Does nursing stop you from getting pregnant? You might have heard this and wonder if it’s true. Here’s the lowdown on breastfeeding and birth control from a Flo expert.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Birth control while breastfeeding: Do you need it, and is it safe?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
When you’ve just had a baby, the prospect of getting pregnant again (or even having sex, for that matter) may be the last thing on your mind. But because there are so many common myths surrounding breastfeeding and fertility, it’s important to be aware of the facts.
You may have noticed that your period hasn’t returned yet if you’re nursing — but does that mean you don’t need to use contraception? We’ll explain the science so you can relax and choose the best birth control plan for you.
Key takeaways
- Despite what you might have heard, you do need to use birth control while breastfeeding. While nursing can delay ovulation (when your ovary releases an egg around mid-cycle) for some women, it’s not the most reliable way to prevent pregnancy.
- If you are breastfeeding exclusively, it can delay ovulation and your period for up to around six months after giving birth.
- Birth control that contains the hormone estrogen can lower your breast milk supply, so it’s best to choose a progestin-only type (like the mini pill, hormonal IUD, or implant) or a barrier method (like condoms) instead.
Do you need birth control while breastfeeding?
In short, yes, you do need to use birth control while breastfeeding for the most reliable protection against pregnancy. “It is still possible to get pregnant while breastfeeding,” says Dr. Renita White, obstetrician and gynecologist, Georgia Obstetrics and Gynecology, Georgia, US. So, it’s important to take steps to prevent pregnancy if you don’t plan on having another baby just yet.
“However, those who are exclusively nursing and nursing every three hours consistently are less likely to conceive,” White adds. “[So] this could be a source of contraception in the first six months postpartum.”
Here’s why: If you don’t breastfeed, you can ovulate (release an egg) within a few weeks of giving birth. However, breastfeeding can delay ovulation after childbirth, usually for up to around six months. This is because while you’re nursing, your body produces a hormone called prolactin. It’s this hormone that makes you produce milk. However, prolactin also pauses ovulation, and releasing an egg is essential in order to get pregnant or have a period. So, by delaying ovulation, breastfeeding can temporarily lower your fertility. Usually, ovulation and your periods return by around six months postpartum.
Using breastfeeding as a contraceptive during those first six months is known as the lactational amenorrhea method (LAM). The method will only work if you haven’t had a period yet since delivering your baby and if you breastfeed exclusively and frequently, which means:
- No more than four hours between feeds during the day
- No more than six hours between feeds at night
Also, note that pumping breast milk might make the method less effective. Understandably, this breastfeeding schedule is not practical for everyone. Remember, while there are benefits to breastfeeding, there is no shame in using formula milk as much as you need to.
It’s also important to know that ovulation generally happens around two weeks before you get your period, which means you could get pregnant before you know your period is about to restart. Ovulation tests are also less reliable postpartum. This is because prolactin decreases levels of luteinizing hormone — the hormone that ovulation tests measure to figure out if you’re ovulating. So, as there is no way of knowing for sure when your fertility will return, using birth control while breastfeeding will give you more reliable protection against pregnancy.
Take a quiz
Find out what you can do with our Health Assistant
What birth control is safe while breastfeeding?
This is an important question, as some forms of birth control are more suitable than others while you’re breastfeeding. “While it is safe to take birth control while breastfeeding, hormonal methods that include estrogen (like the combined pill, patch, and ring) may decrease milk supply,” says Dr. White. This is because estrogen decreases levels of prolactin — which, as we’ve seen, is the essential hormone for milk production.
Hormonal birth control either contains a combination of estrogen and progestin (a synthetic version of progesterone) or progestin on its own. The combined pill, patch, and ring all contain both hormones, but the following methods only contain progestin, which likely won’t impact your breast milk supply. These options are all safe to use while breastfeeding and can be started as soon as immediately after birth.
Progestin-only pill (POP)
The POP (or mini pill) is your estrogen-free alternative to the combined pill. Just like combined oral contraceptives, you need to take it every day. But take note — while it’s good to take any type of oral contraceptive at the same time each day, you need to take POPs within the same three-hour time frame. If you miss the three-hour window, you’ll need to use backup protection for two days. This can be a big adjustment, especially if you’re used to having 12 hours to remember to take a missed pill with the combined oral contraceptive. Setting birth control reminders in the Flo app can help you stick to your schedule.
The POP is just as effective as combined birth control pills, with a 0.3% failure rate with perfect use (when always taken correctly) and a 7% failure rate with typical use (if you forget to take a pill or don’t always take it at the same time). That means, on average, with perfect use, fewer than one in every 100 women will become pregnant per year.
Two types of POPs are available in the United States: one that involves taking the hormone continuously throughout the month and another that includes a four-day break every 24 days. In both types, breakthrough bleeding or spotting is a common side effect. Your doctor will be able to help you figure out which pill might be the best for you.
Hormonal intrauterine devices (IUDs)
A hormonal IUD is a small, T-shaped device that sits in your uterus and releases a type of progestin called levonorgestrel. Hormonal IUDs are one of the most effective methods of birth control, with a failure rate of only 0.2% with typical use. They’re also low maintenance, which can be a real bonus when you’re busy breastfeeding and caring for your baby.
Once your health care provider has inserted the device into your uterus, it can be left there for three to eight years, depending on the brand. If you decide to have another baby, your health care provider can remove the IUD at any point. An IUD won’t impact your fertility — after it’s been removed, you could get pregnant right away. Breakthrough bleeding or spotting is common during the first few months of using hormonal IUDs, but this side effect usually improves over time.
Implant
The implant is a small rod that gets inserted under the skin in your upper arm and releases progestin. Like a hormonal IUD, it can be a convenient form of birth control as it can be left in for up to three years. Plus, if you decide you want another baby, you can have it removed at any point and could get pregnant straight away. It’s also one of the most effective forms of contraception, with a typical use failure rate of just 0.1%. The main downsides are that the implant has to be inserted and removed by your health care provider and can cause breakthrough bleeding or spotting.
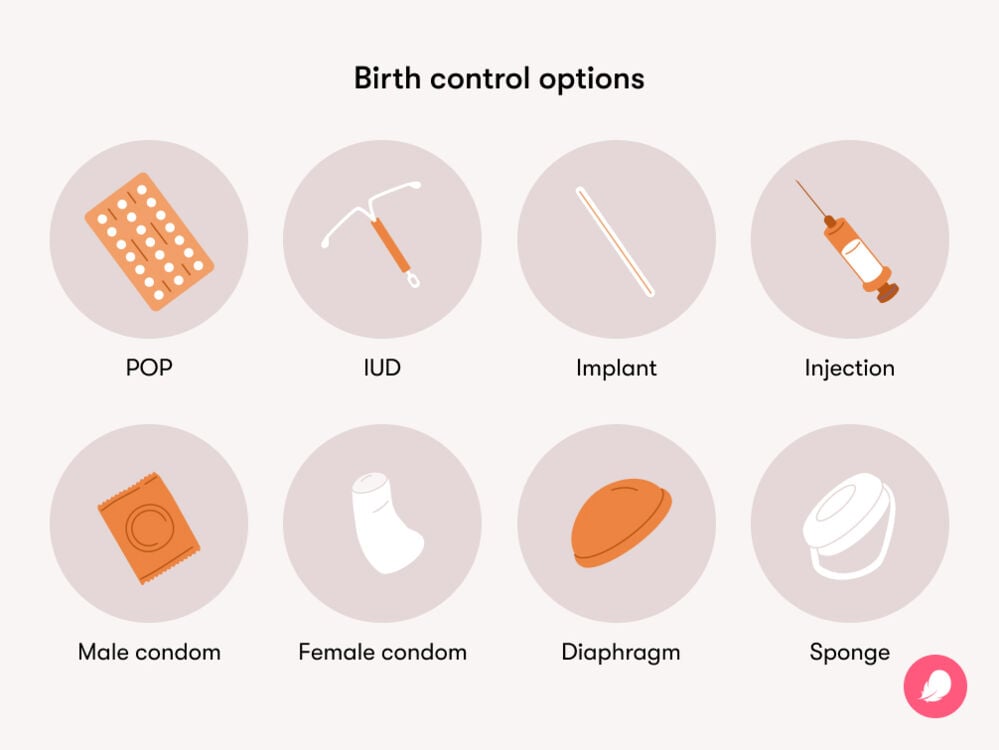
Injection
The injection or birth control shot injects progestin directly into your bloodstream via a muscle, often in your butt or arm. You need to get repeat shots from your health care provider every three months, so you’ll want to set up those calendar alerts.
Along with breakthrough bleeding or spotting, the injection can cause weight gain in some people. It can also take longer for your fertility to return after stopping the injection compared to other types of birth control. Most people find their period returns within six months of their last injection, but it can take longer. So, if you’re planning to try for another baby in the not-too-distant future, this may not be the best option.
Barrier methods
Progestin-only hormonal birth control isn’t your only option. Barrier methods of birth control don’t contain any hormones, if that’s your preference, and there are various different types to choose from. None of the following nonhormonal birth control methods will affect your milk if you’re breastfeeding.
Male condoms
A male condom (often just called a condom) is a thin covering that’s worn on the penis to stop sperm from entering the vagina. With perfect use, they have a failure rate of 2%; however, with typical use, this rises to 13%. Unlike other forms of birth control, condoms also protect against STIs.
Female condoms
Female condoms are designed to be put inside the vagina before sex to stop sperm from entering the uterus. Putting one in is a bit like inserting a tampon, as you put one end (where there is a thick inner ring) inside the vagina and keep the other (a thinner outer ring) outside of it.
Female condoms are slightly less effective than regular condoms, with a 5% failure rate with perfect use and a 21% failure rate with typical use. While you can start using these right after childbirth, you may not want to insert them — or even have sex, for that matter — if you’ve had a vaginal birth and the area feels very sensitive. Whichever birth control you decide on, make sure you’re kind to yourself and don’t rush anything you might not feel physically ready for.
Spermicide
Spermicide is a chemical that destroys sperm. It can be used alone or alongside another form of birth control. It comes in various forms that all need to be inserted into the vagina before sex, including foams, creams, gels, suppositories, and films. You need to wait for 15 minutes after inserting the spermicide before having sex, and it will only work for up to an hour, so you’ll need to be organized with this one. With perfect use, spermicide has a failure rate of 18% and, with typical use, 21%. Spermicide can be used right after childbirth if you’re feeling up to it.
A newer alternative to spermicide is a vaginal gel, which you need to insert into your vagina one hour before you have sex. It works by lowering the pH of the vagina, making it harder for sperm to move. One study found the gel was 86.3% effective.
Sponge
The sponge is a small, round piece of plastic foam that’s coated with spermicide and placed into the vagina before you have sex. It works by trapping and absorbing sperm, preventing it from entering your cervix and reaching an egg. With perfect use, it has a failure rate of 20%, and with typical use, it is 27% for women who have had a baby. The sponge can become less effective once you’ve had a baby because childbirth changes the size of the cervix. You can start using it six weeks after childbirth when your uterus and cervix will most likely have returned to their normal size.
Diaphragm
The diaphragm is a small, dome-shaped device that covers the cervix. You must use it in combination with spermicide and need to keep it in for at least six hours (and up to 24) after having sex, making it one of the slightly more admin-heavy contraceptives. With perfect use, the diaphragm has a failure rate of 6%, and with typical use, 17%. Like the sponge, you need to wait until six weeks after childbirth to use it.
Can you take emergency contraception while breastfeeding?
“Yes, it is safe to take emergency contraception while breastfeeding,” says Dr. White. You can safely breastfeed your baby around three to four hours after taking the medication.
Choosing birth control while breastfeeding
As we’ve seen, you have plenty of options when it comes to birth control while breastfeeding. If the amount of choice feels overwhelming, just go with what feels right for you. Ultimately, it’s a personal decision, and what’s best for you may not be for the next person. “The method you use should be based on preference,” says Dr. White. “One type of method is not better than another.” Ultimately, the most effective method is the one you’ll use.
The best thing to do is to speak to your health care provider about your needs and how you’re feeling about birth control. They’ll be able to recommend a method that suits you and your partner.
More FAQs
What’s the best form of birth control while breastfeeding?
“The best form of birth control while nursing is the method that you prefer,” says Dr. White. “Yet, it’s important to know that methods that include estrogen (like the pill, patch, and ring) may decrease milk supply.”
What are the chances of getting pregnant while breastfeeding?
If you’re breastfeeding exclusively according to the LAM method criteria, your chances of getting pregnant within the first six months after childbirth are about 0.9% with perfect use of the method and 2% with typical use.
How long does it take for fertility to return after breastfeeding?
Breastfeeding can impact fertility, but how quickly your menstrual cycle returns after childbirth will vary from person to person according to many factors. If you’re breastfeeding, ovulation usually returns up to around six months postpartum, but if you have any questions about your menstrual cycle after giving birth, then be sure to speak to your doctor.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Appendix D: Contraceptive Effectiveness.” Centers for Disease Control and Prevention, 25 Apr. 2014, www.cdc.gov/mmwr/preview/mmwrhtml/rr6304a5.htm.
“Barrier Methods of Birth Control: Spermicide, Condom, Sponge, Diaphragm, and Cervical Cap.” The American College of Obstetricians and Gynecologists, Apr. 2022, www.acog.org/womens-health/faqs/barrier-methods-of-birth-control-spermicide-condom-sponge-diaphragm-and-cervical-cap.
“Birth Control Sponge.” Cleveland Clinic, my.clevelandclinic.org/health/articles/24324-birth-control-sponge. Accessed 16 Apr. 2024.
“Breastfeeding? Yes, You Can Still Get Pregnant.” Cleveland Clinic, Sep. 2023, health.clevelandclinic.org/can-you-get-pregnant-while-breastfeeding.
“Combination Birth Control Pills.” Mayo Clinic, 13 Jan. 2023, www.mayoclinic.org/tests-procedures/combination-birth-control-pills/about/pac-20385282.
“Contraception.” Centers for Disease Control and Prevention, www.cdc.gov/reproductivehealth/contraception/index.htm. Accessed 16 Apr. 2024.
“Depo-Provera (Contraceptive Injection).” Mayo Clinic, 22 Feb. 2022, www.mayoclinic.org/tests-procedures/depo-provera/about/pac-20392204.
“Female Condom.” Cleveland Clinic, my.clevelandclinic.org/health/drugs/17946-female-condom. Accessed 16 Apr. 2024.
“How Soon Can You Get Pregnant after Stopping Birth Control?” University of Utah Health, 5 Aug. 2021, healthcare.utah.edu/the-scope/health-library/all/2021/08/how-soon-can-you-get-pregnant-after-stopping-birth-control.
“Intrauterine Device (IUD).” Cleveland Clinic, my.clevelandclinic.org/health/treatments/24441-intrauterine-device-iud. Accessed 16 Apr. 2024.
Kaunitz, Andrew M. “Patient Education: Hormonal Methods of Birth Control (Beyond the Basics).” UpToDate, 18 Mar. 2024, www.uptodate.com/contents/hormonal-methods-of-birth-control-beyond-the-basics/print.
Kaunitz, Andrew M. “Patient Education: Long-Acting Methods of Birth Control (Beyond the Basics).” UpToDate, 28 Nov. 2022, www.uptodate.com/contents/long-acting-methods-of-birth-control-beyond-the-basics.
Labbok, Miriam H. “Breastfeeding, Fertility, and Family Planning.” The Global Library of Women’s Medicine, Nov. 2008, www.glowm.com/section-view/heading/Breastfeeding,%20Fertility,%20and%20Family%20Planning/item/396.
“Menstrual Cycle.” Cleveland Clinic, my.clevelandclinic.org/health/articles/10132-menstrual-cycle. Accessed 16 Apr. 2024.
“Minipill (Progesterone-Only Birth Control Pill).” Cleveland Clinic, my.clevelandclinic.org/health/drugs/17707-minipill. Accessed 16 Apr. 2024.
“Ovulation Home Test.” MedlinePlus, medlineplus.gov/ency/article/007062.htm. Accessed 16 Apr. 2024.
“Postpartum Birth Control.” The American College of Obstetricians and Gynecologists, Apr. 2023, www.acog.org/womens-health/faqs/postpartum-birth-control.
“Prolactin.” Cleveland Clinic, my.clevelandclinic.org/health/articles/22429-prolactin. Accessed 16 Apr. 2024.
Shenenberger, Donald. “Hyperprolactinemia Clinical Presentation.” Medscape, 9 Feb. 2022, emedicine.medscape.com/article/121784-clinical.
Stewart, Judith. “Phexxi.” 28 Mar. 2023, Drugs.com, www.drugs.com/phexxi.html.
“The Right Way to Use a Female (Internal) Condom.” Centers for Disease Control and Prevention, www.cdc.gov/condomeffectiveness/internal-condom-use.html. Accessed 16 Apr. 2024.
Thomas, Michael A., et al. “A Novel Vaginal pH Regulator: Results from the Phase 3 AMPOWER Contraception Clinical Trial.” Contraception: X, vol. 2, 1 July 2020, doi:10.1016/j.conx.2020.100031.
Trussell, James. “Understanding Contraceptive Failure.” Best Practice and Research. Clinical Obstetrics & Gynaecology, vol. 23, no. 2, Apr. 2009, pp. 199–209, doi:10.1016/j.bpobgyn.2008.11.008.
World Health Organization. “Mechanisms of Action and Effectiveness of Contraception Methods.” Family Planning: A Global Handbook for Providers, 2022 Edition. 14 Nov. 2022, cdn.who.int/media/docs/default-source/reproductive-health/contraception-family-planning/mechanisms-of-action-and-effectiveness-of-contraception-methods.pdf?sfvrsn=e39a69c2_1.




