If birth control stops you from getting pregnant, does this mean that you don’t ovulate? Find out how birth control impacts ovulation and whether it’s safe to use long term, with advice from a Flo expert.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Do you ovulate on birth control? Here’s what you need to know


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
For many of us, being on hormonal birth control is an obvious choice (hello clearer skin, lighter periods, and of course, no pregnancies). But what’s actually going on in your body when you take it?
You may be wondering if birth control stops you from ovulating and what this means for your long-term fertility. It can be especially confusing if you think you might be getting the telltale signs of ovulation each month. So let’s look at the science and find out once and for all how birth control impacts ovulation.
Key takeaways
- The hormones in birth control can stop your brain from telling your ovaries to develop and release an egg each month (ovulation). When this happens, it means you don’t ovulate.
- Not ovulating on birth control is perfectly safe and will not impact your fertility. For most types of hormonal birth control, your fertility will return just a cycle or two after stopping.
- Some types of hormonal birth control contain the hormones estrogen and progestin, while others contain only progestin. While progestin alone stops ovulation, it doesn’t always do so every cycle. This means some people find they do ovulate while on progestin-only birth control.
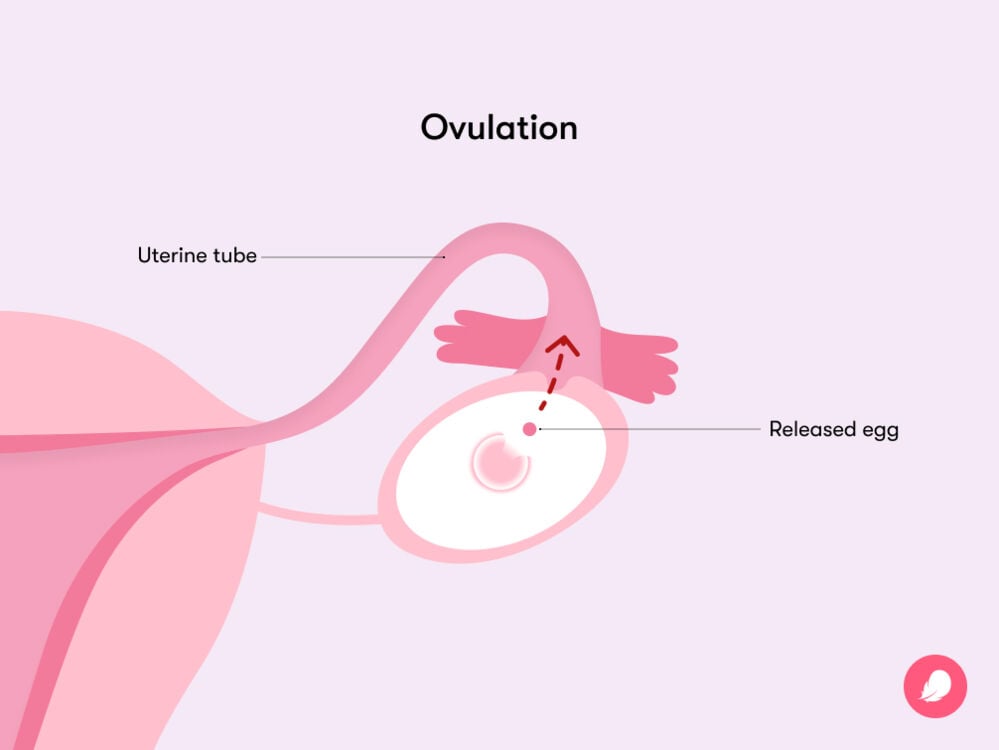
Does birth control stop ovulation?
Ready for a quick science lesson? Over to Flo expert Dr. Jennifer Boyle, obstetrician and gynecologist, Massachusetts General Hospital, Massachusetts, US “The medications in hormonal birth control are synthetic forms of the hormones estrogen and progesterone, which suppress what we call the ‘reproductive axis,’” she says.
The female reproductive axis is the hypothalamus, pituitary gland, and ovaries. You need all three parts to work together for ovulation to happen.
“It starts in the hypothalamus, a small structure in the brain that produces hormones that act on the pituitary, a gland in the brain,” explains Dr. Boyle. “The pituitary gland then produces and releases hormones that make the ovaries produce and release hormones and ovulate.”
She adds, “Taking hormonal birth control, especially one that contains both estrogen and progestin, will make the reproductive axis take a break, so to speak. The ovaries then don’t receive a signal to develop an egg for ovulation.”
You’re probably wondering whether this applies to the type of contraception you’re taking. Well, the following methods all prevent ovulation in this way, as they each contain estrogen and progestin or progestin-only:
- Implant
- Hormonal intrauterine device (IUD)
- Injection
- Pill
- Vaginal ring
- Patch
Does your body stop making eggs on birth control?
Actually, the idea that your body makes eggs each month is a myth. Dr. Boyle explains, “Fun fact: People who have ovaries have the maximum number of eggs that they will ever have before they are even born. Our ovaries don’t ever make more eggs. While using most hormonal birth control methods, eggs will not be developed or released as would happen in a natural cycle.”
So hormonal contraception stops your ovaries from developing your existing eggs, rather than making them in the first place.
You may be wondering whether this means being on birth control saves your eggs, allowing you to keep them for any potential future pregnancies. But this idea is another myth. “Our eggs continue to age and break down whether they mature and are released by the ovaries (ovulation) or not,” says Dr. Boyle.
“So, unfortunately, being on birth control that prevents ovulation doesn’t protect or save your eggs for the future. However, birth control that prevents ovulation helps lower the risk of ovarian cancer and can prevent some types of ovarian cysts from forming. These benefits can protect your ovaries and the eggs they contain, just in a more indirect way than the myth suggests.”
What happens if someone doesn’t ovulate?
If contraception like the pill works for you, you may have been on it for a long time. In fact, some types of hormonal IUDs are designed to be left in place for up to eight years. Is it really safe to suppress ovulation for this long?
“Not ovulating because of your birth control method (or because you are breastfeeding or pregnant) is not at all dangerous to your health and will not impact your fertility,” says Dr. Boyle. “In fact, the breaks from ovulation that birth control methods and breastfeeding provide lower your risk of ovarian cancer.”
When you stop taking birth control, your normal level of fertility should return after just a cycle or two. The only exception is with the birth control shot, which takes several months to clear from your body. How long it takes to get pregnant will vary from person to person, but most people find they are able to get pregnant within 10 months of their last injection.
Why you might have ovulation symptoms while on birth control pills
The kinds of ovulation symptoms you might experience on the pill depend on which type of pill you’re on. Combined birth control pills contain both estrogen and progestin, while the progestin-only pill contains only — you guessed it — progestin (the synthetic form of progesterone).
The side effects of the combined pill can mimic one of the key ovulation symptoms, as Dr. Boyle explains. “While taking the combined pill, sometimes the follicles (sacs of fluid where an egg lives) in your ovaries can develop,” she says. “This can stretch the covering of the ovary and cause a feeling of pressure or pain. Usually, however, the egg isn’t fully released, and ovulation does not occur.”
This pressure or pain might feel a bit like ovulation cramps, which are thought to be caused by the follicle stretching and rupturing when you release an egg.
“It is very different with the progestin-only pill, however,” adds Dr. Boyle. “Also known as the mini pill, the progestin-only pill does not contain estrogen.” Acting alone, progestin can stop ovulation, but it may not stop it consistently.
Take a quiz
Find out what you can do with our Health Assistant
About 40% of people who take the mini pill will continue to ovulate. “For these people, they have ovulation symptoms because they are ovulating,” says Dr. Boyle.
Ovulation symptoms can include tender breasts, changes in vaginal discharge (it may become clear and slippery, like raw egg whites), light cramping, spotting, and a heightened sex drive. If you notice any of these signs, logging the changes in the Flo cycle-tracking app can help you get to know your body better.
But don’t worry — none of this makes the mini pill any less effective. In fact, the typical-use failure rate for the mini pill is the same as for the combined pill, at 7% (meaning 7 in 100 couples would get pregnant anyway after a year of use). That’s because even if you do ovulate on the mini pill, you are still protected from pregnancy. “The good news is, the extra progestin makes the cervical mucus thicken up, and this makes the sperm unable to pass through the cervix and reach the egg,” says Dr. Boyle.
Progestin also thins the lining of your uterus. This means that even if an egg did get fertilized by a sperm, implantation (when a fertilized egg implants in your uterus to become an embryo) wouldn’t be possible.
For the same reasons as for the mini pill, it’s possible to ovulate on other types of progestin-only hormonal birth control, including the injection, hormonal IUD, and implant. But just like the mini pill, these methods also prevent pregnancy through thickening cervical mucus and thinning the uterine lining.
More FAQs
Do you still have a period while on birth control pills?
“Not really,” says Dr. Boyle. “It’s important to understand that the bleeding that you have while taking combined birth control pills is not a real menstrual period.
“You have not had the increase and decrease in estrogen and progesterone, the endometrial lining has not grown and then shed, and you have not ovulated as you would in a true menstrual cycle. The bleeding you have is what we call a withdrawal bleed. You pause the active pills of the birth control pack, and this drop in hormones causes the lining of the uterus to bleed and shed.”
Does birth control stop ovulation right away?
This all depends on the type of birth control and where you are in your cycle when you start taking it. For example, with combined birth control pills, you’ll be protected from pregnancy right away if you start taking it on the first day of your period. Otherwise, you’ll need to use backup protection for seven days.
For the mini pill, you’ll be protected immediately if you start taking it within five days of the start of your period. Otherwise, you’ll need to use backup protection for two days. You should always check with your doctor how quickly the type of birth control you’re taking becomes effective.
Can birth control stop suppressing ovulation?
It’s possible for any kind of birth control method to fail, even when you are using it perfectly. However, perfect-use failure rates for hormonal contraception are low.
For example, the combined pill’s perfect-use failure rate is just 0.3%, meaning fewer than 1 in every 100 people would get pregnant anyway after a year of use. Due to human error, the typical-use failure rate for hormonal contraceptives can be slightly higher. For example, the combined pill’s typical-use failure rate is 7%. This is because you might forget to take it or take it at the wrong time.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Anti-Müllerian Hormone Test.” MedlinePlus, 6 Mar. 2023, medlineplus.gov/lab-tests/anti-mullerian-hormone-test/.
Babic, Ana, et al. “Association between Breastfeeding and Ovarian Cancer Risk.” JAMA Oncology, vol. 6, no. 6, June 2020, https://10.1001/jamaoncol.2020.0421.
“Birth Control Options.” Cleveland Clinic, my.clevelandclinic.org/health/articles/11427-birth-control-options. Accessed 10 May 2024.
Charlewood, G. P. “Mittelschmerz or Ovulation Pain.” Suid-Afrikaanse Tydskrif vir Geneeskunde [South African Medical Journal], vol. 32, no. 10, Mar. 1958, pp. 261–62.
“Contraception.” Centers for Disease Control and Prevention, www.cdc.gov/reproductivehealth/contraception/index.htm. Accessed 10 May 2024.
“Contraception: Hormonal Contraceptives.” InformedHealth.org. Institute for Quality and Efficiency in Health Care (IQWiG), 2006, www.ncbi.nlm.nih.gov/books/NBK441576/.
“Delaying Your Period with Hormonal Birth Control.” Mayo Clinic, 2 Dec. 2022, www.mayoclinic.org/healthy-lifestyle/birth-control/in-depth/womens-health/art-20044044.
Family Planning: A Global Handbook for Providers, 2022 Edition. World Health Organization, 14 Nov. 2022, www.who.int/publications/i/item/9780999203705.
Hariton, Eduardo, et al. “Anti-Müllerian Hormone Levels among Contraceptive Users: Evidence from a Cross-Sectional Cohort of 27,125 Individuals.” American Journal of Obstetrics and Gynecology, vol. 225, no. 5, Nov. 2021, pp. 515.e1–10, https://doi.org/10.1016/j.ajog.2021.06.052.
“Hormonal IUD (Mirena).” Mayo Clinic, 11 Apr. 2024, www.mayoclinic.org/tests-procedures/mirena/about/pac-20391354.
Kaunitz, Andrew M. “Patient Education: Hormonal Methods of Birth Control (Beyond the Basics).” UpToDate, 18 Mar. 2024, www.uptodate.com/contents/hormonal-methods-of-birth-control-beyond-the-basics.
McLaughlin, Jessica E. “Female Reproductive Endocrinology.” MSD Manual Professional Edition, Apr. 2022, www.msdmanuals.com/professional/gynecology-and-obstetrics/female-reproductive-endocrinology/female-reproductive-endocrinology.
“Minipill (Progestin-Only Birth Control Pill).” Mayo Clinic, 13 Jan. 2023, www.mayoclinic.org/tests-procedures/minipill/about/pac-20388306.
“Ovarian Cancer.” Mayo Clinic, 9 May 2023, www.mayoclinic.org/diseases-conditions/ovarian-cancer/symptoms-causes/syc-20375941.
“Ovulation.” Cleveland Clinic, my.clevelandclinic.org/health/articles/23439-ovulation. Accessed 10 May 2024.
“Progestin-Only Hormonal Birth Control: Pill and Injection.” The American College of Obstetricians and Gynecologists, Jan. 2023, www.acog.org/womens-health/faqs/progestin-only-hormonal-birth-control-pill-and-injection.
Wallace, W. Hamish B., and Thomas W. Kelsey. “Human Ovarian Reserve from Conception to the Menopause.” PLOS ONE, vol. 5, no. 1, Jan. 2010, https://doi.org/10.1371/journal.pone.0008772.




