Many people choose to use long-acting reversible contraception (LARC) to prevent pregnancy. Not only are these methods highly effective over a long period of time, but they require little to no effort on your part. So, is LARC right for you? Below, learn about the various types of long-acting reversible contraception methods, who can use them, and their potential side effects to figure out if it could be a good fit for your body and lifestyle.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
LARC: Long-Acting Reversible Contraception Types, Benefits, and Side Effects


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
What is LARC?
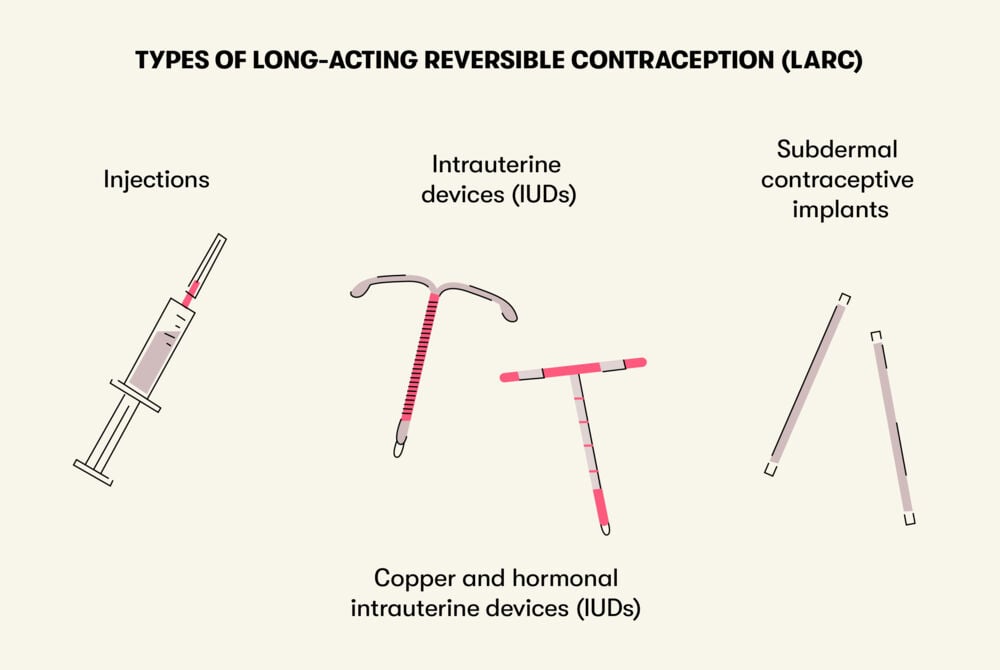
Do you have trouble remembering to take your birth control pill, or are you interested in trying a different form of contraception? Long-acting reversible contraception, or LARC, could be a good option for you. It can prevent pregnancy for months or even years. There are a few different types of long-acting reversible contraceptives that range in how long they last, including:
- Contraceptive injections given every 12 weeks
- Intrauterine device (IUD) placed inside the uterus: copper (non-hormonal) and hormonal options last for 5–10 years depending on the type
- A subdermal contraceptive implant placed under the skin in your arm that lasts for three years
LARC vs. other types of contraception
"Many studies have shown that the most effective [forms of contraception] are long-acting methods, namely IUDs and hormonal implants," according to Professor Johannes Bitzer in his Flo interview on contraception. In fact, fewer than 1 in 100 women who use LARC get pregnant. In comparison, around 9 in 100 who take birth control pills and 18 in 100 people who use male condoms for contraception get pregnant within one year.
The major advantages of LARC over other types of contraception are that they don’t require an ongoing effort, and they prevent pregnancy for a long period of time. Unlike the pill, which you have to remember to take every day around the same time, you don’t have to do anything to make sure LARC works. Once it’s in, you’re protected.
Additionally, you can get pregnant almost immediately after having a LARC device (IUD or implant) removed. As for injections, fertility tends to come back within 9–10 months after the last shot, but it returns within four months for some people.
LARCs are also estrogen-free and are suitable for people who can’t tolerate contraception that contains estrogen.
Finally, LARCs don’t interfere with sex, and no one can see that you’re using it.
However, it’s important to note that LARC doesn’t offer protection from sexually transmitted infections (STIs). No matter what type of LARC you choose, a condom is always a good idea and the only way to prevent the spread of STIs (other than abstinence).
Let’s take a closer look at the different options for long-acting contraceptive methods.
Types of long-acting reversible contraception
Take a quiz
Find out what you can do with our Health Assistant
Injection
The contraceptive injection is a long-acting progestin-only contraceptive that contains depo-medroxyprogesterone acetate (DMPA) that’s given as an injection every three months (12 weeks). It prevents pregnancy by stopping ovulation and thickening the cervical mucus.
This type of reversible contraception is safe and effective for people who are breastfeeding. Providers sometimes recommend the injection to manage certain health conditions like anemia, seizures, endometriosis, and uterine fibroids. The injection can also decrease menstrual pain and lower the risk of endometrial cancer.
The potential side effects of the injection include:
- Longer periods and spotting between periods
- Skipped periods or decreased bleeding
- Weight gain
- Mood changes
- Loss of interest in sex
If you have a history of depression, heart attack, stroke, breast cancer, or liver disease, your health care provider may discourage using this method of birth control.
Intrauterine device (IUD)
The IUD is a small device that’s placed in the uterus to prevent pregnancy.
There are two types of intrauterine devices (IUD):
- Copper IUD
- Hormonal IUD
The IUD is safe for most people and can be used regardless of whether or not you’ve given birth. To insert the IUD, a provider inserts a speculum into the vagina and places the IUD into the uterus via the cervix. If you get an IUD, you may be offered some medicine to help open or numb your cervix beforehand. You may feel some cramping or pain during the insertion. People who haven’t given birth may find the process more painful than those who have. After insertion, you could have some cramping or back pain, so take it easy at home and have a heating pad and some pain medication handy.
These are some common IUD side effects:
- Cramping and spotting during the first few months after IUD insertion
- Increased risk of infection
- IUD may slip out of place, especially during a period, which can lead to pregnancy
- Pregnancy complications in case you get pregnant with the IUD in place (which is extremely rare)
Using a menstrual cup with an IUD is linked to a higher rate of IUD expulsion, which is when the IUD comes out or moves from where it's supposed to be. If this happens, you'll need to see a health care provider right away and note that the IUD may no longer be effective.
The Copper IUD
The copper IUD is a type of long-active reversible contraception that has a T-shaped polyethylene frame with copper wire wrapping around the stem and arms. It’s ideal for people who prefer a hormone-free method of birth control.
The copper IUD prevents pregnancy by stopping sperm from reaching an egg. It also alters the lining of the uterus, making it difficult for a fertilized egg to implant in the uterine wall. This reversible contraception can remain in place for up to 10 years and be removed at any time (by a medical professional).
Additionally, it’s safe to be used while breastfeeding and can act as emergency contraception if inserted within five days of having unprotected sex.
However, the copper IUD is not recommended for some people. If you have any of the following conditions, it might not be for you:
- If you might be pregnant
- Pelvic inflammatory disease (PID)
- Cervicitis
- Abnormal bleeding from the vagina
- Cancer of the genital tract
- Chlamydia
- Gonorrhea
- Pelvic tuberculosis
- Allergies to any component of the IUD
- Uterine abnormalities (such as large fibroids)
Possible side effects of the copper IUD include:
- Bleeding between periods
- Strong cramps
- Heavy bleeding
So, if you already have particularly heavy or painful periods, you may want to think about using a different type of IUD or LARC.
The hormonal IUD
The levonorgestrel-releasing IUD has a T-shaped polyethylene frame and releases levonorgestrel, a hormone similar to progesterone. This IUD prevents pregnancy by thickening the cervical mucus, restricting sperm movement, and stopping ovulation.
The hormonal IUD is not recommended for people who have:
- Breast malignancy (or other cancer sensitive to progestin)
- Liver tumors and disease
Side effects of the hormonal IUD can include:
- Headache
- Acne
- Breast tenderness
- Cramping or pelvic pain
- Irregular bleeding (during first six months)
- Mood swings
- Ovarian cysts
If you have very heavy periods or severe menstrual pain, a hormonal IUD might help reduce bleeding and cramping.
Contraceptive implants
The contraceptive implant is another long-acting reversible contraception method. It’s a 1.6-inch (four-centimeter) rod, about the size of a match, that releases about 68 micrograms of etonogestrel (a progestin) every day.
To use the implant, a health care provider inserts a rod into the outer layer of skin in your upper arm. They will give you local anesthesia so you don’t feel anything during the insertion. Some people experience soreness and bruising where the implant was inserted, but it goes away quickly. Once it’s in, the rod slowly releases hormones to prevent pregnancy.
The hormones released in this LARCs birth control method decrease the lining of the uterus and suppress ovulation. They may also thicken the cervical mucus, which can prevent sperm from entering the uterus altogether.
The advantages of using a subdermal contraceptive implant as a long-acting reversible contraception method are that it is highly effective and easy to use. Just like the IUD, once inserted, you don’t have to think too much about it.
However, people with the following conditions should not use this LARC method:
- If you might be pregnant
- Breast cancer
- Liver disease
- Undiagnosed abnormal uterine bleeding
- Allergy to any component of the implant
If you are overweight with a BMI over 30, the implant may be less effective. Certain medications and herbal products may also decrease the effectiveness of the implant.
The subdermal implant can also have some side effects, such as:
- Irregular bleeding
- Weight gain
- Mood changes
- Headaches
After three years, the implant will need to be replaced to continue preventing pregnancy. For this and all other methods of LARC, be sure to note the date you got it and set a reminder to visit your health care provider to get a new one or have it removed.
Summing Up
Long-acting reversible contraceptives are highly effective ways to prevent pregnancy over a long period of time. A major plus of LARCs is that they don’t require ongoing effort to be effective. Plus, once you stop using them, fertility usually returns fairly quickly. While each type of LARC (injection, IUD, and implant) has its own risk of side effects and limitations on who can get it, many people use them without any issues.
If you’re interested in using a long-acting reversible contraceptive, talk to a health care provider to figure out which one is best for you.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.




