Cervical cancer awareness has increased over the last two decades, but there’s always more to know. Here, an OB-GYN (obstetrician-gynecologist) explains how the four stages of cervical cancer are identified and the importance of cervical cancer screenings.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Cervical cancer stages: Signs, treatments, and prevention

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.

If you or someone you know is going through a difficult time, remember that there are ways to get help. Here are some support services and resources in your country.
Find out moreAs the name suggests, cervical cancer occurs when cancerous cells grow in the cervix. It’s the fourth most common type of cancer in women, and it’s classified in four different stages depending on how much it’s spread to other parts of the body.
You might have heard of your cervix but not be totally sure where it is. It’s the small, round, firm passageway that connects the bottom of your uterus to your vagina. Over the last couple of decades, medical professionals have worked tirelessly to raise awareness of the preventative measures you can take against cervical cancer.
The Centers for Disease Control and Prevention report that more than nine of every ten cases of cervical cancer are caused by human papillomavirus infection (HPV), so attending your pap smear and having the HPV vaccine could be life-saving.
“Cervical cancer, while we have certainly come a long way in reducing incidence and mortality over the past few decades, still requires our full attention,” says Dr. Angela Jones, board-certified obstetrics and gynecology expert.
“In accordance with the American Cancer Society, approximately 14,100 new cases of invasive cervical cancer will be diagnosed, and roughly 4,280 women will die from cervical cancer in the United States in 2022.”
Below, Dr. Jones explains how the different stages of cervical cancer are classified, plus when and how to book regular pap smears.
What are the four stages of cervical cancer?
Any cancer diagnosis is difficult to deal with. You might feel scared, alone, or unsure about who you can speak to. That’s OK. Know that there are lots of places you can go for support.
Learning more about the type of cancer you have been diagnosed with can help you feel more in control of your treatment options and may help you to recognize any symptoms. So let’s start by finding out the facts about cervical cancer.
"[Most] cases of cervical cancer are caused by human papillomavirus infection (HPV), so attending your pap smear and having the HPV vaccine could be life-saving"
Cancer is named after the place in the body where it started. So, even if it spreads, cervical cancer describes cancer that begins in the cervix. It’s one of five gynecological cancers.
There are four main stages of cervical cancer. Stage one is the least severe, and four indicates that the cancer has spread to other parts of the body like the bones, lungs, and kidneys. This stage is also described as metastatic cancer.
Wrapping your head around each of the cervical cancer stages can be confusing. However, your health care provider will be able to explain all the characteristics of each stage, including the size and depth of the cancer and if it’s spread to any of your other reproductive organs or anywhere else in your body.
Each stage is categorized by some key features:
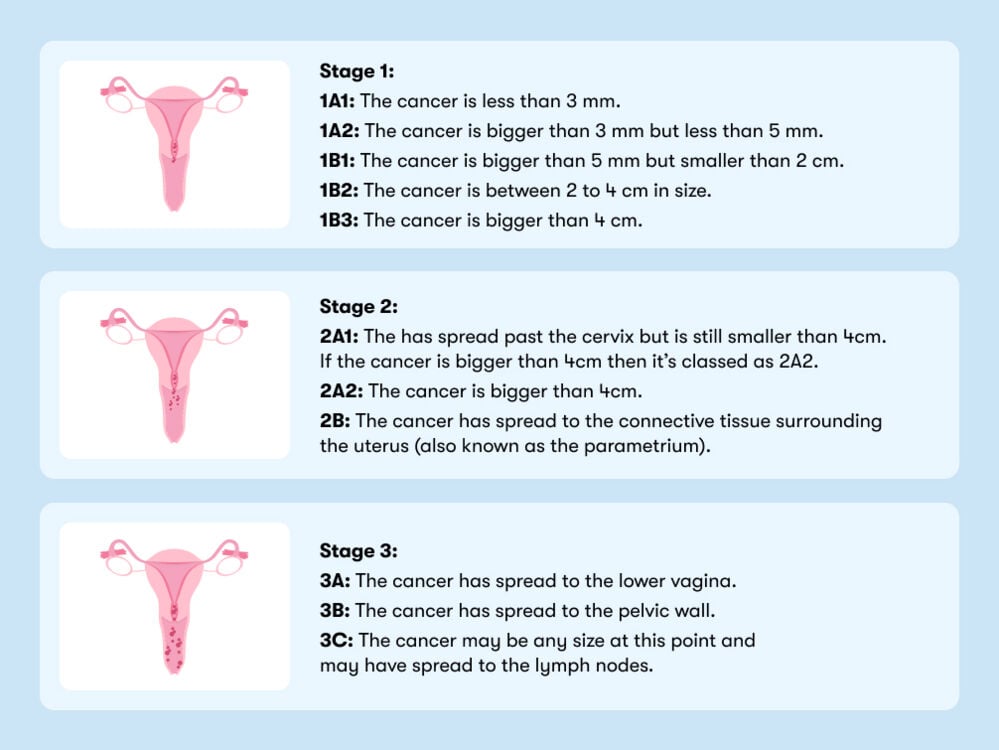
Stage 4: In stage 4, cervical cancer has spread to other parts of the body, such as the bladder, bones, liver, or lungs. This is the most advanced stage of cervical cancer.
What are the symptoms of cervical cancer in the early stages?
Cervical cancer symptoms may be different for each person and often depend on how far the cancer has progressed. “Early-stage cervical cancer may have few to no symptoms, which is why screening is so important,” says Dr. Jones. To learn more about what exactly happens at your pap smear appointment, then keep reading.
Dr. Jones explains that advanced cervical cancer symptoms may include:
- Bleeding after sex
- Unusually long and heavy periods
- Bleeding between periods
- Bleeding that occurs after menopause
- Watery, bloody vaginal discharge
- Vaginal discharge with an odor
- Pelvic pain
- Pain during sex
It’s really important to note that if you experience any of these symptoms, you shouldn’t automatically assume that you have cervical cancer. You may experience these symptoms for a multitude of reasons, so try not to worry if you notice a change. What’s important is to speak to your health care provider as soon as possible.
How is cervical cancer diagnosed?
To get to the bottom of the symptoms you might be experiencing, your medical professional may ask you about your medical history and run a series of tests.
To assess any pains or abnormal bleeding, they may do an internal examination using a speculum. They will first examine your vulva. Then, using the speculum, they will look at your cervix. If at any point before or during your examination you feel any pain or are uncomfortable, you are well within your right to ask your health care provider to stop or to explain what they’re doing and why.
"One of the key things that most of the women I’ve ever diagnosed with cervical cancer had in common was they hadn’t had a pap smear in years"
They might also conduct a pap smear at the same time. Using a swab, they will take a sample of cells from your cervix to test for any abnormal changes. The pap smear can be used to test for human papillomavirus (HPV).
If they notice any abnormalities, then they may recommend that you have a colposcopy.
A colposcope is an instrument that has magnifying lenses and allows them to see the cervix in detail. A special solution is usually applied to the cervix to show abnormal areas. During the procedure, it is possible to take a piece of cervical tissue for examination — a biopsy. This means you’ll have a small amount of tissue removed from your cervix to be examined under a microscope.
How is cervical cancer treated?
Treating cervical cancer isn’t a one-size-fits-all approach. Treatment options vary depending on the stage of cervical cancer, as well as other factors like age, overall health, and your personal preferences.
While your health care provider will take all these things into consideration before presenting you with treatment options, you should also be given the opportunity to ask questions about how treatment could impact your sex life, your ability to have children, and if it will trigger early menopause.
The most common treatment options include:
- Surgery: Surgery is often used to remove cervical cancer. If the cancer is very small, then you may opt to have part of your cervix removed. If it’s larger, then you may have the cervix and part of the vagina removed. And if the cancer has spread further, then you may have your cervix and uterus removed. This is known as a hysterectomy and means you will no longer be able to carry a pregnancy. Surgery is more common during the early stages of cancer (before it has spread outside of the pelvis).
- Radiation therapy: Radiation therapy uses high-energy X-rays to kill cancer cells. It’s often used in combination with surgery to prevent the cancer from coming back.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It may be given alone or in combination with radiation therapy and is common for all stages when the cancerous cells have spread outside the uterus. Chemotherapy may also be used before surgery to shrink the cancer. Common chemotherapy drugs include cisplatin, carboplatin, or a combination of cisplatin and fluorouracil.
- Targeted therapy: Targeted therapy is a newer type of cancer treatment that uses drugs or other substances to target and kill cancer cells. It works by interfering with the way cancer cells grow and divide. Common targeted therapies for cervical cancer include bevacizumab (Avastin) and tisotumab vedotin-tftv (Tivdak).
- Immunotherapy: Immunotherapy is a type of targeted therapy that uses the body's immune system to fight cancer. It works by helping the body's immune system to recognize and kill cancer cells. Pembrolizumab (Keytruda) is an example of an immunotherapy drug used to treat cervical cancer.
How can cervical cancer be prevented?
They say prevention is better than a cure, and luckily, cervical cancer screenings can detect precancerous cells early — when they’re most treatable. Dr. Jones recommends following the American College of Obstetrics and Gynecology (ACOG) cervical cancer screening guidelines:
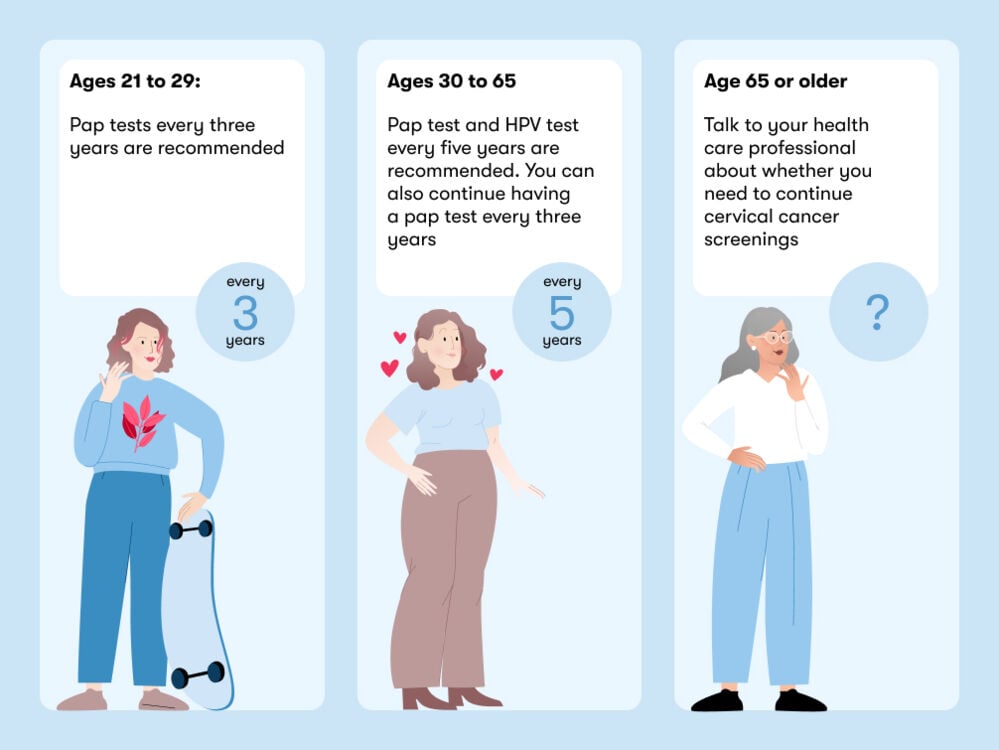
The regularity and timing of your pap test can vary depending on where you live. In the US, you will be invited for your first pap smear after you turn 21. In the UK, you’ll have your first screening around the age of 25. If you’ve had an abnormal pap smear in the past, you may be invited to have screenings more frequently, and you can begin to have annual wellness visits with your gynecologist once you’re 18. They will be able to advise you on when to come in for your first pap smear and what will happen.
Screenings are important, but they’re not the only way to prevent cervical cancer. “Lifestyle modifications such as not smoking and practicing safe sex are also helpful in reducing risks,” explains Dr. Jones, who adds that the HPV vaccine can also help prevent cervical cancer.
Cervical cancer vaccine: How does it work?
The cervical cancer vaccine works by protecting against HPV (the virus that can cause cervical cancer). It does this by stimulating the body to produce antibodies against the virus.
According to the National Cancer Institute, the HPV vaccine is most effective if you have it before you have sex for the first time. This is because HPV is usually spread through sexual contact. However, the HPV vaccine is still effective if you’re already sexually active. It’s given as a series of two to three shots, depending on age. The shots are usually given at least six months apart.
The HPV vaccine is available at most health care provider offices, as well as community health centers, pharmacies, and some schools. Speak to your health care provider for more information on where you can get vaccinated.
Cervical cancer: The takeaway
As with any type of cancer, prevention and early detection make a world of difference. But it’s also important to remember that cervical cancer is treatable — and there are many treatment options available.
“Regardless of which option you choose, ensuring that you are getting some sort of screening is key,” Dr. Jones says. “In all my years of practice, one of the key things that most of the women I’ve ever diagnosed with cervical cancer had in common was they hadn’t had a pap smear in years.”


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Cancers Caused by HPV.” Centers for Disease Control and Prevention, 23 Mar. 2022, https://www.cdc.gov/hpv/parents/cancer.html. Accessed 25 May 2022.
“Cervical Cancer.” World Health Organisation, https://www.who.int/health-topics/cervical-cancer. Accessed 25 May 2022.
“Cervical Cancer Statistics.” National Cancer Institute, https://www.cancer.org/cancer/cervical-cancer/about/key-statistics.html. Accessed 25 May 2022.
“Cervical Cancer Tests.” National Cancer Institute, https://www.cancer.org/cancer/cervical-cancer/detection-diagnosis-staging/how-diagnosed.html. Accessed 25 May 2022.
“Cervical Cancer Treatment.” National Cancer Institute, https://www.cancer.org/cancer/cervical-cancer/treating.html. Accessed 25 May 2022.
“HPV Vaccination: What Everyone Should Know.” Centers for Disease Control and Prevention, 6 May 2022, https://www.cdc.gov/vaccines/vpd/hpv/public/index.html. Accessed 25 May 2022.
“Human Papillomavirus (HPV) Vaccines.” National Cancer Institute, 18 June 2021, https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet. Accessed 25 May 2022.
Mwaka, Amos D., et al. “Awareness of Cervical Cancer Risk Factors and Symptoms: Cross-Sectional Community Survey in Post-Conflict Northern Uganda.” Health Expectations: An International Journal of Public Participation in Health Care and Health Policy, vol. 19, no. 4, Aug. 2016, pp. 854–67. Accessed 25 May 2022.
“NCI Dictionary of Cancer Terms.” National Cancer Institute, 2 Feb. 2011, https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cervical-cancer. Accessed 25 May 2022.
Petignat, Patrick, and Michel Roy. “Diagnosis and Management of Cervical Cancer.” BMJ , vol. 335, no. 7623, Oct. 2007, pp. 765–68. Accessed 25 May 2022.
“Treatment for Cervical Cancer.” NHS, https://www.nhs.uk/conditions/cervical-cancer/treatment/. Accessed 25 May 2022.
“Updated Cervical Cancer Screening Guidelines.” American College of Obstetricians and Gynecologists, https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2021/04/updated-cervical-cancer-screening-guidelines. Accessed 25 May 2022.

