You can get pregnant right away, but it's not always that straightforward. We asked a Flo expert to give us the lowdown.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Getting pregnant after birth control: How long does it take?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
If you’ve been taking birth control for a while and are now thinking about having a baby, then it’s only natural to wonder how long it might take to conceive once you stop.
The key thing to know if you're pregnancy planning is that having taken birth control doesn’t impact your ability to conceive — however, the type of contraceptive you have been taking could affect how long it takes.
Flo spoke with Dr. Jennifer Boyle, obstetrician and gynecologist at Massachusetts General Hospital, US, to break down any common misconceptions about stopping birth control and find out how to prepare for pregnancy after using contraception.
Key takeaways
- “In general, taking hormonal birth control will not make it take longer to become pregnant,” Dr. Boyle says. “However, becoming pregnant can take time.”
- Most people will find their periods return to normal a cycle or two after stopping hormonal birth control, so there’s no delay in getting pregnant.
- Barrier methods of birth control, like condoms, work by physically blocking sperm, so they have no impact on your cycle.
- Other factors, such as age and health, can affect your ability to get pregnant.
How long does it take to get pregnant after birth control?
It’s impossible to give a definitive answer since, as Dr. Boyle says, “It’s different for everyone!” Much research has been done to help understand how long it takes to get pregnant once you stop taking birth control.
For example, a 2018 review of 22 studies from 1985 to 2017 found that out of almost 15,000 women who stopped taking contraception, 83.1% got pregnant within the first 12 months.
Dr. Boyle explains why: “Most people will have a menstrual period about 30 days after stopping hormonal birth control,” she says. “We usually tell people that if they haven’t returned to their typical menstrual cycle two to three months after stopping their birth control method, then they should see a doctor or other clinician.”
And remember that getting pregnant isn’t always as easy as your sex education classes made it seem. Over to Dr. Boyle again: “In general, taking hormonal birth control will not make it take longer to become pregnant. However, becoming pregnant can take time. It’s very normal for it to take six to 12 months to become pregnant even if everything is normal and healthy with a couple.”
Understanding your cycle can make all the difference in knowing what’s normal for your body. Flo’s ovulation calculator and period tracking can help you understand when you’re most fertile and may help you know when the right time to try to conceive is.
It’s worth knowing the latest fertility testing advice by age, too, because our ability to get pregnant does decline as we get older.
If you’re under 35, then you should book an appointment with your doctor if you haven’t become pregnant after 12 months of regular unprotected sex. If you’re 35 or older, then schedule a checkup if six months have passed. If you’re 40 or older, schedule that appointment right away.
Your health care provider might suggest running some tests to check if everything is OK with you and your partner. Trying to conceive can be an emotional time, so speak to your doctor if you have any concerns or questions. They’re there to support you.
Does the type of contraceptive you’re taking matter?
The type of contraception you have been using could affect how long it takes to get pregnant once you stop because some will affect your menstrual cycle, while others will not. Here’s a breakdown of what to expect:
Barrier methods such as condoms, etc.
Condoms, diaphragms, the cervical cap, and the contraceptive sponge are all known as barrier methods of contraception. This is because — when used correctly — they physically prevent the sperm from reaching an egg, so fertilization can’t happen. They’re also nonhormonal, so they don’t affect your cycle. “Because there is no effect on ovulation, there would not be any delay in achieving pregnancy,” Dr. Boyle says.
Combination hormonal methods
Combination hormonal methods means birth control with both the female sex hormones, estrogen and progestin (the synthetic form of progesterone). They include the combined oral contraceptive pill, also known as COCs or OCPs.
These types of birth control work by mimicking the hormones that control your cycle. But, according to Dr. Boyle, “There would be no delay” if you wanted to stop using them and start trying for a baby.
“Most people will have a menstrual period one month after stopping combined hormonal methods,” says Dr. Boyle.
However, if you’re also taking the pill to help with cycle conditions or symptoms, then she has the following advice. “Some people use combined hormonal methods because they have menstrual or hormonal problems such as irregular periods or polycystic ovary syndrome (PCOS),” Dr. Boyle explains. “It’s important to remember that although you may have regular “periods” while using birth control, these are not true menstrual cycles, as discussed above. So, if you had irregular periods or other problems before taking OCPs, then these problems might return when you stop taking OCPs, and that can make it more difficult to become pregnant.
“That’s why we want people to seek care if they don’t have regular menses [periods] within two to three months after stopping birth control.”
Take a quiz
Find out what you can do with our Health Assistant
Progestin-only hormonal methods
If you take the mini pill (progestin-only pills or POPs) or have had the contraceptive injection or implant fitted, then you’re using a progestin-only type of birth control.
These work by releasing progesterone into your bloodstream to thicken the cervical mucus so it’s harder for sperm to get to the egg.[17] POPs can also prevent ovulation (although four in 10 women will still ovulate) and thin the lining of your uterus.
But, as Dr. Boyle explains, getting pregnant after stopping progestin-only birth control shouldn’t be an issue in itself. “[They have] the same rapid return to fertility as the combination methods,” Dr. Boyle explains.
“In fact, it may be even faster with POPs such as Norethindrone 0.35 mg, as not everyone has their ovulation suppressed with this method. Fertility should return to baseline, and cycles should return to normal within two to three months after stopping the implant as well.”
There is one caveat, though: the depot medroxyprogesterone acetate shot (commonly known as Depo Provera). “It’s good to know that the one method that can have a delayed return to fertility after stopping it is the Depo Provera injection,” Dr. Boyle says. “Return of normal menses [periods] can take up to six to 12 months after stopping Depo Provera.”
Intrauterine devices
“The copper IUD has a very rapid return to fertility after stopping. For example, if you had your copper IUD taken out in the first part of your menstrual cycle, you could become pregnant that very cycle. This is because it does not suppress ovulation.
“Progestin-releasing IUDs have a return to fertility that is similar to hormonal methods. Cycles should be back to normal within 2 to 3 months, and if not, a person should seek care.”
What are the chances of getting pregnant after stopping birth control?
To put it simply, you should prepare for the chance that you could get pregnant quite quickly after stopping contraception. “Your chance of becoming pregnant after stopping birth control is the same as if you hadn’t taken birth control,” explains Dr. Boyle. “We generally say that there is a 24% chance of becoming pregnant each menstrual cycle.”
However, it’s important to remember that everyone is different — and if conception is taking longer than expected, it’s likely not due to your birth control. “There are lots of factors that can affect someone’s chances of becoming pregnant, but having recently used birth control (unless it was Depo Provera) is not one of them,” Dr. Boyle adds.
“Factors that can make it harder to become pregnant include older age, body weight, smoking, marijuana use, and heavy alcohol use.”
Certain medical conditions, such as pituitary gland disorders, PCOS, and thyroid disorders, among others, may also affect your fertility. Remember, too, that your partner’s health and their sperm count and quality play a major part in getting pregnant. In fact, male infertility is the cause of a third of infertility cases worldwide, with around 9% of US males having fertility issues. That’s why doctors often recommend you both undergo fertility tests if you’re struggling to conceive.
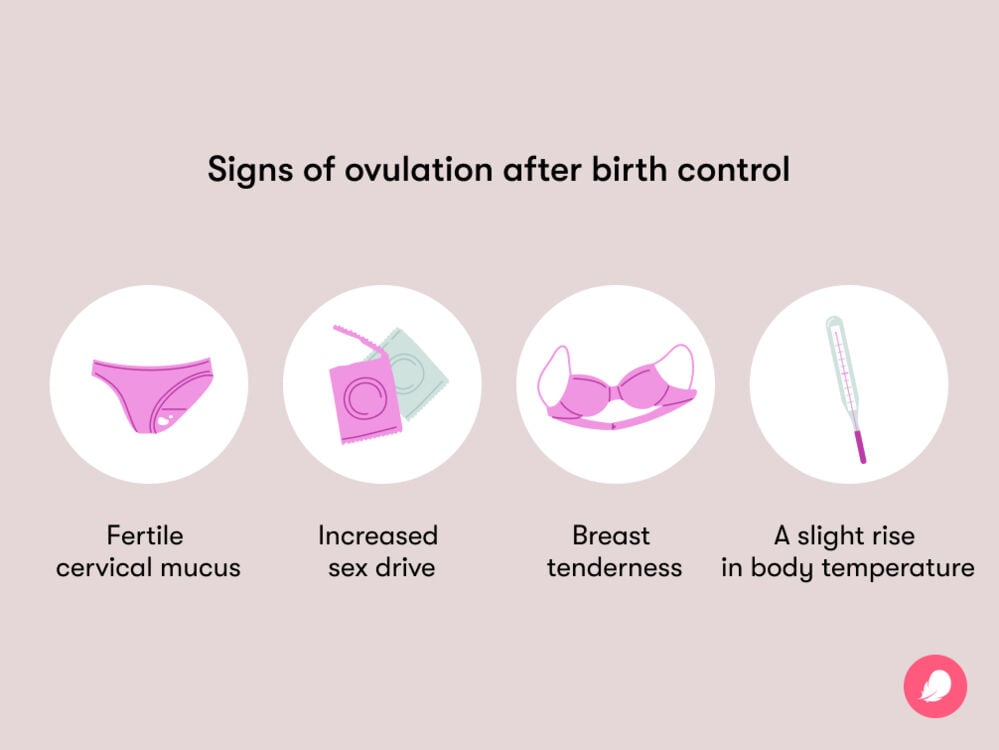
How to spot the signs of ovulation after birth control
Ovulation is when the ovaries release an egg to be fertilized by a sperm. This happens around the midpoint in your cycle (if your cycle is 28 days) — and the days around ovulation are when you’re at your most fertile. So, it makes sense to know the signs of ovulation to look for if you’re trying.
There are a few key signs to look out for that can indicate ovulation:
- Fertile cervical mucus (i.e., slippery, with a consistency and color similar to egg whites)
- Increased sex drive
- Breast tenderness
- A slight rise in body temperature (typically about 0.5 to 1 degree, so often only noticeable if you’re tracking your basal body temperature to determine when you’re ovulating)
- Tracking your cycle using an app like Flo can help you figure out your most fertile days. Remember, though, that you should never use this tool as birth control.
When to stop taking birth control
Unless there is a health or personal reason, “You should not stop birth control until you are really ready to become pregnant,” says Dr. Boyle. “It’s good to take extra folic acid before becoming pregnant because this can decrease the chance of birth defects in the baby’s spine and brain. So start taking a folic acid supplement or a prenatal vitamin about one to three months before you want to try for pregnancy. Then, when you stop your birth control, you will be ready to go!”
Irregular cycles or health conditions can make trying to conceive a little more complicated. Dr. Boyle has this advice: “If you have a history of irregular cycles before, you could consider stopping birth control earlier to make sure your cycles are normal and regular. The downsides of this are that you would need to then use condoms, and you could become pregnant sooner than you planned.”
As always, it’s best to talk to your doctor before you stop birth control. They’ll be able to offer personalized advice or refer you to a fertility specialist if necessary.
More FAQs
Will it be hard to get pregnant after birth control?
That depends, explains Dr. Boyle. “But unless you have been using the Depo Provera injection, it won’t be hard because of the birth control.” Speak to your doctor if you’re struggling to get pregnant.
Does birth control affect fertility later in life?
This is a common misunderstanding, explains Dr. Boyle. “This has been studied extensively, and using birth control will not make it harder to become pregnant later in life. Now, if a person uses birth control until they are age 45 and then tries to become pregnant, they are likely to have a hard time, but it will be because of their age and not because of birth control.
Is being on birth control for 10 years bad?
“No!” says Dr. Boyle. “Longer use of combined oral contraceptive pills has actually been associated with a lower risk of ovarian cancer, so there are actually benefits to longer use.” Women who use nonhormonal IUDs or birth control pills have a lower risk of developing endometrial cancer, too.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Anovulation.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21698-anovulation. Accessed 22 Feb. 2024.
“Birth Control Options.” Cleveland Clinic, my.clevelandclinic.org/health/articles/11427-birth-control-options. Accessed 21 Feb. 2024.
Cooper, Danielle B., et al. “Oral Contraceptive Pills.” StatPearls, StatPearls Publishing, 24 Nov. 2022. www.ncbi.nlm.nih.gov/books/NBK430882/.
“Depo-Provera® (Birth Control Shot).” Cleveland Clinic, my.clevelandclinic.org/health/drugs/4086-depo-provera-birth-control-shot. Accessed 21 Feb. 2024.
Edelman, Alison, et al. “Continuous or Extended Cycle vs. Cyclic Use of Combined Hormonal Contraceptives for Contraception.” Cochrane Database of Systematic Reviews, vol. 2014, no. 7, 29 July 2014, doi:10.1002/14651858.CD004695.pub3.
“Evaluating Infertility.” The American College of Obstetricians and Gynecologists, Jan. 2020, www.acog.org/womens-health/faqs/evaluating-infertility.
“Folic Acid.” Centers for Disease Control and Prevention, www.cdc.gov/ncbddd/folicacid/about.html. Accessed 22 Feb. 2024.
Girum, Tadele, and Abebaw Wasie. “Return of Fertility after Discontinuation of Contraception: A Systematic Review and Meta-Analysis.” Contraception and Reproductive Medicine, vol. 3, no. 9, July 2018, doi:10.1186/s40834-018-0064-y.
“Having a Baby after Age 35: How Aging Affects Fertility and Pregnancy.” The American College of Obstetricians and Gynecologists, Feb. 2023, www.acog.org/womens-health/faqs/having-a-baby-after-age-35-how-aging-affects-fertility-and-pregnancy\.
“How Common Is Infertility?” Eunice Kennedy Shriver National Institute of Child Health and Human Development, www.nichd.nih.gov/health/topics/infertility/conditioninfo/common. Accessed 21 Feb. 2024.
“Infertility.” Mayo Clinic, 13 Sep. 2023, www.mayoclinic.org/diseases-conditions/infertility/symptoms-causes/syc-20354317.
Kaunitz, Andrew M. “Birth Control: Beyond the Basics.” UpToDate, 11 Dec. 2023, www.uptodate.com/contents/hormonal-methods-of-birth-control-beyond-the-basics/print.
MacMahon, B. “Risk Factors for Endometrial Cancer.” Gynecologic Oncology, vol. 2, no. 2–3, Aug. 1974, pp. 122–29, https://doi.org/10.1016/0090-8258(74)90003-1.
“Minipill (Progesterone-Only Birth Control Pill).” Cleveland Clinic, my.clevelandclinic.org/health/drugs/17707-minipill. Accessed 21 Feb. 2024.
“Progestin-Only Hormonal Birth Control: Pill and Injection.” The American College of Obstetricians and Gynecologists, Jan. 2023, www.acog.org/womens-health/faqs/progestin-only-hormonal-birth-control-pill-and-injection.
“The Menstrual Cycle: Menstruation, Ovulation, and How Pregnancy Occurs.” The American College of Obstetricians and Gynecologists, Jan. 2022, www.acog.org/womens-health/infographics/the-menstrual-cycle.
Thibault, C., and M. C. Levasseur. “Ovulation.” Human Reproduction, vol. 3, no. 4, 1 May 1988, pp. 513–23, https://doi.org/10.1093/oxfordjournals.humrep.a136737.




