Planning a pregnancy can be exciting and involves a lot of preparation. One important thing to keep in mind is fertility levels, and whether you’re showing any signs of infertility. In other words, you’ve tried getting pregnant (through regular, unprotected sex) for over a year and have been unable to do so. But what are the symptoms of female infertility, and how do we treat them?
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Female Infertility: How to Spot the Signs and What to Do Next


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Signs of infertility
If you’re having trouble getting pregnant, you’re not alone. Around 12 to 13 percent of couples in the U.S. experience infertility issues. That number jumps to 17 percent worldwide. While it may be difficult to detect infertility symptoms outright, here are some signs that may point to fertility issues:
- Irregular periods: The average woman’s cycle is about 28 days long. However, if the cycle lasts from 21 to 35 days, it’s still considered normal, as long it is consistent. With irregular periods, the cycle is so unpredictable that it’s impossible to know when the next one will come. This is caused by hormonal issues like thyroid hypo- or hyperfunction, hyperprolactinemia, or polycystic ovarian syndrome (PCOS) — all of which can lead to infertility.
- Absence of periods: Temporary life stress or overexercising may cause you to occasionally skip a period. However, if you haven’t had your period in months, it might be a good idea to seek medical advice.
- Heavy and/or painful periods: Periods that hamper your daily activity may be a symptom of fibroids in the uterus or endometriosis. In fact, endometriosis accounts for roughly 20 to 40 percent of women’s infertility issues.
- Pain during sex: Painful sex for women is so normalized that many think it’s just a part of life. But it may actually point to an underlying condition, such as endometriosis or pelvic inflammatory disease.
- Symptoms of hormonal imbalance: Sudden weight gain, hair loss, constant fatigue, edema, headaches, nipple discharge, facial hair, or severe acne are all signs of possible hormonal disorders. These conditions, in which the body’s hormones are imbalanced, make conceiving more difficult.
- Vaginal soreness and/or itchiness: Soreness or itchiness, especially in combination with discharge, could mean a vaginal infection. If left untreated, infections like chlamydia, gonorrhea, and mycoplasma can eventually lead to infertility.
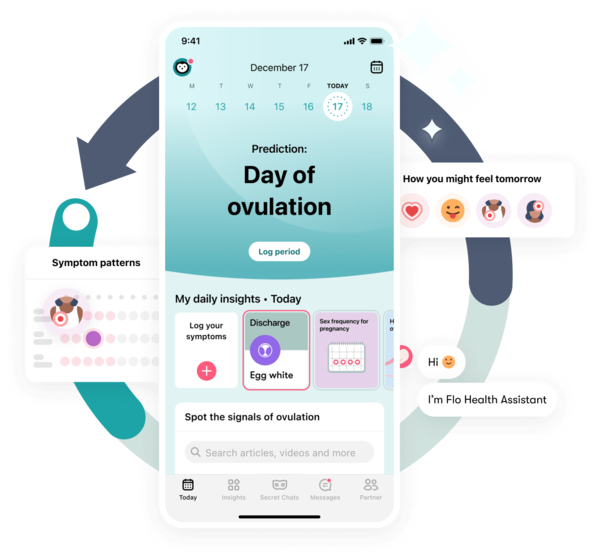
While you’re trying to get pregnant, an ovulation tracking app like Flo can help you manage irregular cycles, spot patterns, and even understand if your symptoms could be related to a condition like endometriosis or PCOS*. You’ll also get a useful health report at the end of every cycle to help you have more informed conversations with your doctor.
*Symptom checker not available in the EU or UK.
The reproductive process

Take a quiz
Find out what you can do with our Health Assistant
In order to successfully conceive, certain reproductive steps must occur, and they are as follows:
- One of the ovaries releases a mature egg.
- The egg travels to the fallopian tube.
- The sperm moves up the cervix, towards the uterus, and into the fallopian tubes to reach and fertilize the egg.
- The fertilized egg moves down the fallopian tube towards the uterus.
- The fertilized egg attaches itself to the uterus (implantation) and begins to grow.
Causes of female infertility
Anything that prevents the above-mentioned steps from happening could be responsible for female infertility. Let’s review some of the most common causes of infertility in women:
Ovulation disorders
Ovulation disorders account for 25 percent of the cases of infertility in women. It occurs when a woman either doesn’t ovulate regularly or doesn’t ovulate at all. Issues with the regulation and production of reproductive hormones are a potential cause. Conditions including PCOS, the presence of excess prolactin, or premature ovarian failure can create ovulation disorders.
Tubal occlusion
According to other research, fallopian tube disorders lead to between 35 and 40 percent of infertility cases. Pelvic inflammatory disease or STIs like chlamydia and gonorrhea may cause these blockages in the fallopian tubes. Previous pelvic surgeries involving the fallopian tubes can also increase your chances of infertility.
Endometriosis
Endometriosis is a condition where the inner lining of the uterus, known as the endometrium, attaches and grows in other areas. These areas include the fallopian tubes, ovaries, small or large intestine, and the walls of the abdominal cavity and pelvis. Such tissue growth and its surgical removal can cause scarring and prevent fertilization.
Uterine and cervical causes
Problems in the uterus or cervix may also affect fertility. Cervical stenosis (a narrowed cervix) or the lack of cervical mucus often make it harder for sperm to travel through the cervix into the uterus. Endometriosis (especially if chronic), uterine fibroids (myomas), or an abnormally-shaped uterus might interfere with conception as well.
Age

As women grow older, it usually becomes more challenging for them to conceive. The quality and quantity of eggs begin to decline by the early 30s and drop even further as a woman approaches the age of 40. This means it’s more difficult to become pregnant and the chance of miscarriage is higher.
Unexplained infertility
Sometimes, doctors are unable to find the reason for infertility, despite running the required fertility tests. Unexplained fertility affects about 10 percent of couples worldwide. Possible causes include the egg not being released at the right time, the egg’s inability to reach the fallopian tube, or the sperm’s inability to reach the egg.

Infertility treatment
Current problems with conception won’t necessarily stop you from starting a family in the future. Many couples with infertility issues go on to have successful pregnancies. There are a wide array of treatments available, each targeting a different cause of infertility, and they include the following:
- Fertility drugs: These drugs work by stimulating the hormones responsible for the maturing and release of the egg and could help those with ovarian disorders. However, there are side effects to using fertility drugs, such as ovarian hyperstimulation or the increased chance of developing ovarian tumors.
- Surgical procedures: These surgeries correct abnormalities or blockages in the uterus and fallopian tubes. Surgical procedures are now rarely used because of the high success rate of other infertility treatments.
- IUI: Fertility doctors may also recommend intrauterine insemination or IUI. In this treatment, millions of healthy sperm are injected into the woman’s uterus at the time of ovulation.
- IVF: The most effective assisted reproductive treatment is in vitro fertilization or IVF. A mature egg is taken from the mother and fertilized with the sperm in a lab. The fertilized egg is then placed back into the uterus. This method takes several weeks and daily hormone injections are needed to ensure successful implantation.
If you’re having trouble conceiving, you are certainly not alone. Signs of infertility include irregular, excessively heavy, or absent periods as well as sudden weight gain, painful sex, or vaginal infections. Female infertility has many possible causes, such as irregular ovulation, uterine fibroids, fallopian tube blockage, PCOS, or endometriosis. Thankfully, there are several options available for treatment, and many useful tips to prepare for conceiving. If you experience any symptoms of infertility, seek advice from a doctor who can diagnose the problem and offer the best treatment for you.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
History of updates
Current version (23 May 2024)
Published (27 March 2019)
In this article
Get your personal guide to fertility
-
Learn how to read your body's ovulation signals
-
Find daily conception tips from our experts
-
Chat with others who are trying to get pregnant




