It’s pretty surprising how many colors your discharge can be. Here’s what you need to know if you see green.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Green vaginal discharge: What is it, and why does it happen?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Have you noticed green discharge in your underwear or when you wipe? A change in the way your vaginal discharge looks and smells can be alarming, but try not to panic. Here’s everything you need to know about green discharge — from what causes it to how to talk to your doctor about it.
Key takeaways
- Most often, green discharge is a sign of an infection. But if you see it, don’t worry — we’ll explain what to do next.
- This article will talk about how conditions like bacterial vaginosis (BV), some sexually transmitted infections (STIs), and pelvic inflammatory infection (PID) can change the way your discharge looks and smells.
- If you notice a change in how your discharge looks, smells, or feels, speak to your health care provider. While you might not be used to talking about discharge, rest assured that it’s no big deal to doctors. They’ll just be interested in making sure you get the right treatment as quickly as possible.
What is green vaginal discharge?
You might notice discharge in your underwear that looks slightly different throughout your cycle. Sometimes, it could be creamy or wet, while other times, it might look stringy like egg whites. It shouldn’t have a strong smell and may be clear, white, or off-white.
It can be hard to know what’s “normal” when you only have your body to go by, but this type of vaginal discharge is very typical. The hormone estrogen can influence the texture of your discharge and how much discharge you have at any point in your cycle. It’s mostly made up of mucus, fluid, and skin cells and is produced by the glands inside your vagina and cervix (the tube-like muscle that attaches your vagina to your uterus) throughout your cycle.
Your discharge can tell you a lot about your vaginal health overall. One of its main responsibilities is to flush out dead cells and bacteria, protecting you from infections. It also provides lubrication, preventing vaginal dryness and irritation. Pretty clever, right?
Chances are you probably already know what your discharge looks like, and if you’re reading this wondering why yours now appears green, then there could be a fairly straightforward answer. Typically, green discharge means that you have some kind of infection. While this might be scary, the good news is that many infections are easily treated, so speak to your doctor.
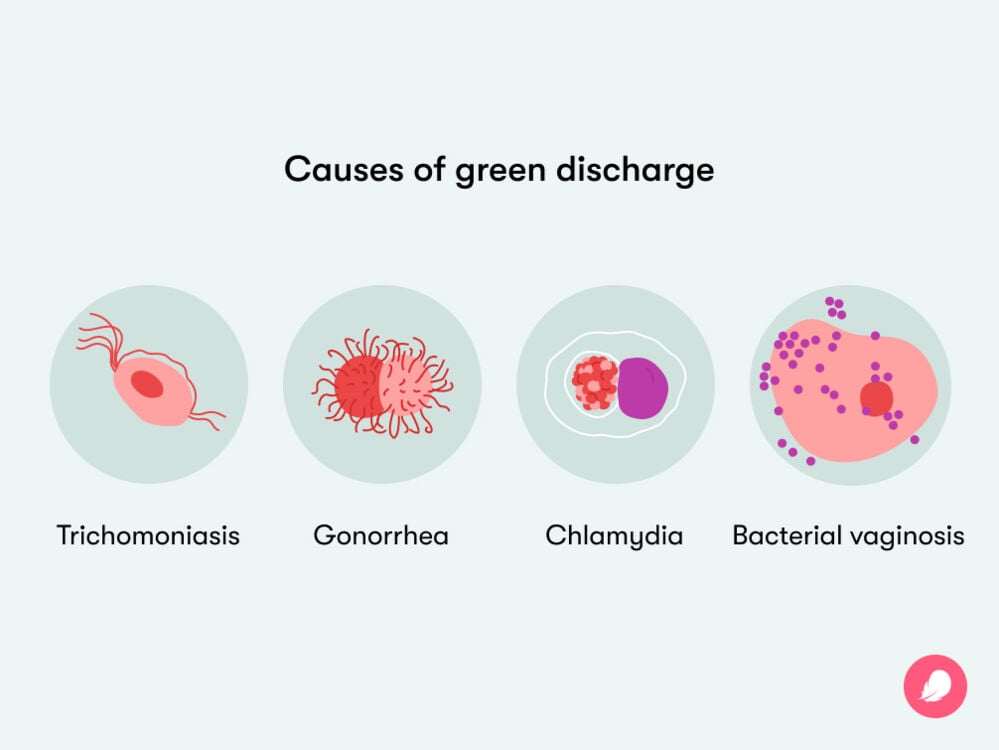
What can cause green discharge?
Reading that you might have an infection can sound alarming, but fear not. Many conditions can be treated easily with a course of antibiotics. It’s nothing to be embarrassed or ashamed about. There are a few different things that could cause infection and green discharge, including:
Bacterial vaginosis (BV)
If your discharge appears to be off-white, gray, or greenish, then it could be a sign of bacterial vaginosis (BV). BV is an infection that’s often characterized by a strong, fishy smell and itching around your vulva.
You might be reading this thinking, “What in the world is BV?” Put simply, BV is caused by a change in the natural balance of bacteria in your vagina. While we often associate bacteria with being a bad thing, there are lots of different types of bacteria that make up your vaginal microbiome. This is the clever system that protects your vagina from infections.
You might experience an imbalance in your vagina’s natural bacteria if you use strongly scented products when washing your vagina. Similarly, douching or using cleansers isn’t recommended, and this can cause an infection. Remember, your vagina is self-cleaning, so all you need to use is water.
If you recognize some of these symptoms, then book an appointment with your doctor. BV is easily treated with a course of antibiotics.
Sexually transmitted infections (STIs)
Green vaginal discharge could also be a sign of an STI, including gonorrhea, chlamydia, or trichomoniasis. A change in the color of your discharge isn’t the only discharge symptom often linked to STIs. Your discharge may also:
If you recognize any of these symptoms, the best thing to do is book an STI screening with your health care provider. Generally speaking, these tests are quick and painless. Your doctor will be able to tell you if you have an STI and what the best course of medication is.
Going for an STI test might not be your ideal way to spend an afternoon, but it’s crucial that you stay on top of your sexual health care. If left unchecked, STIs can get worse, and your symptoms may become more severe as time goes on. You may develop other conditions, such as pelvic inflammatory disease or complications if you try to get pregnant in the future. So, if it’s possible you could have an STI, speak to your doctor as soon as you can. It’s important to be able to let any partners you’ve had recently know that they should get checked too.
Pelvic inflammatory disease (PID)
Another reason why you might notice a change in the way your discharge looks and smells is if you’ve got a condition known as pelvic inflammatory disease (PID).
PID isn’t an STI, but it can be caused when an STI is left untreated, as bacteria enter your reproductive tract, impacting your uterus, ovaries, and uterine tubes.
PID can cause abdominal pain, irregular bleeding between your periods, and pain during sex. If your doctor suspects you have PID, they may recommend you take antibiotics to tackle the original cause of the infection.
Foreign objects
You might read this and wonder what a foreign object is and how it might lead to green discharge. A foreign object is something that might be inserted in your body that doesn’t belong there, like a tampon that you’ve been wearing for too long or a condom that’s slipped off after sex and left inside you.
As your vagina is a warm, moist environment, bacteria can grow and thrive, especially if there’s something inside you that shouldn’t be. For example, if you leave a tampon in for longer than the recommended eight-hour window, it may continue to soak up blood, and bacteria may grow. In some very rare cases, this can lead to toxic shock syndrome (TSS). TSS happens when bacteria that produce toxins grow in your vagina, enter your bloodstream, and spread through the body, leading to symptoms like nausea and vomiting, a fever, and muscle aches, which can be life-threatening.
Only around one to three people in every 100,000 will experience TSS, but if you have any of these symptoms, get medical help immediately. Your doctor may be able to offer you antibiotics to treat TSS.
What does green discharge during pregnancy mean?
While this might not have been on your list of pregnancy symptoms, many people notice that they have more discharge in the early stages of pregnancy. This is due to changes in your hormone levels that can lead you to have more cervical mucus. It might appear thicker, and this is crucial in protecting you from infections and bacteria traveling up your vagina to your uterus.
However, green discharge during pregnancy could also suggest that you have an infection. Whether you’re expecting or not, it’s important to reach out to your health care provider if you spot green discharge in your underwear.
How can I prevent green discharge?
So, how can you ensure that both you and your discharge stay healthy? A good thing to remember is that vaginas are self-cleaning, and strong soaps and detergents can cause more harm than good. While you might want to reach for your favorite body wash to clean your vulva, it doesn’t take a lot to maintain its balance.
To help prevent infections that might cause green discharge, here are some ideas to think about:
- Only use water or a mild soap: Your vagina is a sensitive area, and using harsh, perfumed soaps can lead to irritation and infection. Plain, unperfumed soap or just water is best. Perfumed products may smell good, but they can change your vagina’s pH levels and could cause an infection.
- For similar reasons, you don’t need to douche or spray water into your vagina.
- Wear loose-fitting, cotton underwear. Cotton is breathable and soft, so it won’t rub against or irritate the skin around your vulva.
- When you’re on your period, change your pad or tampon every four to eight hours to avoid a buildup of bacteria.
- Use barrier protection like a condom during sex.
- When you go to the bathroom, always wipe from front to back.
Take a quiz
Find out what you can do with our Health Assistant
When to see your doctor and what to say
We get you — it may feel a little embarrassing to talk to your doctor about green vaginal discharge. But the best thing to do if you notice a change in the way your discharge smells or looks is to head to your health care provider to get checked out. Antibiotics are usually all it takes to treat all of these conditions — and it’s best to start treatment right away because leaving an infection untreated can lead to complications.
Other signs of infection include burning, pain, and itching when you pee; bleeding between periods; and lower abdominal pain. Tracking any symptoms you experience using an app like Flo may come in handy if you go to the doctor because you can have all the information at hand. Some infections like STIs are often symptomless, so even if a change in discharge is all you notice, it’s important not to ignore it.
More FAQs
Can green discharge be treated naturally?
No, green discharge shouldn’t be treated at home with natural products. Generally speaking, green discharge is a sign of an infection, so it’s important that you speak to your doctor about the best way to treat it.
Can a pH imbalance cause green discharge?
Yes! A pH imbalance in your vagina may be due to an infection, so it can be linked to green discharge. While hearing the term pH may throw you back to biology class, your vagina naturally has a slightly acidic pH of four to 4.5. If the pH of your vagina is higher or more alkaline than this, it would suggest an imbalance, meaning you may have a condition like BV — for which greenish discharge is a symptom.
How do you get Gardnerella vaginalis?
You can’t “get” Gardnerella vaginalis because Gardnerella vaginalis is the scientific name for the natural “good” bacteria that grow in your vagina, protecting it from infections. It grows in perfect balance to make up your vaginal microbiome. However, if too much Gardnerella vaginalis grows, you might develop an infection like BV.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Bacterial Vaginosis.” Mayo Clinic, 10 June 2023, www.mayoclinic.org/diseases-conditions/bacterial-vaginosis/symptoms-causes/syc-20352279.
“Foreign Bodies.” MedlinePlus, Aug. 2010, medlineplus.gov/foreignbodies.html.
“Is It Normal to Have Vaginal Discharge?” The American College of Obstetricians and Gynecologists, Oct. 2020, www.acog.org/womens-health/experts-and-stories/ask-acog/is-it-normal-to-have-vaginal-discharge.
Kairys, Norah, et al. “Gardnerella Vaginalis.” StatPearls, StatPearls Publishing, Nov. 2023, www.ncbi.nlm.nih.gov/books/NBK459350/.
Khaskheli, Meharunnissa, et al. “Vaginal Discharge during Pregnancy and Associated Adverse Maternal and Perinatal Outcomes.” Pakistan Journal of Medical Sciences Quarterly, vol. 37, no. 5, Sep.–Oct. 2021, pp. 1302–08, doi:10.12669/pjms.37.5.4187.
“Patient Education: Vaginal Discharge in Adult Women (Beyond the Basics).” UpToDate, 13 Mar. 2023, www.uptodate.com/contents/vaginal-discharge-in-adult-women-beyond-the-basics/print.
“Pelvic Inflammatory Disease (PID).” Mayo Clinic, 30 Apr. 2022, www.mayoclinic.org/diseases-conditions/pelvic-inflammatory-disease/symptoms-causes/syc-20352594.
Brusch, John L. “Prevention of Urinary Tract Infection (UTI) in Women.” Medscape, 1 Apr. 2021, emedicine.medscape.com/article/1958794-overview.
Schwebke, Jane R. “Bacterial Vaginosis.” Current Infectious Disease Reports, vol. 2, no. 1, Feb. 2000, pp. 14–17, https://doi.org/10.1007/s11908-000-0082-0.
“Sexually Transmitted Disease (STD) Symptoms.” Mayo Clinic, 5 May 2022, www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081.
“Sexually Transmitted Infections.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/9138-sexually-transmitted-diseases--infections-stds--stis. Accessed 23 Jan. 2024.
Solomons, Edward, and Gerald C. Dockeray. “Vaginal Discharges.” Irish Journal of Medical Science, vol. 11, Aug. 1936, pp. 548–51, https://doi.org/10.1007/BF02957053.
Soper, David E. “Pelvic Inflammatory Disease (PID).” Infectious Diseases in Obstetrics and Gynecology, vol. 4, no. 2, Feb. 1996, p. 62, doi:10.1155/S1064744996000130.
“Toxic Shock Syndrome (TSS).” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/toxic-shock-syndrome-tss. Accessed 23 Jan. 2023.
“Vaginal Discharge.” Mayo Clinic, 25 Apr. 2023, www.mayoclinic.org/symptoms/vaginal-discharge/basics/definition/sym-20050825.
Barad, David H. “Vaginal Discharge.” MSD Manual Consumer Version, Sep. 2022, www.msdmanuals.com/en-gb/home/women-s-health-issues/symptoms-of-gynecologic-disorders/vaginal-discharge.
“Vaginal Discharge in Pregnancy.” NHS, www.nhs.uk/pregnancy/related-conditions/common-symptoms/vaginal-discharge/. Accessed 23 Jan. 2023.
“Vaginal Odor.” Cleveland Clinic, my.clevelandclinic.org/health/symptoms/17905-vaginal-odor. Accessed 23 Jan. 2024.
“Vaginitis.” Mayo Clinic, 22 Dec. 2021, www.mayoclinic.org/diseases-conditions/vaginitis/symptoms-causes/syc-20354707.
“Vulvovaginitis.” Nelson Essentials of Pediatrics Eighth Edition, edited by Karen J. Marcdante and Robert M. Kliegman, Elsevier Inc., 2019, pp. 417–19, dl.cafepezeshki.ir/book/Nelson-Essentials-of-Pediatrics-8th-Edition(www.CafePezeshki.IR).pdf.
“What Happens if You Leave a Tampon in Too Long?” Cleveland Clinic, 8 Sep. 2022, health.clevelandclinic.org/what-happens-if-you-leave-a-tampon-in-too-long.
“You Don’t Need Fancy Products for Good Feminine Hygiene.” Mayo Clinic Health System, 2 Nov. 2016, www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/you-dont-need-fancy-products-for-good-feminine-hygiene.




