Pregnancy can be an understandably worrying time, so it’s common to wonder about the causes and risks of miscarriage. Here, we speak to a doctor for answers — and reassurance.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Miscarriage: Causes and risks to know about


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Pregnancy can be an anxious time, and it’s natural to worry about miscarriage. While there are causes and risks to consider, it’s important to note that most miscarriages happen for reasons that are completely out of your control, so remember that it’s not your fault if this happens. And thankfully, for the vast majority of people affected, loss of pregnancy is usually a one-off occurrence.
Miscarriage affects around 10% to 25% of known pregnancies — but they often occur very early on, before you even realize you’re pregnant. Symptoms of pregnancy loss include vaginal bleeding or loss of fluids, tissue, or clots from the vagina. Cramping or pain in the abdomen or lower back is also a known symptom. However, remember that spotting and cramping are both also common early signs of pregnancy; while experiencing them can be unnerving, it doesn’t necessarily mean you will miscarry. Some miscarriages can occur without any symptoms, but try not to let this thought run away with you. If you’re concerned, always reach out to your doctor, and they can provide reassurance and advice.
Read on to discover more about what can cause miscarriage and, hopefully, find a little bit of reassurance during this time.

If you or someone you know is going through a difficult time, remember that there are ways to get help. Here are some support services and resources in your country.
Find out moreCauses of miscarriage during pregnancy
First of all, let’s get one thing clear: “There is nothing you can do to prevent or cause a miscarriage,” says Dr. Allison Rodgers, obstetrician and gynecologist, Fertility Centers of Illinois, US. However, it can be helpful to understand what can cause miscarriages and which things to try to avoid during pregnancy, as there are some lifestyle tweaks you can make to help mitigate some of the risks.
Chromosome abnormalities
Approximately 50% of all miscarriages occur because of chromosomal abnormalities — such as having too many or too few chromosomes — which can unfortunately prevent the embryo from developing properly. That might sound confusing if it’s been a while since you studied biology, so let’s break it down a bit. Chromosomes from the sperm and the egg carry the genes an embryo needs to develop into a baby — half from each of the two biological parents. Problems with those chromosomes usually happen by chance during the complex process of cell division (the very first stages of pregnancy), and this can unfortunately lead to a miscarriage a little later down the line.
Physical problems
“Other causes for losses are physical problems,” Dr. Rodgers explains. But what exactly are physical problems? Essentially, there may be problems with the placenta (the organ that grows alongside the baby to provide it with oxygen and nutrients), the uterus (sometimes known as the womb, where the fetus grows), or the cervix (the donut-shaped organ between the uterus and the vagina) — such as an abnormally shaped uterus — or problems with the sperm.
Miscarriage risk factors
Frustratingly, it isn’t always possible to identify the cause, or causes, of miscarriage. However, we do know there are factors that can unfortunately put you at a slightly increased risk of experiencing a miscarriage.
Age
One risk factor for a miscarriage is advanced maternal age. “The risk increases as we get older, so, by the time we are 40, our chances of miscarriage are 40%,” Dr. Rodgers explains. The risk of miscarriage also increases as the father gets older, although this has less impact than the age of the mother.
These statistics might sound frightening, but they certainly don’t mean that people over the age of 40 can’t have positive pregnancy outcomes. Recent data shows that birth rates in the US have declined for nearly all age groups of women under 35 but have actually risen for women in their late 30s and early 40s. So if you’re older and you’re trying to conceive, you have every reason to keep hope.
Long-term health conditions
Unfortunately, some chronic diseases and long-term health issues can also increase the risk of miscarriage.
These include:
- Diabetes that is not well controlled: If you live with either Type 1 or Type 2 diabetes, getting your blood glucose levels under control before pregnancy can be a good way to mitigate this risk. If you have any concerns or questions about your treatment or medication, seek medical advice (ideally before you start trying to conceive).
- Some autoimmune diseases
- Hormonal conditions like thyroid disease or polycystic ovary syndrome (PCOS): People with PCOS are three times as likely to miscarry as those without, but there is hope on the horizon; researchers are currently studying whether taking metformin (a diabetes medication) could reduce this risk.
- High blood pressure (also referred to as hypertension)
- Kidney disease
Remember that although they can increase the risk, living with any of these conditions does not mean that you will have a miscarriage — far from it. If you have any concerns, speak to your health care provider for advice on managing your condition and your overall well-being during pregnancy.
Infections
We’re always encountering viruses and bacteria in our normal lives, so it’s difficult to avoid infections completely. However, some infections could also affect your baby and, in some rare scenarios, may potentially lead to a miscarriage. But it’s important to remember that many of these infections can be easily treated or managed — or, in the case of listeriosis and toxoplasmosis, avoided by not eating high-risk foods, such as raw or undercooked meat and eggs and unpasteurized cheeses.
When it comes to infections, some risk factors include:
- Rubella
- Herpes simplex virus
- Toxoplasmosis
- Chickenpox
- HIV
- Syphilis
- Parvovirus B19
- Cytomegalovirus
If you’re concerned about any of these or other infections or want more information, it’s best to speak to your doctor, who will be happy to help.
Weight issues
Being over or underweight (that means having a Body Mass Index (BMI) below 20 or over 25) may increase your risk of a miscarriage, while being obese (having a BMI over 30) can further increase that risk. If you’re concerned about your weight, speak to your health care provider for advice on healthy eating and exercise during pregnancy.
Smoking
There is evidence that smoking is associated with an increased risk of miscarriage, as well as other adverse pregnancy outcomes. There isn’t currently enough research to determine whether vaping poses a similar risk, but experts recommend avoiding e-cigarettes during pregnancy. Although overcoming a nicotine addiction can be understandably difficult, support is available if you want to quit smoking for your own health and that of your growing baby; try the Centers for Disease Control and Prevention if you’re in the US or the NHS if you’re in the UK.
Alcohol
Experts agree that there is no “safe” amount of alcohol that can be drunk during pregnancy, while research suggests that alcohol consumption can increase the risk of miscarriage. That risk was not related to the number of drinks per week, beverage type, or binge drinking, meaning that alcohol may sadly be linked to a miscarriage even at low levels of consumption. If you’re looking for some ideas of non-alcoholic drinks that are safe to consume during pregnancy, you can read our article on the best drinks to have during pregnancy.
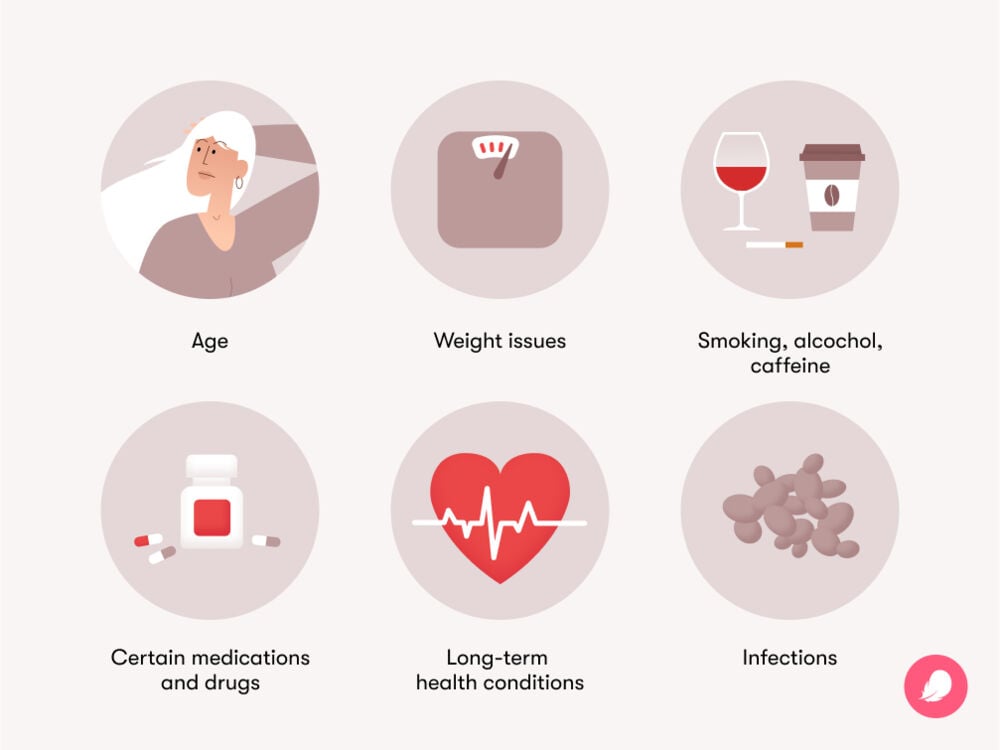
Drugs
Using recreational drugs, including cannabis and cocaine, can affect your baby as these substances can pass through the placenta. Research on drug use and miscarriage is limited, but we do know the use of marijuana, stimulants, and prescription painkillers is associated with more than two times the risk of stillbirth. The American College of Obstetricians and Gynaecologists advises that any illegal drug use or abuse of prescription medications could cause birth defects or pregnancy loss.
Caffeine
Excessive caffeine consumption can increase the risk of early pregnancy loss, so drinking too much coffee during the first trimester could be linked to a miscarriage. One analysis suggested that the risk of pregnancy loss rose by 19% for every increase in caffeine intake of 150 mg/day and by 8% for every increase in coffee intake of two cups per day. Current guidelines recommend limiting your intake to 200 mg of caffeine per day (around two cups of coffee). Remember that caffeine is also found in tea, colas, and energy drinks, as well as food such as chocolate.
Certain medications
Taking some medications can increase the risk of miscarriage, including:
- Misoprostol, used for stomach ulcers
- Retinoids, used for eczema and acne
- Methotrexate, used for conditions such as rheumatoid arthritis
- Nonsteroidal anti-inflammatory drugs, such as ibuprofen
If you’re unsure whether it’s safe to continue taking your usual medicines during pregnancy or while trying to conceive, always speak to your health care provider first.
What physical activity should be avoided to help avoid miscarriage?
“Physical activity is great during pregnancy, and there’s no need to avoid exercise,” advises Dr. Rogers. “It’s healthy for your heart, muscles, and bones, so I typically recommend continuing any exercise that you have been doing, as long as you are not at high risk of falling.”
A fall during pregnancy could trigger a miscarriage, so activities with a risk of falling, including outdoor bike riding, roller blading, horse riding, sledding, skating, or skiing, may be best avoided. High-intensity exercises, such as jogging, ball games, and racket spots, are also associated with increased miscarriage risk during the first trimester. Remember that if you have any questions or concerns about safe exercising during pregnancy, you can always discuss these with your doctor.
Can mental health cause miscarriage?
Pregnancy can be a challenging time, full of mixed emotions and concerns, which may understandably have an impact on your mental health. If you’re struggling with low mood or excessive worry during pregnancy and wondering whether stress can cause miscarriage, it may be reassuring to know that it does not.
“While it is always a good idea to reduce stress during pregnancy, stress itself does not cause a loss,” Dr. Rodgers explains. That doesn’t mean you have to suffer in silence, though; you can seek perinatal mental health support from your doctor.
There is some evidence to suggest that having a preexisting psychiatric disorder may increase the risk of pregnancy loss. Research found an increased risk in women with bipolar disorder, personality disorders, attention-deficit hyperactivity disorder, conduct disorders, anxiety disorders, depressive disorders, somatoform disorders (mental disorders that can cause unexplained physical symptoms), and eating disorders, but not enough is known yet about exactly what the link is. The most important thing for both you and your baby is to ensure your condition is well managed and that you don’t stop taking any prescribed psychiatric medication without first seeking medical advice.
Women who have experienced a miscarriage can understandably be at increased risk of depression and anxiety, as well as post-traumatic stress disorder, as a result of their loss. Research suggests the profound psychological impact of experiencing one miscarriage can, in turn, increase the risk of subsequent miscarriage, but try not to focus on this possibility as the chances are still very slim. If you have previously suffered a pregnancy loss, be sure to look after yourself and seek support to help you manage your grief; organizations such as Share Pregnancy and Infant Loss Support in the US and Tommy’s in the UK can provide further information.
The takeaway: Miscarriages causes and risk
Ultimately, it’s difficult to pinpoint exactly what causes miscarriage. In most cases, the cause is genetic issues or other factors that cannot be controlled. However, there are lifestyle tweaks you can make to mitigate certain risk factors. “Being as healthy as you can be is always a good idea — not smoking or using nicotine, as well as limiting caffeine and alcohol,” Dr. Rodgers says.
But whatever happens, she adds, “It’s important to remember that miscarriage is never your fault and that most pregnancies after a miscarriage go on to be successful.” Indeed, less than 5% of women who miscarry have two consecutive miscarriages, and only 1% experience three or more pregnancy losses in a row.
If you do experience more than one miscarriage, be sure to speak to your doctor. They can help to identify any issues and discuss any possible treatment options with you. And remember that 60% to 80% of women who experience unexplained recurrent miscarriages do go on to have healthy pregnancies. So be sure to be kind to yourself and take the space, time, and support you need if you do experience miscarriage, no matter how early on or what the circumstances are.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Early Pregnancy Loss.” The American College of Obstetricians and Gynecologists, www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2018/11/early-pregnancy-loss. Accessed 5 Dec. 2022.
“Moderate Caffeine Consumption during Pregnancy.” The American College of Obstetricians and Gynecologists, www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2010/08/moderate-caffeine-consumption-during-pregnancy. Accessed 6 Dec. 2022.
“Pregnancy with Type 1 or Type 2 Diabetes.” The American College of Obstetricians and Gynecologists, www.acog.org/womens-health/faqs/pregnancy-with-type-1-or-type-2-diabetes. Accessed 6 Dec. 2022.
“Tobacco, Alcohol, Drugs, and Pregnancy.” The American College of Obstetricians and Gynecologists, www.acog.org/womens-health/faqs/tobacco-alcohol-drugs-and-pregnancy. Accessed 6 Dec. 2022.
“Bleeding and/or Pain in Early Pregnancy Patient Information Leaflet.” The Royal College of Obstetricians & Gynaecologists, www.rcog.org.uk/for-the-public/browse-all-patient-information-leaflets/bleeding-andor-pain-in-early-pregnancy-patient-information-leaflet/. Accessed 16 Dec. 2022.
Hamilton, B. E., et al. “Vital Statistics Rapid Release.” Centers for Disease Control and Prevention, www.cdc.gov/nchs/data/vsrr/vsrr-007-508.pdf. Accessed 5 Dec. 2022.
Du Fossé, N. A., et al. “Advanced Paternal Age Is Associated with an Increased Risk of Spontaneous Miscarriage: A Systematic Review and Meta-Analysis.” Human Reproduction Update, vol. 26, no. 5, 2020, pp. 650–69, doi.org/10.1093/humupd/dmaa010.
“Falling during Pregnancy: Reason to Worry?” Mayo Clinic, 21 Jan. 2022, www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-answers/fall-during-pregnancy/faq-20119023.
“Fetal Alcohol Syndrome.” Mayo Clinic, 10 Jan. 2018, www.mayoclinic.org/diseases-conditions/fetal-alcohol-syndrome/symptoms-causes/syc-20352901.
Gao, R., et al. “Systemic Autoimmune Diseases and Recurrent Pregnancy Loss: Research Progress in Diagnosis and Treatment.” Chinese Medical Journal, vol. 134, no. 17, 2021, pp. 2140–42, doi.org/10.1097/cm9.0000000000001691.
Li, J., et al. “A Meta-Analysis of Risk of Pregnancy Loss and Caffeine and Coffee Consumption during Pregnancy.” International Journal of Gynaecology and Obstetrics, vol. 130, no. 2, 2015, pp. 116–22, doi.org/10.1016/j.ijgo.2015.03.033.
Madsen, M., et al. “Leisure Time Physical Exercise during Pregnancy and the Risk of Miscarriage: A Study within the Danish National Birth Cohort.” BJOG, vol. 114, no. 11, 2007, pp. 1419–26, doi.org/10.1111/j.1471-0528.2007.01496.x.
Magnus, M. C., et al. “Risk of Miscarriage in Women with Psychiatric Disorders.” The British Journal of Psychiatry, vol. 219, no. 3, 2021, pp. 501–06, doi.org/10.1192/bjp.2020.259.
“Implantation Bleeding: Common in Early Pregnancy?” Mayo Clinic, 19 Apr. 2022, www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-answers/implantation-bleeding/faq-20058257.
“Miscarriage.” Mayo Clinic, 16 Oct. 2021, www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptoms-causes/syc-20354298.
“Does PCOS Affect Pregnancy?” Eunice Kennedy Shriver National Institute of Child Health and Human Development, www.nichd.nih.gov/health/topics/pcos/more_information/FAQs/pregnancy. Accessed 6 Dec. 2022.
“Pregnancy Loss (Before 20 Weeks of Pregnancy).” Eunice Kennedy Shriver National Institute of Child Health and Human Development, www.nichd.nih.gov/health/topics/factsheets/pregnancyloss. Accessed 5 Dec. 2022.
“Substance Use While Pregnant and Breastfeeding.” National Institute on Drug Abuse, 4 May 2022, nida.nih.gov/publications/research-reports/substance-use-in-women/substance-use-while-pregnant-breastfeeding.
Ng, KaYingBonnie, et al. “Systematic Review and Meta-Analysis of Female Lifestyle Factors and Risk of Recurrent Pregnancy Loss.” Scientific Reports, vol. 11, 2021, p. 7081, doi.org/10.1038/s41598-021-86445-2.
“Miscarriage: Causes.” NHS, www.nhs.uk/conditions/miscarriage/causes/. Accessed 6 Dec. 2022.
Pineles, Beth L., et al. “Systematic Review and Meta-Analysis of Miscarriage and Maternal Exposure to Tobacco Smoke during Pregnancy.” American Journal of Epidemiology, vol. 179, no. 7, 2014, pp. 807–23, doi.org/10.1093/aje/kwt334.
Sundermann, Alexandra C., et al. “Week-by-week Alcohol Consumption in Early Pregnancy and Spontaneous Abortion Risk: A Prospective Cohort Study.” American Journal of Obstetrics and Gynecology, vol. 224, no. 1, 2021, p. 97.e1–97.e16, doi.org/10.1016/j.ajog.2020.07.012.
“Tobacco, Alcohol, Drugs, and Pregnancy.” The American College of Obstetricians and Gynecologists, www.acog.org/womens-health/faqs/tobacco-alcohol-drugs-and-pregnancy. Accessed 5 Jan. 2023.
Tong, Stephen, et al. “Miscarriage Risk for Asymptomatic Women after a Normal First-Trimester Prenatal Visit.” Obstetrics & Gynecology, vol. 111, no. 3, 2008, pp. 710–14, doi.org/10.1097/AOG.0b013e318163747c.
“TORCH Infections.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/23322-torch-syndrome. Accessed 5 Jan. 2023.
“Miscarriage.” MedlinePlus, medlineplus.gov/ency/article/001488.htm. Accessed 5 Dec. 2022.
Williams, D., and Davison, J. “Chronic Kidney Disease in Pregnancy.” BMJ, vol. 336, no. 7637, 2008, pp. 211–15, doi.org/10.1136/bmj.39406.652986.be.
Wang, Y., et al. “Anxiety and Depression Are Risk Factors for Recurrent Pregnancy Loss: A Nested Case-Control Study.” Health and Quality of Life Outcomes, vol. 19, no. 1, 2021, p. 78, doi.org/10.1186/s12955-021-01703-1.
“Infections in Pregnancy That May Affect Your Baby.” NHS, www.nhs.uk/pregnancy/keeping-well/infections-that-may-affect-your-baby/. Accessed 16 Dec. 2022.

