An abdominal pregnancy is a form of ectopic pregnancy that sadly results in pregnancy loss. While it’s very rare, it can be a difficult thing to experience. Here, a doctor explains everything you need to know; plus, a psychiatrist shares tips to care for your mental health along with where to go for support.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
What is an abdominal pregnancy?

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Sadly, not every pregnancy will go according to plan. There are a handful of rare conditions that can sometimes pose a risk to the health of the fetus or the pregnant person. One of these is abdominal pregnancy, a type of ectopic pregnancy that will, unfortunately, result in a pregnancy loss. This is a difficult thing to go through, and understandably, it can be hard to cope with.
If you are reading this article, you or someone you know might have experienced an abdominal pregnancy. Grief often comes with losing a baby, and it’s a completely normal reaction. You might also be experiencing health issues that can sometimes occur alongside an abdominal pregnancy (physical, mental, or both), making this difficult moment even harder to navigate.
While all this can be hard to work through, take some comfort in knowing that you are absolutely not alone; there is always help and support available.
One of the most useful ways to begin processing an abdominal pregnancy can be to learn more about it. To equip you with all the details you might need and hopefully provide some reassurance, we’ve spoken to OB-GYN (obstetrician and gynecologist) Dr. Sara Twogood and professor of psychological medicine Kathryn Abel, PhD. We’ve also included details for some support services at the end of this article.
What is an abdominal pregnancy, and how common is it?
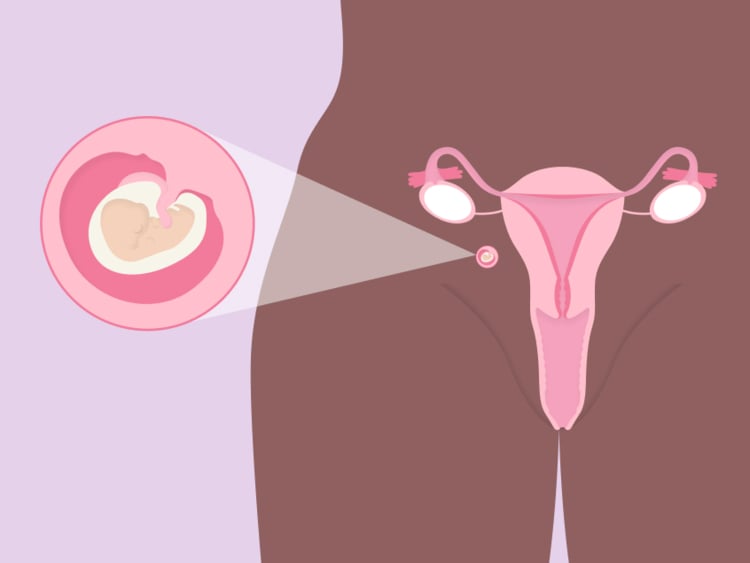
It can be helpful to first understand what an abdominal pregnancy is and how rare it is. To do this, let’s look at the journey a fertilized egg typically makes. Generally speaking, it will travel from the uterine tube into the uterus, where it will implant in the uterus wall and grow as an embryo.
Sometimes, however, the fertilized egg doesn’t reach the uterus but implants elsewhere in the body. There is little understanding about exactly why this happens, but the most important thing to know is that this process cannot be controlled. It is absolutely not the fault of the person carrying the baby. This process is known as an ectopic pregnancy, which occurs in around 1% to 2% of pregnancies, according to US statistics. Very sadly, it means the pregnancy is unviable (unable to continue to full term) as there is no way for it to be safely reimplanted inside the uterus.
Most ectopic pregnancies — 95% — take place in the uterine tubes. But sometimes, very rarely, they can occur in the abdomen. Across more than 20 years, researchers who surveyed women in the United States found that abdominal pregnancies account for just 1.4% of ectopic pregnancies, and as we know, ectopic pregnancies are uncommon in themselves.
What are the symptoms of an abdominal pregnancy, and how do they occur?
Because abdominal pregnancies are a rare type of ectopic pregnancy, the signs tend to be the same as for other ectopic pregnancies. You might not experience any symptoms at all, but if you do, they may include vaginal bleeding, pain in your abdomen or shoulder, or discomfort when peeing or pooping. Symptoms of an ectopic pregnancy are most likely to occur between the 4th and 12th week of pregnancy; however, abdominal pregnancies tend to present much later than ectopic pregnancies that take place in the uterine tubes because there is more room for growth.
It’s important not to automatically jump to conclusions if you notice any bleeding or pain during early pregnancy, however. Bleeding in the first trimester can occur in 27% of pregnancies. “It does not mean the pregnancy will miscarry or be an ectopic,” says Dr. Twogood, adding, “Cramping pain is also common in early pregnancy.” So if you experience these symptoms, don’t panic; remember that abdominal pregnancies are incredibly rare. If you are concerned, however, make sure to call your health care provider and schedule a checkup.
Whatever the outcome, experiencing these symptoms during pregnancy can be unsettling and scary. Lean on your loved ones for support and help, and try not to search the web for medical advice; only take the advice of professionals during this time.
When and how are abdominal pregnancies usually detected?
“When a patient is being evaluated in early pregnancy, a physical exam and ultrasound are performed, and the level of beta hCG (the pregnancy hormone) is checked (often twice over the course of 48 hours),” explains Dr. Twogood.
For those who are experiencing an ectopic or abdominal pregnancy, the level of beta hCG is likely to be lower and rise more slowly. An ultrasound will reveal if there’s an ectopic or abdominal pregnancy, but if these tests are unclear, doctors will consider more blood tests, further scans, or surgery to make a firm diagnosis.

If you have just been diagnosed with an abdominal pregnancy, Dr. Abel says it’s completely understandable that you may “experience a mix of fear, anxiety and grief.” You may need some time to come to terms with it or want more information and guidance about what the diagnosis means. With this in mind, Dr. Abel explains that “most experienced obstetric teams will be fully aware that this news can come as a great shock” and should be able to offer the support you need. “Grief counseling and peer support are available, depending on where you live,” she adds.
What does an abdominal pregnancy mean for the baby, and how do doctors treat it?
Regrettably, a fetus in an ectopic or abdominal pregnancy cannot be saved, meaning it will almost always result in a pregnancy loss. This can naturally trigger emotional distress for some people, but from a physical perspective, Dr. Twogood explains that there are two main treatments for ectopic pregnancies. “One is a medication called methotrexate that can stop the pregnancy from growing,” she says. “The second is surgery to remove the pregnancy. Your doctor will help you decide which of these options is best because it depends on many individual factors.”
Do abdominal pregnancies have health implications for the pregnant person?
Abdominal pregnancies can, unfortunately, have health implications for the mother or person carrying the fetus, such as internal bleeding. “This can be life threatening for the mother and may necessitate emergency surgery and a blood transfusion,” explains Dr. Twogood. We know this sounds scary, but remember that your health care provider and their team will know the safest way to help you get through this and recover as quickly as possible.
Understandably, an abdominal pregnancy can also take a toll on your mental health. “Everyone deals with loss in different ways,” says Dr. Abel. “Overall, women experiencing abdominal pregnancy are at similar risk of developing depression postnatally as women with healthy pregnancies. And the level of anxiety during the time they are still pregnant may be greater given the potential risks involved.”
“You need to give yourself time and avoid blame”
Remember that you’re not alone. If you or someone you know is struggling with their mental health or feelings of anxiety, there is help available. You can lean on your loved ones for support, and there are also plenty of resources available to help you work through this incredibly difficult time. As a first port of call, you could speak to the doctor who diagnosed you to answer any questions. They should also be able to point you in the direction of further support in your area such as a specialized organization or a counselor. There’s also a list of specialist pregnancy loss helplines and support services at the end of this article.
Does experiencing an abdominal pregnancy mean you are more likely to have one again in the future?
Unfortunately, if you’ve had one ectopic pregnancy, such as an abdominal pregnancy, then you are at a slightly increased risk of having another one in the future. This may understandably make you feel fearful of a repeat event, but it’s important to remember that the risk of having another ectopic pregnancy is only around 10%, and 65% of women go on to have a healthy pregnancy within 18 months of an ectopic pregnancy.
“I know this information sounds scary, and it can be,” adds Dr. Twogood. “But ectopic and abdominal pregnancies are rare, and if you are in the small minority of people that have one, I want you to have heard of it before and have knowledge so you aren’t as overwhelmed by the diagnosis and treatment options.”
How can you help yourself to recover from the loss of a pregnancy?
Going through a pregnancy loss can be an incredibly difficult time, so remember to be kind to yourself, seek support from your loved ones, and look for further assistance if you want it. “You need to give yourself time, avoid blame, and have enough opportunity to talk to clinicians about future pregnancies, risks, and protective factors,” says Dr. Abel.
You might also want to consider talking to a therapist. “Having the opportunity to talk through traumatic events is consistently shown to be valuable for people,” she explains.
Abdominal pregnancy: The takeaway
As with any ectopic pregnancy, know that there is absolutely nothing you could have done to change things. It’s totally natural to experience feelings of grief and sadness following a miscarriage, so give yourself time to heal, and don’t underestimate the physical toll it can take on your body, too.
If you feel you need it, there are various organizations that offer further support. The US-based Share Pregnancy and Infant Loss Support offers advice and online support groups. The Miscarriage Association offers specific information on ectopic pregnancies, as does Tommy’s. Both are based in the United Kingdom but can be accessed worldwide.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Baffoe, P., et al. “Term Abdominal Pregnancy with Healthy Newborn: A Case Report.” Ghana Medical Journal, vol. 45, no. 2, June 2011, pp. 81–83. Accessed 28 Feb. 2022.
Bouyer, J., et al. “Sites of Ectopic Pregnancy: A 10 Year Population-Based Study of 1800 Cases.” Human Reproduction, vol. 17, no. 12, Dec. 2002, pp. 3224–30, https://doi.org/10.1093/humrep/17.12.3224. Accessed 14 Mar. 2022.
Breen, James L. “A 21 Year Survey of 654 Ectopic Pregnancies.” American Journal of Obstetrics and Gynecology, vol. 106, no. 7, Apr. 1970, pp. 1004–19, https://doi.org/10.1016/S0002-9378(16)34087-X. Accessed 14 Mar. 2022.
Chauhan, Suneet P. “Abdominal Pregnancy.” UpToDate, 2022, https://www.uptodate.com/contents/abdominal-pregnancy. Accessed 14 Mar. 2022.
"Current Trends Ectopic Pregnancy -- United States, 1990-1992." Centers for Disease Control and Prevention. 27 Jan. 1995, https://www.cdc.gov/mmwr/preview/mmwrhtml/00035709.htm. Accessed 14 Mar. 2022.
“Depression during and after Pregnancy.” Centers for Disease Control and Prevention, 15 Dec. 2021, https://www.cdc.gov/reproductivehealth/features/maternal-depression/index.html. Accessed 28 Feb. 2022.
“Ectopic Pregnancy.” NHS, 18 Nov. 2021, www.nhs.uk/conditions/ectopic-pregnancy/. Accessed 28 Feb. 2022.
“Ectopic Pregnancy.” The Miscarriage Association, 29 Sept. 2016, https://www.miscarriageassociation.org.uk/information/ectopic-pregnancy/. Accessed 28 Feb. 2022.
“Ectopic Pregnancy - Diagnosis and Treatment.” Mayo Clinic, 18 Dec. 2020, www.mayoclinic.org/diseases-conditions/ectopic-pregnancy/diagnosis-treatment/drc-20372093. Accessed 28 Feb. 2022.
“Ectopic Pregnancy Information and Support.” Tommy’s, https://www.tommys.org/baby-loss-support/ectopic-pregnancy-information-support. Accessed 28 Feb. 2022.
Ego, A., et al. “Survival Analysis of Fertility after Ectopic Pregnancy.” Fertility and Sterility, vol. 75, no. 3, Mar. 2001, pp. 560–66, https://doi.org/10.1016/s0015-0282(00)01761-1. Accessed 14 Mar. 2022.
“Fertilization and Implantation.” Mayo Clinic, 15 Nov. 2021, https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/multimedia/fertilization-and-implantation/img-20008656. Accessed 28 Feb. 2022.
Hasan, Reem, et al. “Association between First-Trimester Vaginal Bleeding and Miscarriage.” Obstetrics and Gynecology, vol. 114, no. 4, Oct. 2009, pp. 860–67, https://doi.org/10.1097/AOG.0b013e3181b79796. Accessed 14 Mar. 2022.
“Home.” Share Pregnancy & Infant Loss Support, 31 Oct. 2018, https://nationalshare.org/. Accessed 28 Feb. 2022.
"New Ohio Bill Falsely Suggests That Reimplantation of Ectopic Pregnancy Is Possible.” Consult QD, 11 Feb. 2020, https://consultqd.clevelandclinic.org/new-ohio-bill-falsely-suggests-that-reimplantation-of-ectopic-pregnancy-is-possible/. Accessed 14 Mar. 2022.
“Stomach Pain in Pregnancy.” NHS, 18 Nov. 2021, www.nhs.uk/pregnancy/related-conditions/common-symptoms/stomach-pain. Accessed 28 Feb. 2022.

