Thanks to fluctuating hormone levels, your joints can swell and ache during perimenopause. Here’s how to relieve the pain and keep moving.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Perimenopause joint pain: Why it happens and how to soothe it


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Was that a slight twinge in your knee when you got out of bed this morning? Or maybe you felt a little achy relaxing on the couch post-dinner? That sounds like joint pain — aka aches or soreness in your joints.
Joint pain — medically known as arthralgia — is a common complaint, and a bunch of factors could be causing it. It could be a sports injury or perhaps a health condition, and we know aches and pains can happen more often as you get older.
However, if you’re in your late 30s or 40s, your cycle tracking app (such as Flo) shows your periods have been hit and miss lately, and you’ve been feeling a bit creaky, it might be a sign of perimenopause joint pain. If it turns out your aches and pains are hormone-related, don’t lose hope. With the right treatment, most perimenopause symptoms are manageable. You don’t just have to live with it.
Here, family physician Dr. Sarina Schrager, Wisconsin, US, shares everything you need to know about perimenopause joint pain. If you want to know why it happens, when to see a doctor, and how to ease your achy joints, read on.
Key takeaways
- Over 50% of women report some form of joint pain or stiffness during perimenopause.
- Hormone therapy (previously known as hormone replacement therapy or HRT) has been found to help perimenopause joint pain symptoms in many people.
- Low estrogen levels are believed to be a contributor to perimenopause joint pain.
- Simple lifestyle changes, including keeping active and improving your muscle strength, may help to ease joint pain and stiffness.
Take a quiz
Find out what you can do with our Health Assistant
Is joint pain linked to perimenopause?
Have you heard of menopause but not perimenopause? The terms are often used interchangeably, but they’re two separate things. Put simply, perimenopause refers to the years leading up to menopause (your final period).
Perimenopause is a natural life stage that almost everyone with ovaries goes through. It usually begins somewhere between your late 30s and 50s but happens most often in your 40s. You’re later diagnosed as having gone through menopause when you haven’t had a period for 12 months (usually between the ages of 45 and 55). From then on, you are postmenopausal.
So, how can joint pain be linked to perimenopause? Just like other, more widely known perimenopause symptoms such as hot flashes and brain fog, it’s all thanks to fluctuating hormones. During perimenopause, your estrogen levels start to change and eventually reduce. Estrogen is obviously important in your menstrual cycle, but it also plays a role in protecting your joints. The exact science isn’t well understood, says Dr. Schrager, but she points out some possible reasons why:
- Your joints contain estrogen receptors, so hormone changes can affect them.
- Estrogen can help to reduce inflammation (when your immune system reacts to injury with pain, redness, or swelling), which might explain the achiness you’ve noticed.
- “Your muscle mass decreases [during perimenopause], so you have less support for your joints,” explains Dr. Schrager.
Joint pain affects over half of people going through perimenopause, so if it’s bothering you, and you think your changing hormones might be to blame, speak to your doctor for advice. Only they will be able to confirm whether it’s perimenopause causing your aches and pains.
As a general rule, hormone-related discomfort tends to be sneaky and subtle, says Dr. Schrager. “It would be more gradual than pain from an injury,” she says. “It wouldn’t be like you woke up yesterday and your knee hurt. It would develop over weeks and months.”

What else causes joint pain?
You might be experiencing joint pain for reasons other than perimenopause, such as arthritis, a sports injury, or even an infection. This article focuses on perimenopause joint pain, but if you experience any type of pain that prevents you from living your everyday life, it’s always a good idea to reach out to your health care provider. Other causes of joint pain can include:
- Sprains and strains: When you hurt yourself, usually in sports, the injured area tends to be swollen or bruised.
- Inflammatory arthritis: A group of conditions, including gout and rheumatoid arthritis, where your immune system is overactive and causes joint inflammation.
- Fibromyalgia: A chronic condition that brings on muscle and joint pain, often in the neck and shoulders.
- Tendonitis and tendinopathy: Pain and swelling in your tendons, usually after an injury or overuse.
- Bursitis: When a bursa, a fluid-filled sac that sits between bones and tendons (like bubble wrap for your body), gets inflamed.
- Infection: Infections like septic arthritis can make your joints swell and become hot.
If you’re not sure what’s causing your pain, book an appointment with your health care provider.
They’ll be able to provide advice, put together a personalized treatment plan, and direct you to the right specialist, should you need one. If it is perimenopause related, they could help you to manage any other symptoms you might be experiencing, too.
How to ease joint pain caused by perimenopause
If you’re in constant pain, don’t feel like you have to live with it. It’s best to chat with your doctor, but you could also give these perimenopause joint pain relief tips a try.
1. Consider hormone therapy
If your pain is perimenopause related, your doctor might recommend hormone therapy (also known as hormone replacement therapy or HRT) in some cases. Research suggests it could help. In a study of over 10,000 postmenopausal women, those who took an estrogen tablet (a form of hormone therapy) daily for at least a year experienced less joint pain than the ones who took a placebo.
As with many things, there are pros and cons of hormone therapy. Chat with your doctor about it, and they can help you decide whether it’s a good option for you.
2. Build up strength and mobility
Your first instinct might be to put your feet up in an attempt to soothe your soreness. However, the best way to keep joints healthy and flexible is often to keep moving.
You want to aim to support your joints by improving your muscle strength. If weight-bearing exercises aren’t comfortable for you, or your doctor has told you to avoid them, lower-impact activities like cycling or swimming are great too.
Exercise can also help to keep your bones healthy, make it easier to sleep, and improve your balance — all of which is good news for your joints. It could also help you maintain a healthy weight for you, allowing you to take stress off your joints and make them feel better.
“For the most part, moderate exercise (walking, biking, swimming) is protective and may make joint pain better, but some strenuous exercise (running) can make it worse,” says Dr. Schrager. “If joint pain gets worse after activity, resting for a few days should make it better.”
3. Prioritize sleep
If perimenopause joint pain is bugging you, another thing you can do is try to improve your sleep. Banish your phone from the bedroom and ditch that evening espresso. Caffeine affects you longer than you might think; it can take up to 10 hours to completely clear from your bloodstream.
How does all this link to joint soreness? “We depend on sleep for muscle recovery, and we know that women, as they start to have hormone fluctuations, tend not to sleep as well,” says Dr. Schrager.
4. Take over-the-counter pain relief
To ease perimenopause joint pain, you could try simple painkillers such as acetaminophen (paracetamol) or ibuprofen, suggests Dr. Schrager. Topical pain relief (a gel or patch applied to the affected area) could also be helpful.
5. Apply a hot or cold compress
You could try a cold compress to soothe perimenopause joint pain by reducing inflammation. You can make one at home super easily by following these simple steps:
- Dampen a cloth with cold water.
- Fold it and place it in a ziplock bag.
- Pop the bag in the freezer for 15 minutes.
- Apply it to the affected area.
Alternatively, you could try a heating pad, a hot shower, or a sauna. “Unless there is an acute injury, heat is often the better option,” says Dr. Schrager. “Heat tends to loosen up muscles and can help pain.”
When to see a doctor about joint pain
If you experience any type of pain, don’t shrug it off — make an appointment with your doctor. Not quite convinced? “If the pain is interfering with what you want to do with your day, if you can’t sleep, and if you’ve tried a few things, and you’re not getting better, [reach out for help],” says Dr. Schrager.
You should also visit your doctor if:
- Your pain gets worse or keeps coming back.
- It hasn’t improved after being treated at home for two weeks.
- Your joints are stiff for more than 30 minutes after you wake up.
- You’re losing weight unexpectedly.
- It’s harder than normal to walk due to the pain.
Seek urgent medical attention if:
- The skin around your sore joint is swollen or red and feels hot.
- Alongside your joint pain, you feel unwell, hot, and shivery or have a fever.
- You’ve had a fall or injury, and your joint pain is really bad.
- You can’t walk or put weight on your sore joints.
- You have a tingling sensation or no feeling at all in the area around your joint.
- The joint has moved out of place (it might look a bit odd, or you might have heard a pop or crack).
Your health care provider will first try to figure out the cause of your pain and then recommend the best way to treat it. You might need to have some tests, like scans or a blood test, but these should help your doctor recommend specific treatments based on the likely cause of your pain.
More FAQs
Can perimenopause cause hip and back pain?
During perimenopause, your estrogen levels start to change, making you more susceptible to aches and pains. This can affect various parts of the body, including the hips and back.
Does menopause joint pain go away?
It can be normal for our bodies to become more achy as we age, whether we’re in the perimenopausal or the postmenopausal stage. But everyone is different.
Some of us may notice short-term discomfort, others may feel ongoing joint pain, and some people may not experience any at all. Exploring different treatment options can be the best way to help joint pain go away if that’s something you’re experiencing.
What supplements help menopause joint pain?
There is little evidence to suggest that dietary supplements have any effect on perimenopause or menopause joint pain symptoms. It’s also worth noting that menopause supplements are not routinely regulated by the US Food and Drug Administration.
If you’re keen to give supplements a try, discuss it with your health care advisor, as some products can cause side effects or interact with other medications.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Anderson, A. Shane, and Richard F. Loeser. “Why Is Osteoarthritis an Age-Related Disease?” Best Practice and Research: Clinical Rheumatology, vol. 24, no. 1, Feb. 2010, pp. 15–26, https://doi.org/10.1016/j.berh.2009.08.006.
Bartlett, Susan. “Role of Exercise in Arthritis Management.” Johns Hopkins Arthritis Center, www.hopkinsarthritis.org/patient-corner/disease-management/role-of-exercise-in-arthritis-management/. Accessed 2 Apr. 2024.
Bhargava, Juhi, and John A. Hurley. “Fibromyalgia.” StatPearls, StatPearls Publishing, 11 June 2023, www.ncbi.nlm.nih.gov/books/NBK540974/.
Charnoff, Jesse, et al. “Tendinosis.” StatPearls, StatPearls Publishing, 17 Oct. 2022, www.ncbi.nlm.nih.gov/books/NBK448174/.
Chlebowski, Rowan T., et al. “Estrogen Alone and Joint Symptoms in the Women’s Health Initiative Randomized Trial.” Menopause, vol. 20, no. 6, June 2013, pp. 600–08, doi:10.1097/GME.0b013e31828392c4.
“Dealing with Common Aches and Pains as We Age with Dr. Donald Ford.” Cleveland Clinic, 21 Nov. 2018, my.clevelandclinic.org/podcasts/health-essentials/dealing-with-common-aches-and-pains-as-we-age-with-dr-donald-ford.
“Exercise Helps Ease Arthritis Pain and Stiffness.” Mayo Clinic, 21 Sep. 2023, www.mayoclinic.org/diseases-conditions/arthritis/in-depth/arthritis/art-20047971.
“Here’s Why Losing Weight Is the Key to Losing Joint Pain.” Cleveland Clinic, Dec. 2020, health.clevelandclinic.org/if-you-lose-weight-you-can-lose-joint-pain-too/.
“Hormone Therapy for Menopause.” The American College of Obstetricians and Gynecologists, Oct. 2021, www.acog.org/womens-health/faqs/hormone-therapy-for-menopause.
“How to Quit Caffeine without a Headache.” Cleveland Clinic, Nov. 2023, health.clevelandclinic.org/how-to-quit-caffeine/.
“Joint Pain.” Cleveland Clinic, my.clevelandclinic.org/health/symptoms/17752-joint-pain. Accessed 2 Apr. 2024.
“Joint Pain.” NHS, www.nhs.uk/conditions/joint-pain/. Accessed 2 Apr. 2024.
Kozinoga, Mateusz, et al. “Low Back Pain in Women before and after Menopause.” Menopause Review, vol. 14, no. 3, Sep. 2015, pp. 203–07, https://doi.org/10.5114/pm.2015.54347.
Magliano, Malgorzata. “Menopausal Arthralgia: Fact or Fiction.” Maturitas, vol. 67, no. 1, 10 May 2010, pp. 29–33, https://doi.org/10.1016/j.maturitas.2010.04.009.
Malanga, Gerard A., et al. “Mechanisms and Efficacy of Heat and Cold Therapies for Musculoskeletal Injury.” Postgraduate Medicine, vol. 127, no. 1, Jan. 2015, pp. 57–65, https://doi.org/10.1080/00325481.2015.992719.
Martín-Millán, Marta, and Santos Castañeda. “Estrogens, Osteoarthritis and Inflammation.” Joint, Bone, Spine, vol. 80, no. 4, July 2013, pp. 368–73, https://doi.org/10.1016/j.jbspin.2012.11.008.
“Menopause 101: A Primer for the Perimenopausal.” The North American Menopause Society, www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal. Accessed 2 Apr. 2024.
“Menopause.” World Health Organization, 17 Oct. 2022, www.who.int/news-room/fact-sheets/detail/menopause.
“Perimenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21608-perimenopause. Accessed 2 Apr. 2024.
Poudel, Pooja, et al. “Inflammatory Arthritis.” StatPearls, StatPearls Publishing, 17 Apr. 2023, www.ncbi.nlm.nih.gov/books/NBK507704/.
Roman-Blas, Jorge A., et al. “Osteoarthritis Associated with Estrogen Deficiency.” Arthritis Research and Therapy, vol. 11, no. 241, 21 Sep. 2009, doi:10.1186/ar2791.
“Septic Arthritis.” NHS, www.nhs.uk/conditions/septic-arthritis/. Accessed 2 Apr. 2024.
“Sprains and Strains.” NHS, www.nhs.uk/conditions/sprains-and-strains/. Accessed 2 Apr. 2024.
“Supplements for Menopause Symptoms: Are They Safe?” Cleveland Clinic, Oct. 2022, health.clevelandclinic.org/menopause-supplements.
“What Is Menopause?” National Institute on Aging, www.nia.nih.gov/health/menopause/what-menopause. Accessed 2 Apr. 2024.
History of updates
Current version (04 April 2024)
Published (04 April 2024)
In this article
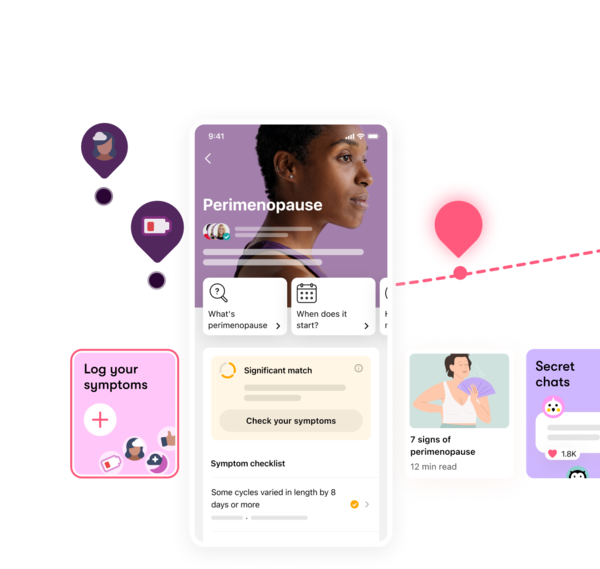
Track your perimenopause journey in the Flo app
-
Log symptoms and get tips to manage them
-
Learn what to expect with expert-led articles and videos
-
Connect with others who can relate to how you're feeling




