When it comes to PCOS treatment, there are many ways you can manage your PCOS symptoms. Here, an OB-GYN talks us through the options for each symptom — depending on whether you’re trying to have a baby or not.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
PCOS treatment: What are your options?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
You’ve probably heard of polycystic ovary syndrome (PCOS), but what are some of the symptoms, and what is the best treatment for PCOS?
First things first: PCOS is a common hormonal disorder that affects around one in ten reproductive-age women. While scientists still aren’t sure what causes PCOS, what they do know is that you could be more likely to have it if it runs in your family, if you are overweight (that’s a body mass index above 25 kg/m2), or if you have insulin resistance.
There are a number of symptoms associated with PCOS, but the main three are:
- Irregular or missed periods
- A high level of “male” hormones, called androgens (which can cause excessive hair growth on the body and face, as well as acne and thinning of hair on the head)
- Polycystic ovaries, which occur when small fluid-filled sacs, called cysts, develop on the ovaries
Confusingly, despite the name, you don’t always develop polycystic ovaries with PCOS. Instead, a medical professional may diagnose you with PCOS if you exhibit two of the above three symptoms.
Unfortunately, there is currently no cure for PCOS, and if you’ve been diagnosed with the condition, it’s completely understandable to feel upset or concerned about your health. However, please be assured that there are numerous treatment options available (whether you’re trying to conceive or not) that can help to control your symptoms.
Information is power, so to arm you with as many details as possible, we’ve taken a closer look at each PCOS symptom along with the treatments available. We’ve also spoken to Dr. Jennifer Boyle — an OB-GYN (obstetrician and gynecologist) with over 15 years’ experience — to break down everything you need to know about each.
PCOS treatment: Irregular periods
One of the most common symptoms associated with PCOS is irregular periods. The high level of androgens can prevent the ovaries from releasing eggs regularly or stop ovulation altogether. This may mean your periods become heavy, irregular, or you might miss them altogether sometimes.
Dr. Boyle explains that “women with PCOS do not ovulate as often as other women.” That means, typically, they’ll have less than nine periods over the course of a year. If you aren’t trying to conceive, then you may be able to regulate your menstrual cycle with hormonal contraception like the contraceptive pill, vaginal rings, and patches.
Without this hormonal regulation, you may notice you experience heavy bleeding occasionally. “Our ovaries produce both estrogen and progesterone, but they only make progesterone after ovulation. So when you don’t ovulate often, you get estrogen without the balancing effect of progesterone,” Dr. Boyle explains. “Without this balancing effect of progesterone, the lining of the uterus can grow too much.”
If your uterus lining grows too much or becomes too thick, it can cause episodes of abnormal bleeding known as “anovulatory abnormal uterine bleeding.” This bleeding is different from a normal period, notes Dr. Boyle, explaining that “it can be heavier and last much longer, sometimes even weeks.”
This is why hormonal contraceptives are often offered as the first line of treatment for PCOS; they offer the “missing ingredient” of progesterone and may be able to give you that balance.
But what about if you’re trying to conceive? The good news is that there are other ways to manage hormonal imbalances. You can speak to your health care provider about trying letrozole or clomiphene, pills you can take to help trigger ovulation. Alternatively, metformin may be suggested, which is a diabetes medication that can help to regulate your periods. A recent literature review concluded that metformin can effectively bring periods back to a more regular cycle, although scientists are still unsure exactly how it works.
Take a quiz
Find out what you can do with our Health Assistant
PCOS treatment: Excessive hair growth
Another common symptom of PCOS is hair growth. Up to 70% of women with PCOS will experience excessive hair growth, with dark or coarse hair growing on their face, arms, chest, or abdomen. This is called hirsutism and is once again relative to the high level of androgens that result from PCOS.
Excessive hair growth can be inconvenient and upsetting, but there are treatments available. If you’re not currently trying to get pregnant, your health care provider may recommend medication, including birth control pills and the blood pressure medication spironolactone. Again, the key here is to balance out your hormones.
“To treat these symptoms, we must lower testosterone [one of the androgens],” says Dr. Boyle. “Hormonal contraceptives that contain estrogen do this very well, and they’re considered the first-line treatment.”
Spironolactone is an antiandrogen, which means it can block testosterone. It’s usually taken as a pill. “Spironolactone is sometimes used with hormonal contraceptives if they don’t work well enough on their own,” Dr. Boyle explains. However, she adds: “Women who use spironolactone must make sure they are not at risk of becoming pregnant as it can cause birth defects.”
While these treatments can be effective, Dr. Boyle emphasizes that they can take time to work properly. “It will take at least six months to see an effect,” she explains. “Unfortunately, hormonal treatments won’t make the hair go away entirely, but they will allow for hair removal techniques to work much better and will prevent new hair growth.”
If you are trying to conceive, your health care provider may recommend a cream called eflornithine that could help to slow hair growth or electrolysis treatment where the hair follicle is zapped with a weak electric current to stop it from growing back. Laser therapy is another option, which involves a beam of light damaging the hair follicles to prevent hair growth.
PCOS treatment: Hair thinning or loss
Those pesky androgens can also have the opposite effect: causing the hair on your head to thin or fall out, which can be equally distressing. If you experience this, you could try over-the-counter shampoos or supplements or speak to your health care provider. They may suggest trying hormonal contraceptives to lower testosterone levels or other medications designed to stimulate hair growth.
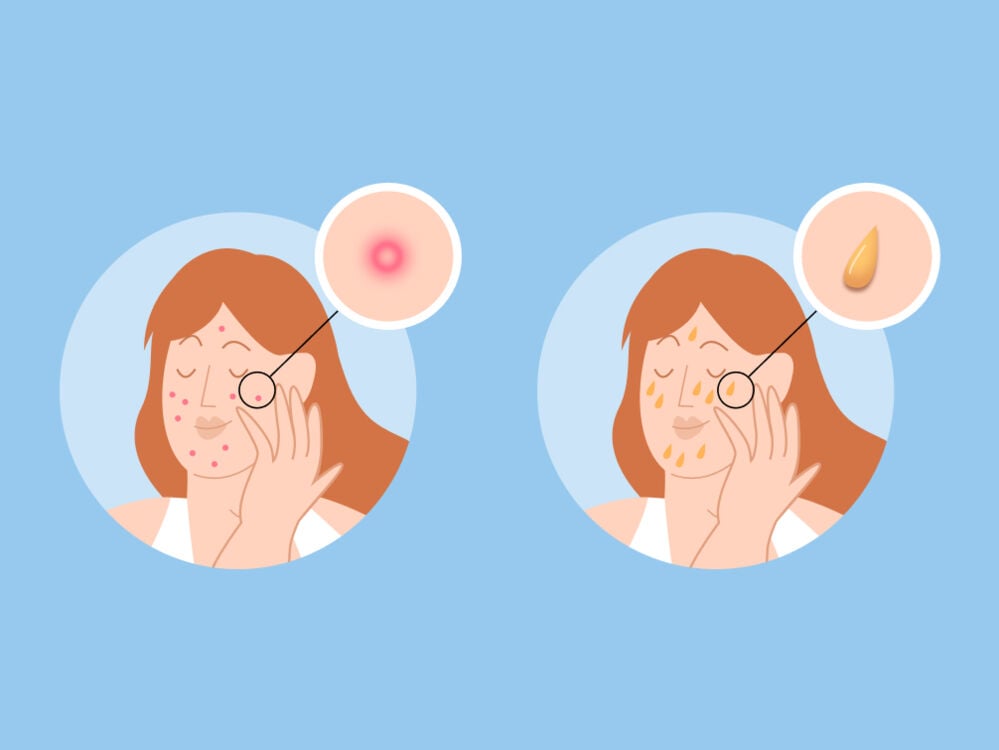
PCOS treatment: Acne or oily skin
PCOS can also make your skin more oily and prone to acne (thanks again, androgens!). The acne will usually appear on your chest, back, or face, and it may be frustratingly stubborn to treat.
If over-the-counter spot creams or treatments don’t work, your health care provider may recommend hormonal contraceptives, and there is also evidence that isotretinoin capsules (commonly known as Roaccutane), an intensive acne treatment, could help too. Speak to your doctor and/or a dermatologist about its pros and cons to find out whether it’s right for you.
PCOS treatment: Weight issues, insulin resistance, and diabetes
You may have heard that insulin resistance, weight gain, and PCOS are linked, but it’s common not to know exactly how or why. The truth is that these three factors can indirectly affect each other, which we’ll explain below.
First up, let’s break down what insulin resistance is. Insulin is a hormone that plays an important role in our bodies because it regulates blood sugar. It does this by helping the blood sugar (which we get from food) to enter our body’s cells, where it’s then used for energy.
Insulin resistance is when your body produces insulin but doesn’t use it effectively. It affects around 65% to 70% of women with PCOS and can be a cause of PCOS as it leads to increased levels of androgens. Often (but not always), insulin resistance can be triggered by being overweight.
Having insulin resistance doesn’t automatically mean you have diabetes, but it can lead you to develop prediabetes or type 2 diabetes, as well as put on weight. Making some lifestyle changes, such as getting more exercise, can help to reverse insulin resistance, lowering your risk of developing diseases such as diabetes or PCOS.
“The first-line treatment for women who are overweight or obese with PCOS is improved nutrition, exercise, and weight loss,” says Dr. Boyle. This can affect other areas of your health.
“People with PCOS have an increased risk of heart disease and other cardiovascular problems and diabetes,” Dr. Boyle explains. “In addition to nutrition and exercise therapy, health care providers may recommend the medication metformin to prevent or treat diabetes.”
PCOS treatment: Polycystic ovaries
You might think that polycystic ovaries are a given if you have PCOS (the clue’s in the name!), but that’s not the case. Some people who are diagnosed with PCOS may have cysts on their ovaries, but others don’t. And the cysts you may experience from PCOS are not the same as functional ovarian cysts.
Functional ovarian cysts are linked to your menstrual cycle. Before ovulation, an egg sits inside a follicle in one of your ovaries. The egg is surrounded by fluid to protect it. If an egg is not released during ovulation or the fluid isn’t discharged once it’s released, then the follicle can swell, creating a cyst. The good news is that functional ovarian cysts normally shrink by themselves within 60 days. However, some larger cysts can cause issues such as pelvic pain and painful periods.
In comparison, the cysts related to PCOS develop due to a lack of ovulation, and as a silver lining, they generally don’t cause any pain.
Surgery can be used to treat functional ovarian cysts, but this is not often needed for polycystic ovaries; if you have been diagnosed with PCOS or think you may have the condition, speak with your health care provider about potential treatment options for cysts.
PCOS treatment: Fertility issues
Since one of the main symptoms of PCOS is irregular periods, it can be tricky to track when you’re ovulating if you’re trying to conceive. This can make timing sex for conception really hard.
As PCOS can prevent ovulation from happening altogether, the condition is, unfortunately, one of the main causes of infertility in women. Between 70% and 80% of women with PCOS are thought to be unable to conceive. This figure might sound alarming, but remember that there are numerous treatment options available. While exact figures are unclear, it’s believed that most women with PCOS will eventually be able to get pregnant if they manage the condition with treatment.
"Most women with PCOS will eventually be able to get pregnant if they manage the condition with treatment"
First of all, your health care provider might recommend a course of oral medication to help stimulate ovulation. They may offer you letrozole or clomiphene, which are taken as a pill in short doses at the beginning of each of your menstrual cycles, usually for a number of cycles. You might also be offered a medication called gonadotropins, which is given through an injection.
If these medications don’t work, your health care provider might suggest trying intrauterine insemination (IUI), also known as artificial insemination, where sperm is inserted into the woman’s uterus in an attempt to trigger fertilization. Following that, in vitro fertilization (IVF) may be suggested, which involves your egg being fertilized in a lab and then transferred into your uterus. In some parts of the world, you may also be offered surgery called ovarian drilling to try and remove the parts of your ovaries that are producing androgens. However, Dr. Boyle adds that “This surgery is not offered in the US for PCOS, mainly because we want to avoid the risks.”
PCOS treatment: Pregnancy complications
Unfortunately, PCOS can also cause a number of pregnancy complications. Sadly, women with PCOS are up to three times more likely to have a miscarriage in early pregnancy. However, plenty of people with PCOS go on to have a healthy pregnancy and birth.
Experiencing a miscarriage can understandably be incredibly distressing, and if you have been affected by this, please don’t hesitate to reach out for support from your friends, family, or the support groups listed below.
- Share Pregnancy and Infant Loss Support (US)
- The Miscarriage Association (UK)
- The Pink Elephants Support Network (AU)
PCOS can also cause other complications, including gestational diabetes, preeclampsia or pregnancy-induced high blood pressure, and in some cases, preterm birth (going into labor before the 37-week mark). However, there is hope on the horizon. Scientists are currently researching whether these risks can be lowered if patients are treated with diabetes medication such as metformin.
PCOS treatment: Depression or anxiety
The physical side effects of PCOS are the ones we tend to know most about, but the condition has also been connected to mental health symptoms. Research suggests that up to 50% of people with PCOS can experience depression or anxiety, but scientists don’t know exactly what causes this link. There was a theory that it could be due to “emotional disturbances” resulting from symptoms of PCOS such as obesity, infertility, and acne, but findings have been mixed, so this shouldn’t be assumed to be the cause.
If this is something you’ve experienced, the good news is there are ways to help manage it. Healthy lifestyle changes are usually recommended as the first port of call for improving mental health in people with PCOS, but cognitive behavioral therapy and medications such as metformin may also be suggested as a means of helping to reduce stress related to the condition.
If you’re struggling with depression or anxiety, it’s always worth speaking with a health care professional who can help you put together a plan of action. Remember that these kinds of mental health issues have been commonly linked with PCOS, so you’re certainly not alone. For additional help and support, reach out to organizations like Mental Health America in the US or Mind in the UK — they will always be happy to help.
PCOS treatment: The takeaway
So, what is the best treatment for PCOS? As we’ve seen, there really is no one-size-fits-all answer to that question. The best course of action across the board is to maintain a healthy lifestyle with regular exercise and healthy, balanced meals. But beyond that, specific treatment for PCOS will first depend on whether or not you are currently trying to have a baby and also on the way the syndrome affects you personally — whether that’s physically or mentally.
While PCOS is a lifelong condition, there are a number of effective treatments available for the symptoms, which means your life before and after PCOS treatment could look radically different. Don’t feel like you just have to “put up” with it; explore your options, but remember to always speak to a medical professional before taking any medication.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Acmaz, G., et al. “The Effects of Oral Isotretinoin in Women with Acne and Polycystic Ovary Syndrome.” BioMed Research International, vol. 2019, Apr. 2019, p. 2513067.
CDC. “Insulin Resistance and Diabetes.” Centers for Disease Control and Prevention, 11 Aug. 2021, https://www.cdc.gov/diabetes/basics/insulin-resistance.html.
CDC. “PCOS (Polycystic Ovary Syndrome) and Diabetes.” Centers for Disease Control and Prevention, 28 Sept. 2021, https://www.cdc.gov/diabetes/basics/pcos.html.
Damone, Anna L., et al. “Depression, Anxiety and Perceived Stress in Women with and without PCOS: A Community-Based Study.” Psychological Medicine, vol. 49, no. 9, July 2019, pp. 1510–20.
“Does PCOS Affect Pregnancy?” www.nichd.nih.gov/, https://www.nichd.nih.gov/health/topics/pcos/more_information/FAQs/pregnancy. Accessed 25 Apr. 2022.
Farrell, Kristen, and Michael H. Antoni. “Insulin Resistance, Obesity, Inflammation, and Depression in Polycystic Ovary Syndrome: Biobehavioral Mechanisms and Interventions.” Fertility and Sterility, vol. 94, no. 5, Oct. 2010, pp. 1565–74.
Grant, Paul, and Shamin Ramasamy. “An Update on Plant Derived Anti-Androgens.” International Journal of Endocrinology and Metabolism, vol. 10, no. 2, Apr. 2012, pp. 497–502.
Hajishafiha, Masomeh, et al. “Combined Letrozole and Clomiphene versus Letrozole and Clomiphene Alone in Infertile Patients with Polycystic Ovary Syndrome.” Drug Design, Development and Therapy, vol. 7, Dec. 2013, pp. 1427–31.
Haoula, Zeina, et al. “Evaluating the Association between Endometrial Cancer and Polycystic Ovary Syndrome.” Human Reproduction , vol. 27, no. 5, May 2012, pp. 1327–31.
Infertility. 3 Mar. 2022, https://www.cdc.gov/reproductivehealth/infertility/index.htm.
Jackson, Joseph, et al. “The Effect of Eflornithine 13.9% Cream on the Bother and Discomfort due to Hirsutism.” International Journal of Dermatology, vol. 46, no. 9, Sept. 2007, pp. 976–81.
Marshall, John C., and Andrea Dunaif. “Should All Women with PCOS Be Treated for Insulin Resistance?” Fertility and Sterility, vol. 97, no. 1, Jan. 2012, pp. 18–22.
Melo, Anderson Sanches, et al. “Treatment of Infertility in Women with Polycystic Ovary Syndrome: Approach to Clinical Practice.” Clinics , vol. 70, no. 11, Nov. 2015, pp. 765–69.
“Metformin.” Nhs.uk, https://www.nhs.uk/medicines/metformin/. Accessed 25 Apr. 2022.
NICE-The National Institute for Health, and Care Excellence. [No Title]. https://bnf.nice.org.uk/drug/spironolactone.html. Accessed 25 Apr. 2022.
“Ovarian Cysts.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/9133-ovarian-cysts. Accessed 25 Apr. 2022.
“Polycystic Ovary Syndrome.” Nhs.uk, https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/. Accessed 25 Apr. 2022.
Polycystic Ovary Syndrome (PCOS). https://www.acog.org/womens-health/faqs/polycystic-ovary-syndrome-pcos. Accessed 25 Apr. 2022.
Rathnayake, Deepani, and Rodney Sinclair. “Innovative Use of Spironolactone as an Antiandrogen in the Treatment of Female Pattern Hair Loss.” Dermatologic Clinics, vol. 28, no. 3, July 2010, pp. 611–18.
Rasquin Leon, Lorena I., et al. “Polycystic Ovarian Disease.” StatPearls, StatPearls Publishing, 2021.
Spritzer, P. M., et al. “Spironolactone as a Single Agent for Long-Term Therapy of Hirsute Patients.” Clinical Endocrinology, vol. 52, no. 5, May 2000, pp. 587–94.
Teede, Helena, et al. “International evidence-based guideline for the assessment and management of polycystic ovary syndrome 2018.” Monash University, Melbourne Australia, 2018, pp. 6. Available at: www.monash.edu/__data/assets/pdf_file/0004/1412644/PCOS_Evidence-Based-Guidelines_20181009.pdf
Tejpal, Chavi, et al. “Is Metformin the Answer for Distressed Females with Menstrual Irregularities?” Cureus, vol. 11, no. 8, Aug. 2019, p. e5460.
Torborg, Liza. “Mayo Clinic Q and A: Effect of PCOS on Fertility Can Vary from One Woman to Another.” Mayo Clinic News Network, 14 July 2015, https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-effect-of-pcos-on-fertility-can-vary-from-one-woman-to-another/.
“Uterine Cancer.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/16409-uterine-cancer. Accessed 25 Apr. 2022.
Witchel, Selma Feldman, et al. “Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment With Emphasis on Adolescent Girls.” Journal of the Endocrine Society, vol. 3, no. 8, Aug. 2019, pp. 1545–73.
Yin, Weiyao, et al. “Association Between Polycystic Ovary Syndrome and Cancer Risk.” JAMA Oncology, vol. 5, no. 1, Jan. 2019, pp. 106–07.




