrives before 37 weeks of pregnancy.) This may sound scary, but it just means that you need to keep an eye on your symptoms during pregnancy.
Endometriosis and pregnancy
Women with endometriosis who are pregnant are 1.5 times more likely to have a preterm birth than women without the condition. That means it’s important to keep an eye on any labor-like symptoms (like contractions or pelvic pain) as you progress through your pregnancy.
Placenta previa is another complication to watch out for if you’re pregnant and have endometriosis. This is when the placenta is located near the opening of the cervix rather than the uterine walls where it should be. Placenta previa can mean there’s a higher risk of blood loss or a ruptured placenta, which is a serious condition requiring immediate medical help. The key symptom is bright-red vaginal bleeding.
None of this is intended to scare anyone. Many people with PCOS and endometriosis go on to have perfectly healthy pregnancies. It just means that if you’re pregnant and have either of these conditions, it’s even more important to talk to a health care professional about your specific needs and how to manage any risks.
PCOS vs. endometriosis: How to manage symptoms
Frustratingly, scientists haven’t gotten to the bottom of how to cure either PCOS or endometriosis just yet. But in more positive news, there are plenty of ways you can manage, mitigate, and treat your symptoms.
Lifestyle changes
Firstly, everyone is different, so talk to your health care provider about what they think your case of PCOS or endometriosis means for you and your body. Usually, a healthy lifestyle can go a long way. For example, in both cases, it can help to make sure you’re eating a balanced diet.
Medication
Depending on your circumstances, doctors might recommend you go on hormonal birth control, which can be helpful for both conditions. How does this work as a treatment for PCOS and endometriosis?
- With PCOS, the hormones from birth control can counteract the hormone imbalance, which can help ease your symptoms.
- With endometriosis, hormones can help to stop or reduce the frequency of your periods, which can prevent more backward blood flow and pain.
There are other medication options for both PCOS and endometriosis that aren’t birth control related, which you can read about in more detail here (PCOS treatment) and here (endometriosis treatment).
Surgery
In the case of endometriosis, if the symptoms cause you extreme discomfort and severe pain, your doctor might suggest surgery to remove or burn away any abnormal tissue growth. There are different levels of surgery available depending on how extensive your endometriosis is, and a consultation with a health care professional will help you to figure out what’s right for you.
Should I have my IUD taken out if I have endometriosis or PCOS?
“I would say it depends on what kind of IUD (intrauterine device) you have,” says Dr. Rodgers. A hormonal IUD can actually be useful for both conditions, just like most hormonal birth control, as it can help manage the pain of endometriosis and help correct the hormonal imbalance of PCOS.
However, a copper IUD may cause more bleeding during your periods and may make things worse if you have endometriosis. If you’re not sure, speak with your physician to see what option works best for you.
PCOS vs. endometriosis: The takeaway
PCOS and endometriosis are poles apart in what they mean for your body, but they do have some things in common. “One thing is that there is a spectrum [for both],” says Dr. Rodgers.
“There’s a huge spectrum between very mild and very severe PCOS and endometriosis. And they are very treatable. There are treatments that work really well for people not trying to get pregnant and people who are trying to get pregnant.”
Both conditions can be tricky to manage, and it’s important to acknowledge that it won’t always be straightforward all of the time so that you’re better equipped to handle the tough times. But there are several tools you can use to help mitigate your symptoms and discomfort. Remember: Every case is different and personal, so speak to your health care provider about how best to navigate it for you.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Anderson-Bagga, Frances M., and Angelica Sze. “Placenta Previa.” StatPearls, StatPearls Publishing, 2021.
Chantalat, Elodie, et al. “Estrogen Receptors and Endometriosis.” International Journal of Molecular Sciences, vol. 21, no. 8, Apr. 2020, doi.org/10.3390/ijms21082815.
“Diagnosing Polycystic Ovary Syndrome in Adults.” NYU Langone Health, nyulangone.org/conditions/polycystic-ovary-syndrome/diagnosis. Accessed 29 June 2022.
Dinsdale, Natalie L., and Bernard J. Crespi. “Endometriosis and Polycystic Ovary Syndrome Are Diametric Disorders.” Evolutionary Applications, vol. 14, no. 7, July 2021, pp. 1693–715.
“Endometriosis.” Office on Women’s Health, www.womenshealth.gov/a-z-topics/endometriosis. Accessed 29 June 2022.
“Endometriosis.” World Health Organization, www.who.int/news-room/fact-sheets/detail/endometriosis. Accessed 29 June 2022.
“Endometriosis Diet: Foods to Eat and Avoid.” Cleveland Clinic, 28 Jan. 2022, health.clevelandclinic.org/endometriosis-diet/.
Hager, Marlene, et al. “The Prevalence of Incidental Endometriosis in Women Undergoing Laparoscopic Ovarian Drilling for Clomiphene-Resistant Polycystic Ovary Syndrome: A Retrospective Cohort Study and Meta-Analysis.” Journal of Clinical Medicine Research, vol. 8, no. 8, Aug. 2019, doi.org/10.3390/jcm8081210.
“Insulin Resistance and Diabetes.” Centers for Disease Control and Prevention, 11 Aug. 2021, www.cdc.gov/diabetes/basics/insulin-resistance.html.
Khan, Muhammad Jaseem, et al. “Genetic Basis of Polycystic Ovary Syndrome (PCOS): Current Perspectives.” The Application of Clinical Genetics, vol. 12, Dec. 2019, pp. 249–60.
Kim, Sun-Gyeong, et al. “Primiparous Singleton Women with Endometriosis Have an Increased Risk of Preterm Birth: Meta-Analyses.” Obstetrics & Gynecology Science, vol. 60, no. 3, May 2017, pp. 283–88.
Matsuzaki, Shinya, et al. “Placenta Previa Complicated with Endometriosis: Contemporary Clinical Management, Molecular Mechanisms, and Future Research Opportunities.” Biomedicines, vol. 9, no. 11, Oct. 2021, doi.org/10.3390/biomedicines9111536.
Moen, Mette H. “Endometriosis, an Everlasting Challenge.” Acta Obstetricia et Gynecologica Scandinavica, vol. 96, no. 6, June 2017, pp. 783–86.
“Polycystic Ovary Syndrome.” Office on Women’s Health, www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome. Accessed 29 June 2022.
Rzońca, Ewa, et al. “Polycystic Ovary Syndrome and Endometriosis as Reasons for Women’s Admission to Outpatient Specialist Care in Poland: A Retrospective Analysis.” International Journal of Environmental Research and Public Health, vol. 18, no. 4, Feb. 2021, doi.org/10.3390/ijerph18041442.
Sawant, Shital, and Priya Bhide. “Fertility Treatment Options for Women with Polycystic Ovary Syndrome.” Clinical Medicine Insights: Reproductive Health, vol. 13, Dec. 2019, p. 1179558119890867.
Schenken, Robert S. “Endometriosis: Pathogenesis, Epidemiology, and Clinical Impact.” UpToDate, 2023.
“Symptoms: Polycystic Ovary Syndrome.” NHS, www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/symptoms/. Accessed 29 June 2022.
Teede, Helena, et al. “International Evidence-Based Guideline for the Assessment and Management of Polycystic Ovary Syndrome 2018.” Monash University, 2018, pp. 6, www.monash.edu/__data/assets/pdf_file/0004/1412644/PCOS_Evidence-Based-Guidelines_20181009.pdf.




