Surgery may feel like a pretty major way to treat endometriosis. But there are a few different options to match what you want and need. Here, two Flo experts explain how endometriosis surgery can help ease symptoms.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Endometriosis surgery: What are the options, and what actually happens?

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
If you have endometriosis, you may have heard of endometriosis surgery. But what different types of surgery are there, what can each involve, and which is right for you? This guide will give you the lowdown.
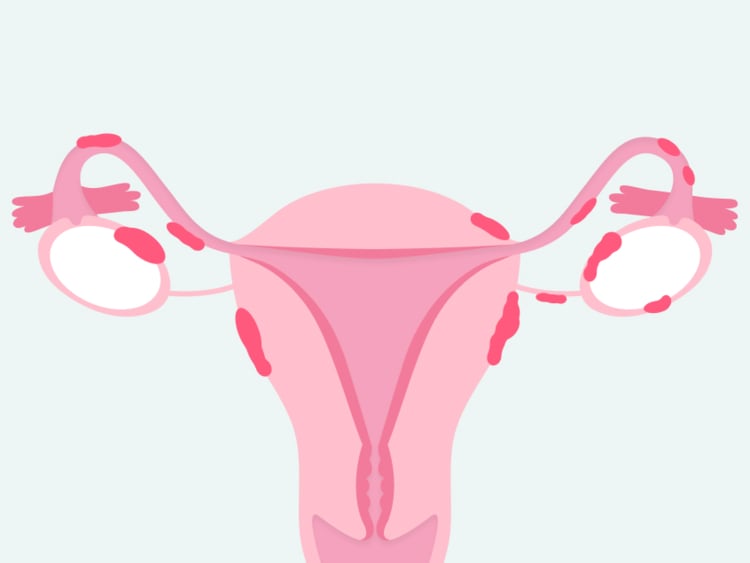
But first, here’s some background: Endometriosis is when cells that are very similar to the ones usually seen in the uterus grow elsewhere in the body. Common places for these cells to grow include the ovaries, outer uterine walls, and uterine (or fallopian) tubes, but they can also extend farther than that. Their presence can cause severe pain and discomfort because they may bleed and swell, just as the lining inside of your uterus does during a period.
Surgery is just one option for managing the symptoms associated with endometriosis, and here, a Flo expert outlines everything you need to know.
How is endometriosis diagnosed?
As you may already be aware, it can take on average anywhere between eight and 12 years to get an endometriosis diagnosis. This is because symptoms are often dismissed as painful menstrual cramps — something that many people assume it’s “normal” to have to deal with.
Health care providers and patients normalizing complaints and symptoms aren’t the only drivers behind the delay in endometriosis diagnosis. Detecting endometriosis through MRI or ultrasound images requires a doctor with a certain level of expertise, and there is a shortage of people trained in this area, explains Dr. Samir Babayev, assistant professor of obstetrics and gynecology at the Mayo Clinic School of Health Sciences, Minnesota, US. Even if your doctor specializes in endometriosis, it can be really difficult to spot endometriosis using imaging studies.
“This means that often, surgery is the gold standard for diagnosing endometriosis,” says Dr. Babayev. Surgery is the most invasive treatment option for endometriosis, so your doctor will want to ensure you understand what will happen. This can mean that there may be a bit of a delay in treatment.
Take a quiz
Find out what you can do with our Health Assistant
What are the benefits of endometriosis surgery?
The good news is that along with diagnosing the disease, surgery is also used to manage endometriosis. In a nutshell, it involves removing endometriosis tissue, and it has a number of benefits, including:
- Improving symptoms and significantly reducing pain
- Improving fertility, meaning it may be a great fit for you if you’re trying to get pregnant or thinking of starting a family one day
“With endometriosis, you often have high levels of inflammation that scar tissue has built up,” says clinical assistant professor of obstetrics and gynecology Dr. Warren Jay Huber III, Louisiana, US. “The surgery can restore the normal relationships between the ovaries, the fallopian [uterine] tubes, and the uterus, which is especially important for patients who are looking to try to conceive.”
Endometriosis surgery types
There are a few different endometriosis surgery options, and your doctor should be happy to discuss the different factors you might want to consider before making a decision.
“If fertility is an important priority for the patient, then we’d go with the more conservative option,” says Dr. Babayev. “If they are not interested in future fertility and would like to minimize chances of needing another surgery, then we’d go with a more radical approach.”
After you discuss the different options with your doctor, Dr. Babayev advises getting a second opinion. “Medicine is at least 50% art, and it’s important to consider options and hear multiple opinions,” he says.
Here’s what you need to know about the different types of endometriosis surgery.
Laparoscopy
If you have endometriosis and want to become pregnant in the future, your doctor may discuss surgical options that are described as “fertility-sparing.” These are treatments that don’t impact your reproductive organs so you can try to get pregnant in the future.
You may have heard of laparoscopic or “keyhole” surgery before. It’s sometimes described as a “conservative” procedure or minimally invasive surgery and is fertility-sparing. It’s when a surgeon will make little cuts in your lower abdomen and insert a laparoscope (a small tube with a light and camera) into the incisions to look inside the area.
Laparoscopic surgery is a tool doctors use to diagnose endometriosis. At the same time, they might also remove any of the endometriosis lesions they find by burning them off (known as fulguration or ablation) or cutting them out (excision). This type of surgery is a good option if you’re planning to start a family because the goal is to preserve your reproductive organs.
Laparotomy
If some endometriosis tissue is left behind after a laparoscopy, then it’s possible that it may grow back. In that case, your doctor might consider slightly more complex surgery. One of these surgery options is called a laparotomy. This is where a larger incision is made in your lower abdomen to remove endometriosis lesions wherever they are visible, which could mean removing endometrial tissue from organs like the bladder, urinary tract, or bowel. This surgery is still intended to protect your reproductive organs so is another fertility-sparing option.
Your doctor may recommend a laparotomy if you’ve had a couple of laparoscopy procedures but still have endometriosis tissue remaining. Due to the fact that it’s more invasive, you may need to have more doctors present during the operation. As Dr. Babayev explains, “There are a number of patients who require treatment for deep endometriosis, and this usually requires a multidisciplinary team of surgeons” who are specialists.
Hysterectomy
If you have severe endometriosis (stage 4) or don’t want to get pregnant in the future, then your doctor may discuss the option of having a hysterectomy. Hysterectomy is seen as a way to treat endometriosis because by removing the source organs of endometriosis, you’re removing the underlying cause of the disease and therefore reducing your chances of needing surgery again. This procedure is when your uterus is removed. If you have endometriosis lesions on your uterine tubes and ovaries, then there are other surgery options to remove those too.
If your ovaries are removed during a hysterectomy, you may be offered hormone replacement therapy afterward. This is because your ovaries are responsible for making estrogen, and by removing them, you will experience a dramatic dip in your hormone levels. This can lead to vaginal dryness, hot flashes, and mood changes, all of which hormone replacement therapy may help you manage.

What does endometriosis surgery feel like?
Many people who start to explore surgery as a way to treat endometriosis will initially look into having a laparoscopy. Lowri was one of them. After 17 years of symptoms, including severe pain that radiated from her waist to her knees, she finally got her endometriosis diagnosis just before her 31st birthday.
“You go in doubting yourself,” Lowri, who is now 36, says. She pushed her doctor to schedule a laparoscopy for her after reading an article about endometriosis. “I had this feeling that I’d wake up and they’d say, ‘There’s nothing in there,’” she says. “So actually, when I woke up and the doctor said I had quite extensive endometriosis over one side of my pelvis — and they’d burned it all off — I was really happy.”
“Technically, that day I was clear of all visible endometriosis.”
Lowri had two keyhole surgeries before finding out that she may need more complex surgery that would still protect her reproductive organs. “I was in surgery for 6.5 hours, and it went amazingly well,” Lowri says. “Technically, that day I was clear of all visible endometriosis.”
Rosie also has endometriosis and had four conservative surgeries over a period of 10 years before deciding to have a hysterectomy in 2020. “It’s natural to have a few moments and think, ‘This is huge. This is irreversible.’ But the surgery was the right thing to do,” says Rosie. “I’d known for some time that it was my best chance of being pain free in the longer term. Yes, there is pain after surgery. But it’s short term. It’s going to go away.”
After a slow recovery, which took around seven weeks, Rosie started to feel the best she’d felt in a long time. “I still get occasional bits of pain, but it’s not a fraction of what it was before. I’ve also got mobility in my lower back that I can’t remember having for years. Because I was quite happy that children weren’t going to happen for me — I’d dealt with that for quite some time before the surgery — I didn’t think about it too much afterward. I’m still a woman. Just because those bits aren’t in my body, I am still me.”
How long does recovery take after surgery?
Recovering from any kind of surgery can take its toll both emotionally and physically. You might be curious as to how long you will stay in the hospital and when you’ll be back on your feet. The answer is that it really depends on the type of surgery you had. In fact, the earlier a patient gets moving after surgery, the better it could be for their recovery.
Recovery times can vary from person to person depending on the type of surgery you have:
- Laparoscopy: within five days
- Laparotomy: You may be sore for a couple of weeks. If there are no complications, you may return to normal activities within that time period.
- Hysterectomy: It can take from six to eight weeks to recover from a hysterectomy, and you may not be discharged from the hospital for a few days following your surgery. However, your recovery time is really personal to you and depends on the type of surgery you had.
The key thing to remember is that everybody is different, and the most important thing to do following your procedure is to be gentle with yourself and give yourself all the time you need. Your doctor will be able to advise you on anything you can do during your recovery and answer any questions you have.
How quickly can endometriosis grow back after surgery?
After conservative surgery, if endometriosis grows back, it usually does so within five years, explains Dr. Babayev. He says that endometriosis-related pelvic pain also comes back in about a third of these patients.
But even with the most radical surgeries, it’s vital for you to know that endometriosis surgery is not a cure. “Although the more radical the surgery, the more likely the patient won’t need further surgery, patients might need treatments and interventions later on,” Dr. Babayev adds.
This is because even if you have your uterus and ovaries removed, there might still be microscopic amounts of the disease present (although the chance of recurrence in this instance is very low, at less than 5%). Plus, there’s always a risk that surgery will cause scarring, which can lead to other problems.
“I never dared hope that the surgery would help to the extent it has”
Rosie was aware of all this but still decided that endometriosis surgery was worth it. “I thought, even if I still have some problems, but there is a bit less pain, that’d still be better,” she says. “I never dared hope it would be this much better, that the surgery would have helped to the extent it has.”
Endometriosis surgery: The takeaway
Having any kind of procedure like this can be a scary decision to make, so it’s natural to spend a considerable amount of time deciding whether it’s worth getting endometriosis surgery. The only person that can answer that is you, but thankfully, there are endometriosis support groups and organizations all over the world that can offer you advice. These include Endometriosis Association, which is available globally, Endometriosis Foundation of America, and Endometriosis UK. Your doctor will also be able to answer all of your questions. Whether surgery is right for you is a hugely personal decision, but know that there are options out there besides simply putting up with your pain.
If you believe you might have endometriosis but haven’t yet received a diagnosis, try tracking your symptoms with an app like Flo. Keeping a log of your symptoms can be helpful when you speak to your doctor. That’s the first step to easing and managing your symptoms because you shouldn’t have to just live with them.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Classification of Endometriosis. The American Fertility Society.” Fertility and Sterility, vol. 32, no. 6, Dec. 1979, pp. 633–34, www.ncbi.nlm.nih.gov/pubmed/510564.
“Endometriosis.” World Health Organization, 31 Mar. 2021, www.who.int/news-room/fact-sheets/detail/endometriosis.
“Endometriosis.” Office on Women’s Health, 22, Feb. 2021, www.womenshealth.gov/a-z-topics/endometriosis.
“Treatment: Endometriosis.” NHS, www.nhs.uk/conditions/endometriosis/treatment/. Accessed 17 Mar. 2022.
“Laparoscopy (Keyhole Surgery).” NHS, www.nhs.uk/conditions/laparoscopy/. Accessed 21 Feb. 2022.
Lebovic, Dan I. “Endometriosis: Surgical Management of Pelvic Pain.” UpToDate, 2021, www.uptodate.com/contents/endometriosis-surgical-management-of-pelvic-pain?topicRef=7383&source=see_link.
“Management of Endometriosis.” The American College of Obstetricians and Gynecologists, July 2010, www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2010/07/management-of-endometriosis.
Moen, Mette H. “Endometriosis, an Everlasting Challenge.” Acta Obstetricia et Gynecologica Scandinavica, vol. 96, no. 6, June 2017, pp. 783–86, doi.org/10.1111/aogs.13148.
Namnoum, A. B., et al. “Incidence of Symptom Recurrence after Hysterectomy for Endometriosis.” Fertility and Sterility, vol. 64, no. 5, Nov. 1995, pp. 898–902, doi.org/10.1016/s0015-0282(16)57899-6.
“Surgical Treatment of Endometriosis: Excision and Destruction.” Brigham and Women’s Hospital, www.brighamandwomens.org/obgyn/infertility-reproductive-surgery/endometriosis/surgical-treatment-of-endometriosis-excision-and-destruction. Accessed 11 Mar. 2022.




