Have you noticed that you’re ovulating later in your cycle than usual? We ask an obstetrician and gynecologist to explain what might be going on.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Late ovulation: What’s the deal?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Imagine if our cycles ran like clockwork, meaning we could pinpoint the exact moment that we ovulate each month (and, of course, when our period would arrive). This is the case for a lucky few, but for most of us, things aren’t quite that simple.
The moment of ovulation can vary from cycle to cycle, and it’s natural to feel concerned if you realize that you’re ovulating later than your usual pattern. Maybe you’ve started tracking your basal body temperature and were surprised to find the big day didn’t land as you’d expected, or you’ve used an ovulation kit and been confused by the negative result.
Either way, try not to worry (easier said than done, we know). Late ovulation doesn’t always mean that something is wrong and needs treatment. To find out more about what causes late ovulation, we spoke to Flo expert Dr. Jennifer Boyle, obstetrician and gynecologist, Massachusetts General Hospital, US.
Key takeaways
- Late ovulation is when you ovulate anytime after day 21 of your cycle.
- If you ovulate later, then you’re likely to have a longer menstrual cycle, meaning your period will arrive later, too.
- A number of things can mess with ovulation, from conditions like polycystic ovaries to stress.
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
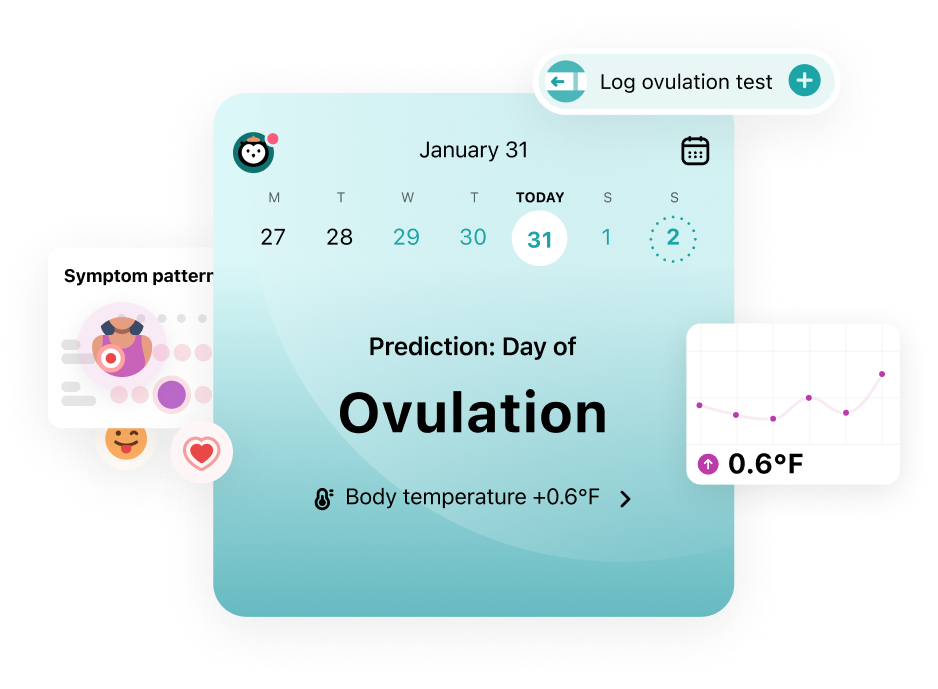
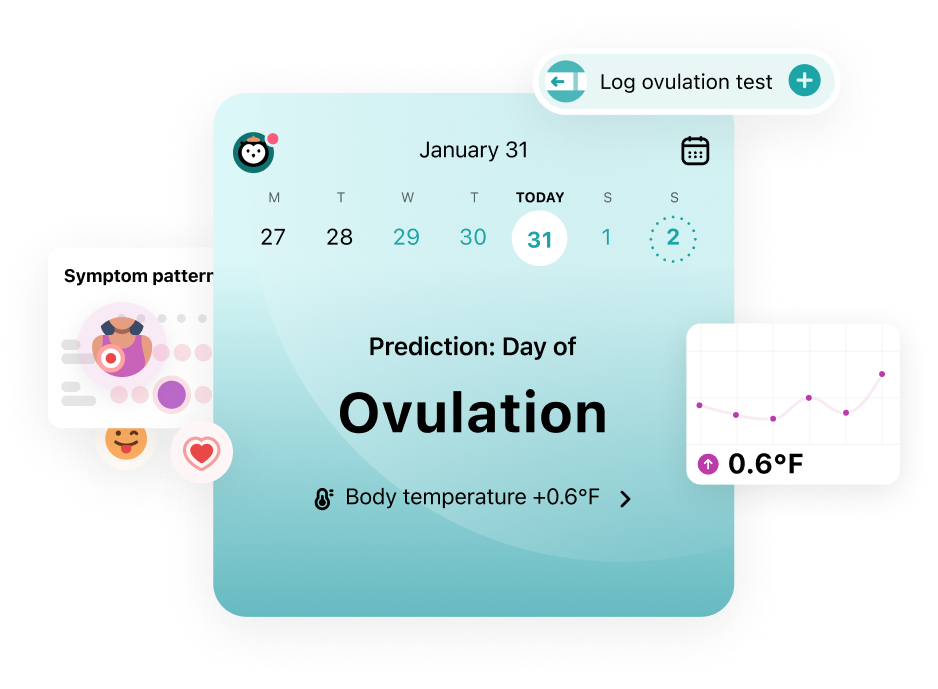
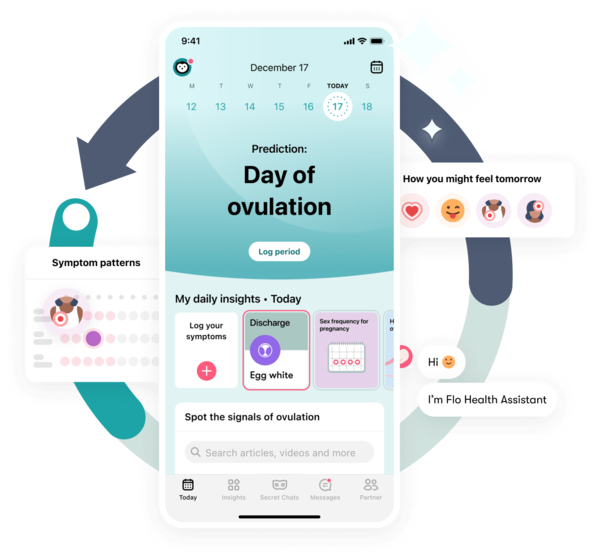
Understand your fertility better with the Flo app
- Learn more about your fertility signals
- Improve ovulation predictions by tracking temperature via Apple Watch
- Log your ovulation test results
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
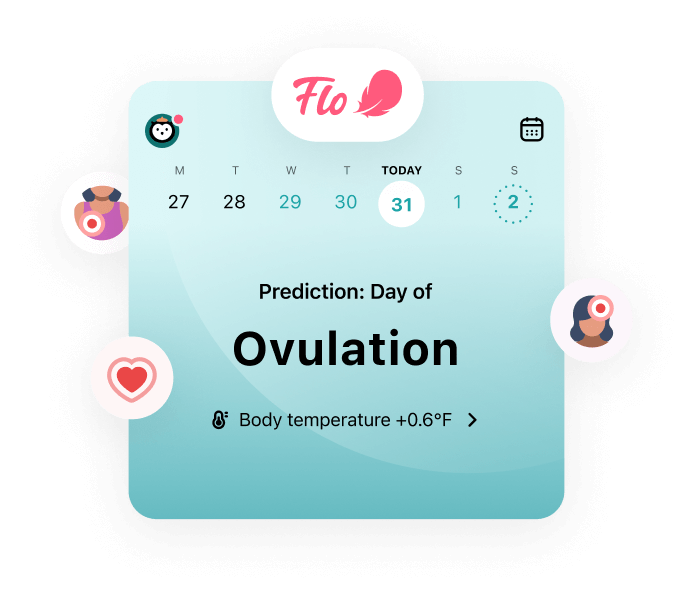
Trying to conceive?
The Flo app can help you better understand your fertility
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
Understand your fertility better with the Flo app
- Learn more about your fertility signals
- Improve ovulation predictions by tracking temperature via Apple Watch
- Log your ovulation test results
Take a quiz
Find out what you can do with our Health Assistant
What is late ovulation?
First, let's look at the definition of ovulation. Ovulation is when one of your ovaries releases an egg, ready to be fertilized by a sperm. If you have an average 28-day cycle, then you’ll usually ovulate around the middle of this, on day 14.
However, not everyone’s cycle lasts for 28 days. In fact, around 84% of women and people with periods have a cycle that is longer or shorter than this, and anything between 21 and 35 days is considered normal. So it might be more helpful to know that ovulation typically takes place around 14 days before your period arrives, no matter how long your cycle is. You can track your periods to figure out your cycle length using an app like Flo.
However, ovulation doesn’t always happen on time. If you ovulate after day 21 of your cycle, then you’re experiencing late ovulation.
Find out how to improve your chances of getting pregnant if your periods are irregular
Does late ovulation mean a late period?
Yes — if you ovulate later than usual in your cycle, then it makes sense that your period will arrive later than usual, too.
What causes late ovulation?
If you’ve realized you’re ovulating later than usual in your cycle, you’re probably eager to know why. Here are some of the potential reasons.
PCOS
You might have heard of polycystic ovarian syndrome (PCOS) but not be totally sure what it is.
PCOS is a common hormonal disorder that affects around 8% to 13% of women of reproductive age worldwide. It can cause your ovaries to grow larger than usual and contain many fluid-filled sacs (called follicles) where your eggs develop.
These follicles aren’t always able to release their eggs, meaning ovulation can happen later than usual or sometimes not at all.
The good news is that there are a number of treatment options available, from taking medication to lifestyle changes, such as exercising more often.
If you’re diagnosed with PCOS, your health care provider can talk you through the options and help you choose what’s best for you.
Breastfeeding
Have you recently had a baby? If so, there could be a simple explanation behind your late ovulation, as research shows that breastfeeding can put a pause on ovulation.
Plus, the more you breastfeed (in terms of how often and how long each feed is), the longer you’ll experience this effect. Researchers aren’t exactly sure why this is, but it could be due to the high levels of prolactin your body produces when you breastfeed.

Hyperprolactinemia
Hyperprolactinemia is when you have high levels of a hormone called prolactin. Prolactin can affect two hormones called luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which are both important for ovulation. This means that having hyperprolactinemia can cause you to ovulate later than usual in your cycle.
Things that can cause high levels of prolactin include damage to your pituitary gland (a small gland in your brain), kidneys, liver, or thyroid.
If you have hyperprolactinemia, your doctor might recommend you take medication to help lower your levels of prolactin, which should help to ease your symptoms.
Medications
Some medications, such as psychotropic drugs, narcotics, and drugs that treat high levels of stomach acid, can also cause hyperprolactinemia.
“If you have noticed a change in your cycles after starting a new medication, you should discuss this with the doctor who prescribed the medication,” says Dr. Boyle.
This is also important if you’re currently trying for a baby. “Part of planning for pregnancy is making sure all of your medications are pregnancy friendly,” adds Dr. Boyle. “Some medications can be stopped as soon as you find out you are pregnant, and some need to be stopped ahead of time.”
Thyroid issues
Ovulation requires a delicate balance of hormones — and not just FSH and LH. You might be surprised to know that hormones produced by your thyroid (the large gland in your neck) play a part too.
If you have thyroid-related medical issues like hypothyroidism (when it’s underactive) or hyperthyroidism (when it’s overactive), then you might also experience irregular cycles or late ovulation. Ask your doctor about medication that can help.
Stress

It’s true: Stress can have a physical impact on your body. “Stress can cause irregular cycles and skipped ovulation,” says Dr. Boyle. This is because increased levels of the stress hormone cortisol can block or delay the all-important spike in LH that makes ovulation happen.
However, this only happens in cases of prolonged or chronic stress. So, if your stress is temporary — for example if you’re rushing to make a deadline at work one week (we’ve all been there) — then the good news is that it’s unlikely to affect your cycle.
Some things that could cause chronic stress are relationship or family issues or a really unsatisfying job. If you think you might be living with chronic stress, know that help is out there, and you’re not alone.
It could be worth looking into stress management techniques such as meditation or yoga, especially if you’re trying for a baby. Dr. Boyle says, “Stress management and stress reduction are crucial when trying for pregnancy, not just to help with becoming pregnant, but because pregnancy, birth, and parenting are inherently stressful experiences … with lots of things one can’t control or predict.”
Age and weight
As you reach perimenopause (the transition to menopause), your estrogen production becomes unpredictable, which can have a ripple effect on when you ovulate and how long your cycles are.
Perimenopause is a natural life stage, just like starting your periods, which will often begin in your 40s but could start anywhere between your late 30s and 50s. It’s often accompanied by symptoms such as hot flashes, brain fog, and irregular cycles. Your doctor can help you manage perimenopause symptoms, so be sure to reach out to them if you need to.
Weight can also impact the timing of ovulation. “Being both underweight and overweight can cause ovulatory problems,” says Dr. Boyle. How so? Being underweight can disrupt the balance of your hormones and lead to anovulation (when ovulation stops happening). Meanwhile, being overweight can cause delayed ovulation because it leads to changes in hormones that can interfere with that delicate hormonal process that makes you ovulate.
If you have any concerns about your weight and how it might be affecting the timing of when you ovulate, your doctor should be able to offer advice and support.
"It is absolutely possible to get pregnant with delayed ovulation"
Late ovulation symptoms
If you’re tracking your cycles with an app like Flo or using ovulation tests, you’ll probably be able to spot when you’re ovulating later than usual. But your body might give you some other telltale signs to look out for:
- No change to your cervical mucus
Your cervical mucus will usually turn wet and slippery, a bit like raw egg whites, just before and during ovulation. This is for a pretty clever reason: It makes it easier for any sperm to swim toward your egg and potentially fertilize it. If you haven’t noticed this type of discharge yet, it could mean you’re ovulating late.
- Irregular basal body temperature (BBT)
Your BBT (your body’s resting temperature) will increase very slightly by around 0.5 to 1 F (0.22 to 0.56 C) just after ovulation. If you measure your BBT and haven’t recorded this change, it could mean that you haven’t ovulated yet.
- Delayed period
The length of the second half of your cycle usually stays pretty constant, so if your period is late, it could mean that you’ve ovulated later than usual.
Can you ovulate late and still get pregnant?
Yes, it is absolutely possible to get pregnant with delayed ovulation — it would just happen a bit later in your cycle. In one study, women who ovulated late had around the same chances of conceiving per cycle (22%) as the participants in the study overall (21%).
Late ovulation treatment: Do I need it?
Late ovulation doesn’t always need treatment, especially if it’s a one-off. However, if late ovulation is causing you to have irregular or abnormal cycles, your health care provider might recommend some options to help.
“The treatments can include lifestyle modifications such as stress management, nutrition changes, and trying to get your weight into a healthy range if it is not already there,” says Dr. Boyle. “Sometimes, medications to help someone ovulate more regularly are prescribed.”
These medications could include clomiphene citrate, a tablet that helps stimulate ovulation, and gonadotropins, an injection that helps your ovaries produce more eggs. Your doctor will be able to help you decide which option could work best for you.
When to see your doctor
It’s always a good idea to speak to your doctor if you’ve noticed that you’re regularly ovulating later than usual or if you have irregular cycles. “They will make sure your irregular cycles aren’t due to a medical problem,” says Dr. Boyle.
This could include some of the causes of late ovulation that we looked at earlier, such as PCOS, hyperprolactinemia, or thyroid issues. Your doctor will examine you and run any necessary tests to help work out what could be going on. They will also be able to discuss any treatment options needed with you and, most importantly, answer any questions you might have.
Your doctor can also offer you some advice on getting pregnant with late ovulation if needed. “They can also help you better understand your fertile window and when to have sex [for the best chance of conceiving], taking into consideration how your cycle varies,” says Dr. Boyle.
More FAQs
Will late ovulation delay a positive pregnancy test?
Yes, late ovulation can delay a positive pregnancy test. This is because a test can’t detect a pregnancy before implantation has occurred.
This is when a fertilized egg burrows into your uterus, which usually happens around six to 10 days after conception. So, if you’ve ovulated later than usual, fertilization and implantation will happen later, too.
Does late ovulation mean a late due date?
If you ovulate late, then using the date of your last menstrual period to figure out your due date can be frustratingly unreliable.
But rest assured that your dating ultrasound will provide a much more accurate idea of when your baby is due. This is where a doctor measures the size of your baby to work out when you’re due, and you could have it as early as 7 to 8 weeks pregnant, depending on your provider.
Can you get pregnant if you ovulate early?
Yes, you can. There’s no evidence that early ovulation affects egg quality or fertility. One study showed that women can ovulate as early as day eight of their cycle and still go on to have a healthy baby.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Anovulation.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21698-anovulation. Accessed 9 Jan. 2024.
Boutari, Chrysoula, et al. “The Effect of Underweight on Female and Male Reproduction.” Metabolism: Clinical and Experimental, vol. 107, June 2020, https://doi.org/10.1016/j.metabol.2020.154229.
Burkman, Ronald T. “Perimenopause.” Obstetrics and Gynecology Clinics of North America, vol. 29, no. 3, Sep. 2002, pp. xi – xii, https://doi.org/10.1016/S0889-8545(02)00018-9.
Chao, S. “The Effect of Lactation on Ovulation and Fertility.” Clinics in Perinatology, vol. 14, no. 1, Mar. 1987, pp. 39–50, https://doi.org/10.1016/S0095-5108(18)30780-2.
“Chronic Stress.” Yale Medicine, www.yalemedicine.org/conditions/stress-disorder. Accessed 9 Jan. 2024.
“Female Infertility.” Mayo Clinic, 27 Aug. 2021, www.mayoclinic.org/diseases-conditions/female-infertility/diagnosis-treatment/drc-20354313.
“Fertility Awareness-Based Methods for Family Planning: A Literature Review.” Journal of Christian Nursing, vol. 37, no. 4, Oct/Dec 2020, pp. E47–48, https://doi.org/10.1097/cnj.0000000000000758.
Greendale, G. A., et al. “The Menopause.” The Lancet, vol. 353, no. 9152, Feb. 1999, pp. 571–80, https://doi.org/10.1016/s0140-6736(98)05352-5.
Grieger, Jessica A., and Robert J. Norman. “Menstrual Cycle Length and Patterns in a Global Cohort of Women Using a Mobile Phone App: Retrospective Cohort Study.” Journal of Medical Internet Research, vol. 22, no. 6, June 2020, https://doi.org/10.2196/17109.
“Hyperprolactinemia.” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/hyperprolactinemia. Accessed 9 Jan. 2024.
“Hyperthyroidism (Overactive Thyroid).” Mayo Clinic, 30 Nov. 2022, www.mayoclinic.org/diseases-conditions/hyperthyroidism/symptoms-causes/syc-20373659.
“Hypothyroidism and Infertility: Any Connection?” Mayo Clinic, 20 May 2023, www.mayoclinic.org/diseases-conditions/female-infertility/expert-answers/hypothyroidism-and-infertility/faq-20058311.
“Implantation Bleeding.” Cleveland Clinic, my.clevelandclinic.org/health/symptoms/24536-implantation-bleeding. Accessed 9 Jan. 2024.
Koyyada, Arun, and Prabhakar Orsu. “Role of Hypothyroidism and Associated Pathways in Pregnancy and Infertility: Clinical Insights.” Tzu Chi Medical Journal, vol. 32, no. 4, Apr. 2020, pp. 312–17, https://doi.org/10.4103%2Ftcmj.tcmj_255_19.
“Irregular Periods.” NHS, www.nhs.uk/conditions/irregular-periods/. Accessed 9 Jan. 2024.
Davis, Joseph B., and James H. Segars. “Menstruation and Menstrual Disorders: Anovulation.” Global Women’s Medicine, May 2009, www.glowm.com/section-view/heading/Menstruation%20and%20Menstrual%20Disorders:%20Anovulation/item/295\.
“Methods for Estimating the Due Date.” The American College of Obstetricians and Gynecologists, May 2017, www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/05/methods-for-estimating-the-due-date.
“Ovulation.” Cleveland Clinic, my.clevelandclinic.org/health/articles/23439-ovulation. Accessed 9 Jan. 2024.
“Menopause 101: A Primer for the Perimenopausal.” The North American Menopause Society, www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal. Accessed 9 Jan. 2024.
“Overview: Polycystic Ovary Syndrome.” NHS, www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/. Accessed 9 Jan. 2024.
“Polycystic Ovary Syndrome.” World Health Organization, 28 June 2023, www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome.
“Polycystic Ovary Syndrome (PCOS).” Mayo Clinic, 8 Sep. 2022, www.mayoclinic.org/diseases-conditions/pcos/diagnosis-treatment/drc-20353443.
Reed, Beverly G., and Bruce R. Carr. “The Normal Menstrual Cycle and the Control of Ovulation.” Endotext. MDText.com, Inc., 5 Aug. 2018, www.ncbi.nlm.nih.gov/books/NBK279054/.
Steward, Kaitlyn, and Avais Raja. “Physiology, Ovulation and Basal Body Temperature.” StatPearls. StatPearls Publishing, 17 July 2023, https://www.ncbi.nlm.nih.gov/books/NBK546686/.
“Stress Relief.” Mayo Clinic, 18 Nov. 2023, www.mayoclinic.org/healthy-lifestyle/stress-management/basics/stress-relief/hlv-20049495.
Su, Ren-Wei, and Asgerally T. Fazleabas. “Implantation and Establishment of Pregnancy in Human and Nonhuman Primates.” Advances in Anatomy, Embryology, and Cell Biology, vol. 216, 2015, pp. 189–213, https://doi.org/10.1007%2F978-3-319-15856-3_10.
“Ultrasound in Pregnancy.” Cleveland Clinic, my.clevelandclinic.org/health/diagnostics/9704-ultrasound-in-pregnancy. Accessed 9 Jan. 2024.
“Weight, Fertility, and Pregnancy.” Office on Women’s Health, 17 Feb. 2021, www.womenshealth.gov/healthy-weight/weight-fertility-and-pregnancy.
Wilcox, Allen J., et al. “Natural Limits of Pregnancy Testing in Relation to the Expected Menstrual Period.” JAMA, vol. 286, no. 14, Oct. 2001, pp. 1759–61, https://doi.org/10.1001/jama.286.14.1759.
Wilcox, A. J., et al. “The Timing of the ‘Fertile Window’ in the Menstrual Cycle: Day Specific Estimates from a Prospective Study.” BMJ, vol. 321, no. 7271, Nov. 2000, pp. 1259–62, https://doi.org/10.1136/bmj.321.7271.1259.
History of updates
Current version (10 January 2024)
Published (02 May 2019)
In this article
Get your personal guide to fertility
-
Learn how to read your body's ovulation signals
-
Find daily conception tips from our experts
-
Chat with others who are trying to get pregnant




