You may not have heard of a molar pregnancy unless it’s happened to you, and it can be a difficult thing to understand. With the help of a Flo expert, here’s what you should know about the pregnancy complication.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Molar pregnancy: What it is and how it feels


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Experiencing any kind of pregnancy that doesn’t work out can be extremely hard for anyone. But when it’s the result of a rare, sometimes unheard-of condition, it can feel even more isolating.
Molar pregnancy occurs in around 1 in 1,000 pregnancies. And while they are rare, molar pregnancies can happen to anyone, and there is nothing you can do to avoid them, so you should try not to blame yourself if it happens to you.
Some of the symptoms of molar pregnancy are easily confused with other, intense pregnancy symptoms. To help you understand the difference, we spoke to Dr. Gian Carlo Di Renzo, chair of the department of obstetrics and gynecology, University of Perugia, Italy. With his help, we explain what a molar pregnancy is, what the signs are, and what to do if you experience one.
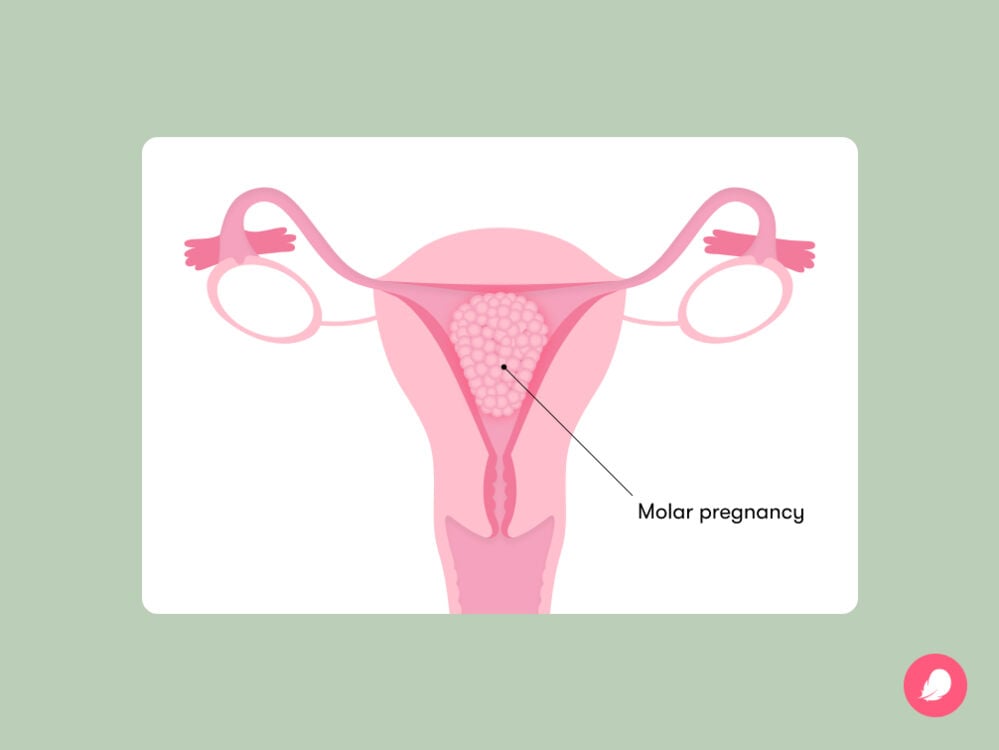
What is a molar pregnancy?
A molar pregnancy — known more scientifically as a “hydatidiform mole” — is when fertilization doesn’t quite work the way it’s supposed to. This condition causes tissue to grow in the uterus that you wouldn’t usually find there, called “trophoblastic tissue.” If left untreated, these growths can cause health problems.
In a healthy pregnancy, a sperm fertilizes an egg. Each brings 23 chromosomes, containing all sorts of genetic material that determines lots of factors, from the color of our hair to the sound of our voice. But in a molar pregnancy, there’s an error in the process, which results in an imbalance of these chromosomes. There are two types of molar pregnancy: complete and partial.
Complete molar pregnancy
“A complete mole is when there is an egg with chromosomes that don’t work or an egg without any chromosomes in it — it’s empty,” Dr. Di Renzo says. That means that when it’s fertilized (either by one sperm or sometimes two at the same time), it contains only the sperm’s chromosomes. As a healthy pregnancy needs chromosomes from both the sperm and egg, a fetus can’t be created in this situation. But the tissue that forms the placenta still grows because your body still thinks it’s pregnant. The excess tissue can also continue to grow, developing into a noncancerous tumor in the uterus.
A complete mole is considered riskier for your health than a partial mole, “because it grows very quickly,” Dr. Di Renzo says. It also means that your pregnancy symptoms would advance more quickly than expected. “At eight weeks, you might feel as pregnant as you would at 16 weeks, because your uterus is growing so fast. Sometimes, you can think you have twins or multiple pregnancies because of the rate of the growth, but the ultrasound will show there is no fetus,” he explains.
Partial molar pregnancy
A partial molar pregnancy is slightly more complex. This is when the egg’s chromosomes are there, but two sperm fertilize an egg at the same time, so there are two sets of chromosomes from the sperm. This scenario can lead to early signs of a fetus, but unfortunately, it can’t develop into a healthy baby.
“A partial molar pregnancy isn’t quite as dangerous as a complete mole, but it can go unnoticed for longer,” Dr. Di Renzo says. This is because a person might bleed, which is a symptom of molar pregnancy (more on that below), and assume they have had a miscarriage. Based on this assumption, they might not go to their health care provider for tests, meaning the remaining molar tissue in the uterus isn’t discovered as quickly.
Learning that your pregnancy is molar and won’t result in a baby can be understandably hard, especially as you will likely have experienced many of the usual symptoms of a healthy pregnancy and may not have been aware there was anything wrong. Scroll down for advice on how to cope if you find yourself in this difficult situation.
Molar pregnancy symptoms
Symptoms are very similar in both partial and complete molar pregnancies; however, pregnancy symptoms are often more intense with a complete mole. Below, we share some of the most common signs of molar pregnancy to look out for. If you notice these or anything else that’s concerning or unusual during the first few weeks and months of your pregnancy, reach out to your health care provider for advice.
Intense nausea and vomiting
It’s common to experience nausea and vomiting as part of your pregnancy journey. However, in molar pregnancies, your hormone levels are much higher than normal (more on that below), making these symptoms very intense.
Dark brown discharge or bleeding from your vagina during first trimester
Bleeding in the first few months of pregnancy doesn’t always mean there’s a problem, but it’s always worth calling a health care professional if it happens. A common molar pregnancy symptom is bleeding that’s bright red or dark brown discharge, which can sometimes convince patients that they’ve had a miscarriage.
High hCG hormone levels
In a healthy pregnancy, you will start producing a hormone called human chorionic gonadotropin (hCG) around 10 days after conception. This is what causes other pregnancy symptoms like nausea and vomiting.
“But in a molar pregnancy, [hCG levels] are unnaturally high,” explains Dr. Di Renzo. This is because molar tissue in the uterus triggers the release of hCG. However, the only way you’ll be able to find out your exact hCG levels is by doing a blood test, so speak to your health care provider if you’re at all concerned about the severity of the pregnancy symptoms you are experiencing.
Other unusual feelings
As is the general rule with pregnancy, you should speak to a doctor whenever you experience anything that doesn’t feel right for you. In molar pregnancies, this could include high blood pressure, cysts that look like grapes in the vaginal area, and pelvic pain, so keep an eye out.
How is molar pregnancy diagnosed and treated?
If you have a molar pregnancy, this will be spotted at your first ultrasound scan. “Specialists can usually diagnose a molar pregnancy after an ultrasound, because there will be no embryo (or a very small one), ovarian cysts, or an unusual placenta,” Dr. Di Renzo says.
“If the health professional suspects a molar pregnancy, they might recommend blood tests to measure your hormone (hCG) levels,” Dr. Di Renzo adds.
Once it’s been diagnosed, your doctor will arrange for you to have the tissue from the molar pregnancy removed from your uterus. This is a short procedure that will often be done under general anesthesia, meaning you won’t feel any pain. The tissue is cleared, often using ultrasound guidance, by opening up your cervix with dilators and using a suction device to gently remove the abnormal tissue from the uterus.
“After you’ve had the tissue cleared, it’s important to continue monitoring so that we’re sure everything has been removed,” Dr. Di Renzo says. “The easiest way to do this is to continue urine tests every week or fortnight to measure hormone levels.” And when is it safe to consider trying to conceive again? “If you wait until everything is back to normal, which can be as soon as two months, you can start trying for another baby,” Dr. Di Renzo says.
Finding out you have a molar pregnancy can be extremely distressing, particularly because the symptoms of molar pregnancy are so similar to those of a healthy pregnancy. If you’ve experienced this kind of pregnancy complication and have felt grief, isolation, or guilt afterward, know that these feelings are totally normal. Allow yourself to work through them. Remember that molar pregnancy can happen to anyone and that you’re not alone. If it could be helpful, reach out to organizations like March of Dimes in the United States and the Miscarriage Association in the United Kingdom for support.
Molar pregnancy complications and risk factors
It’s important to remember that molar pregnancies are rare, “so anyone trying to get pregnant shouldn’t worry too much about this,” Dr. Di Renzo says. While some patterns have been identified by research, a molar pregnancy can happen to anyone, and it’s not caused by anything anyone does wrong. (10)
“Molar pregnancy tends to be more common among adolescents or among women over 40,” Dr. Di Renzo says. “Some populations appear to have more molar pregnancies than others,” he adds. It’s not exactly clear why this may be, however, because there’s very little research on it. Other factors that may slightly elevate your risk are having two or more miscarriages or a previous history of molar pregnancies (although try not to worry — this only raises your risk very slightly, by 1% to 2%).
There are a few very uncommon complications with molar pregnancies. One of these is called “choriocarcinoma,” which occurs when parts of the tissue created in molar pregnancy remain in the body after the end of the pregnancy. In very rare cases, the remaining molar tissue can spread to other parts of the body and may become cancerous. But remember, this really is incredibly unlikely. It only happens in around 1 in 50,000 pregnancies, and it’s very treatable. If you do experience choriocarcinoma and have chemotherapy, the positive news is that there’s an 80% chance you will go on to have a healthy pregnancy.
One other possible complication with molar pregnancy is a “twin molar pregnancy,” which can make treatment more complex. This is “when there is a healthy embryo in the uterus along with a partial or complete mole,” explains Dr. Di Renzo. “It can impair the growth of the other fetus, but that doesn’t mean the healthy fetus won’t survive,” he adds.
Again, this situation is rare, only happening in around 1 in 100,000 pregnancies. (16) “It can lead to complications, but there is around a 60% survival rate for the healthy fetus,” notes Dr. Di Renzo.
How does it feel to experience a molar pregnancy?
It’s one thing understanding the physical side of what happens in a molar pregnancy, but there’s also the emotional impact it can have. Jayde, 36, from Warrington, UK, experienced a molar pregnancy in June 2020 during the height of the coronavirus pandemic. She already had two children, Charlie and Theia, and had previously experienced endometriosis, polycystic ovaries, and multiple miscarriages.
“When I got to eight or nine weeks, the hospital called to book me an appointment for a scan,” Jayde tells Flo. “Everything felt normal. I was hormonal and feeling [nauseous], which was just like a normal pregnancy. The only difference was that I was sicker than I had been with my previous two children. I had headaches and some pain down my right side.”
Jayde shared this with her health care provider, and partly due to her medical history, she was sent for an earlier scan to make sure everything was OK. When the scan arrived, Jayde received the devastating news that she’d had another miscarriage.
“Every miscarriage is a shock, but this one was even more difficult to take in because I had all the symptoms of pregnancy,” Jayde recalls.
Further investigations, including blood tests and another scan, revealed her hormone levels were unusually high, and Jayde was referred to a specialist center. After being diagnosed with a complete molar pregnancy, Jayde had surgery to remove the molar tissue from her uterus.
“I felt hugely impacted by the molar pregnancy experience,” Jayde says. “I felt angry that it had happened to me, especially when I saw friends and family members around me having healthy pregnancies.
“Every miscarriage is a shock, but this one was even more difficult to take in because I had all the symptoms of pregnancy”
“It’s a very difficult thing for people to relate to, so they just couldn’t understand. It feels like a grieving process when you have an unsuccessful pregnancy.”
Following her aftercare, which involved checks to ensure all the molar tissue had been removed from her uterus and urine tests every two weeks, Jayde got the good news that her hormone levels had returned to normal. Four months after her surgery, she became pregnant again.
Despite feeling understandably anxious throughout the next pregnancy, Jayde went on to give birth to a healthy baby boy named Bodhi. “He felt like a little miracle,” she says. “I always call him my little heart-healer, because that’s what it felt like at the time.”
Blighted ovum vs. molar pregnancy
If you’re reading this and wondering what the difference is between a molar pregnancy and a blighted ovum (also known as an anembryonic pregnancy), it’s a good question. The symptoms can be quite similar, after all.
A blighted ovum is when a normally fertilized egg attaches itself to the uterus, but the embryo never develops or stops developing. It means you might have a positive pregnancy test, but the symptoms will quickly subside.
A molar pregnancy, as we now know, happens when there are issues with fertilization to begin with, creating abnormal growths, which can make the two conditions appear similar at first. Sadly, neither pregnancy complication can result in a viable pregnancy, which can cause understandable heartache.
Getting pregnant after a molar pregnancy
Going through a molar pregnancy can be extremely challenging and emotional. Those feelings must be worked through, but the positive news is that there’s every chance you can go on to have a healthy pregnancy afterward. In fact, the risk of a molar pregnancy happening again is low. For 99 out of 100 women, their next pregnancy will not be a molar pregnancy. (14)
Jayde’s story is an example of this, so keep hope. Just remember that you should wait until all the molar pregnancy tissue has gone from your uterus before trying again.
Molar pregnancy: The takeaway
Molar pregnancy is a complex and rare condition, but hopefully this article has helped you to understand it further. Despite its rarity, there are people all around the world who have experienced it, and there are specialists in place to help you through it.
“My advice to someone going through a molar pregnancy is to ask questions and listen to your gut instinct,” Jayde says. “Don’t be afraid to go to your appointments armed with questions and keep yourself informed.
“Most of all, don’t lose hope. Like me, you’re likely to go on to have a wonderful, healthy pregnancy.”


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Bitzer, Johannes. “Blighted Ovum: Symptoms, Causes, and Where to Find Support.” Flo Health, 9 Feb. 2019, flo.health/pregnancy/pregnancy-health/complications/blighted-ovum.
“Genetics Basics.” Centers for Disease Control and Prevention, 13 Sep. 2022, www.cdc.gov/genomics/about/basics.htm.
Ghassemzadeh, Sassan, et al. “Hydatidiform Mole.” StatPearls, StatPearls Publishing, 2022.
“Molar Pregnancy: Symptoms, Risks & Treatment.” American Pregnancy Association, 27 Apr. 2012, americanpregnancy.org/healthy-pregnancy/birth-defects/molar-pregnancy/.
“Molar Pregnancy.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/17889-molar-pregnancy. Accessed 13 Jan. 2023.
“Molar Pregnancy.” Mayo Clinic, 12 Nov. 2022, www.mayoclinic.org/diseases-conditions/molar-pregnancy/symptoms-causes/syc-20375175.
“Molar Pregnancy.” NHS, www.nhs.uk/conditions/molar-pregnancy/. Accessed 13 Jan. 2023.
“Molar Pregnancy and Gestational Trophoblastic Disease.” Royal College of Obstetricians & Gynaecologists, www.rcog.org.uk/for-the-public/browse-all-patient-information-leaflets/molar-pregnancy-and-gestational-trophoblastic-disease/. Accessed 13 Jan. 2023.
“Persistent Trophoblastic Disease and Choriocarcinoma.” NHS, www.nhs.uk/conditions/persistent-trophoblastic-disease-choriocarcinoma/. Accessed 13 Jan. 2023.
“Pregnancy Test: When To Take, Types & Accuracy.” Cleveland Clinic, my.clevelandclinic.org/health/articles/9703-pregnancy-tests. Accessed 13 Jan. 2023.
“Symptoms of Persistent Trophoblastic Disease and Choriocarcinoma.” Cancer Research UK, www.cancerresearchuk.org/about-cancer/gestational-trophoblastic-disease-gtd/persistent-trophoblastic-disease-ptd-choriocarcinoma/symptoms. Accessed 13 Jan. 2023.
“Vaginal Bleeding.” NHS, www.nhs.uk/pregnancy/related-conditions/common-symptoms/vaginal-bleeding/. Accessed 13 Jan. 2023.
Zilberman Sharon, N., et al. “Obstetric Outcomes of Twin Pregnancies Presenting with a Complete Hydatidiform Mole and Coexistent Normal Fetus: A Systematic Review and Meta-Analysis.” BJOG, vol. 127, no. 12, Nov. 2020, pp. 1450–57.

