“Post-pill PCOS” is a medical myth. But your periods can become irregular when you stop taking the pill — and you may experience other symptoms that could be linked to PCOS. Here’s the lowdown on why this can happen with advice from a Flo expert.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Can birth control cause PCOS? Here are the facts

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
When you’re figuring out which birth control you’d like to use, there’s a lot to consider. It needs to fit with what’s going on in your life right now, along with your health history. You might also have a method in mind that you prefer.
The pill is an effective, convenient contraceptive method — and a popular choice for a lot of people. In fact, a 2020 report found the pill was the most used reversible contraception in the United States, with 14% of women taking it. But on the flip side, the pill can cause unwanted side effects for some, including headaches and irritability.
“Post-pill PCOS” can also come up as a possible side effect when you’re doing your research. This is the unfounded idea that taking the pill could cause the condition polycystic ovary syndrome or PCOS. There isn’t any truth in this, but let’s break down where this medical myth comes from. Plus, we’ll discuss reasons you might experience symptoms like irregular periods when you stop taking the pill.
Key takeaways
- PCOS is a condition that affects how your ovaries work. It’s estimated that 8% to 13% of reproductive-age women have PCOS.
- While you may have come across misinformation online, taking hormonal birth control does not cause PCOS.
- Some people experience symptoms associated with PCOS — like irregular periods — after stopping birth control. This is often because your body is adjusting to changing hormone levels and usually regulates itself within a few months.
- While hormonal birth control doesn’t cause PCOS, it can mask some symptoms by making your period appear regular. This can mean that when you stop taking birth control, PCOS symptoms can start or come back.
Can birth control cause PCOS?
The simple answer is no, it can’t. While some people worry that “pill-induced PCOS” is a thing, it isn’t a medical condition or something that doctors recognize.
In fact, the opposite is true. Hormonal birth control is often used to “counteract some of the effects of PCOS,” explains Dr. Jenna Beckham, obstetrician, gynecologist, and complex family planning specialist, WakeMed Health and Hospitals, Planned Parenthood South Atlantic, North Carolina, US.
That means your doctor may recommend the pill as a way to regulate your cycle if you have PCOS and don’t have regular periods. They may also prescribe it to help with another common PCOS symptom: acne.
So why do some of us mistakenly think the pill can cause PCOS? It’s likely due to some people’s periods being unpredictable when they come off the pill. “Depending on their history and how long they’ve been on birth control pills, some patients will [notice a] change in their cycle,” Dr. Beckham explains.
This makes sense because the pill works by releasing hormones that suppress ovulation. So when you come off the pill, your body needs to readjust to the changing hormone levels. “It may take a little bit of time for it to regulate again,” Dr. Beckham says. Up to three months is normal. However, if you have any concerns or other symptoms, then schedule an appointment with your doctor.
Take a quiz
Find out what you can do with our Health Assistant
What causes PCOS?
So, if the pill doesn’t cause PCOS, then what does? Frustratingly, the exact cause of PCOS isn’t totally understood, but it may be linked to an imbalance in your hormone levels.
Here’s the science: Our cycle relies on lots of different hormones in order to stay in sync. Doctors think that PCOS occurs when your ovaries produce higher than normal levels of hormones known as androgens. The most commonly known androgen is testosterone. Sometimes androgens are considered “male hormones” because they are found in higher levels in men, but it is normal for both women and men to have androgens.
If you have high androgen levels as a result of PCOS, then it can cause changes to your cycle when you’re not using hormonal birth control, such as:
- Having an irregular cycle. That means your periods have a smaller (fewer than 21 days) or larger (35 days or more) than average gap between them. You might also experience heavier or lighter bleeding than usual or miss three or more periods in a row.
- Not ovulating or releasing an egg every cycle. This is why PCOS can sometimes make it harder to become pregnant. Please know that lots of people with PCOS go on to get pregnant and have healthy babies.
Another common feature of PCOS relates to how people’s ovaries can appear on ultrasound. PCOS gets its name from exactly this finding. The “cysts” in PCOS are actually lots of small fluid-filled sacs called follicles.
These follicles contain immature eggs that are not developing or getting ready for ovulation as they normally do. While this might sound scary, the multiple follicles are not painful or dangerous and will not need to be surgically removed. These cysts are also caused by high levels of androgens, but not every person with PCOS has them. Doctors aren’t sure why this happens.
What they do know is that PCOS can develop any time after you’ve started puberty. Frustratingly, though, it can sometimes take up to 12 years to get a diagnosis. And while it’s hard to know why some people develop the condition, you may be more likely to have PCOS if other people in your family have been diagnosed with it.
Why “post-pill PCOS” doesn’t exist
So, let’s clear this up: Medical experts don’t recognize post-pill PCOS as a condition. But if you’ve heard about it from friends or online, then it’s helpful to unpack why this myth exists.
Whether you’ve been diagnosed with PCOS or not, you might recognize some of these symptoms, like an irregular cycle, from a time before you started taking hormonal birth control. It’s important to remember that PCOS isn’t the only reason why you might have an irregular cycle.
Once you started taking hormonal birth control, your cycle might have become more regular, or you might not have had a bleed at all, even if you had PCOS. However, if you had irregular cycles before starting the pill, unfortunately, your cycles will probably go back to being irregular off of the pill. This might make it seem like the pill has caused PCOS when, in fact, your pill might have just masked some of the symptoms associated with PCOS.
As hormonal birth control can regulate your cycle, it means you can’t be assessed for PCOS while you’re taking it. You may already have PCOS and just not know until you come off the contraceptive pill. Alternatively, you may come off the contraceptive pill and mistake your period not returning to a regular cycle for a few weeks or months as a sign of PCOS.
Do post-pill symptoms go away?
Since it can take your body a few months to adjust to the change in hormones when you stop taking the pill, you may notice changes to your menstrual cycle and symptoms.
That’s because, as Dr. Beckham explains, “a lot of hormonal birth controls can be beneficial in managing some other symptoms that are related to changes in hormones.” She says that includes “mood symptoms, cramping, and some of the premenstrual emotional symptoms.”
So, you might find that your periods have become longer or shorter since coming off birth control. Or they might be heavier or more painful. Perhaps you’re having more mood swings or your premenstrual symptoms feel worse than they were before.
Rest assured that this is normal. However, these changes can sometimes be disruptive and uncomfortable, so go easy on yourself. If you’re worried about symptoms after coming off the pill, then talk to your doctor. Similarly, if your cycle hasn’t returned within three months after going off birth control, book an appointment with your health care provider.
“Obviously, each individual can make their own decision, and if after one month, they’re feeling very stressed about it, or they’re having a lot of negative symptoms, it’s always worth having a conversation with their provider,” says Dr. Beckham. “But absolutely, if at the three-month mark, they’ve not had a return to regular cycles, or they’re still having a lot of other symptoms that they’re concerned about, I would absolutely recommend making an appointment and talking about it with their provider.”
How to tell if it’s PCOS
Now that you know that it can take some time before your cycle becomes regular after coming off hormonal birth control, here’s how to spot some of the signs that might point to PCOS.
Signs of PCOS
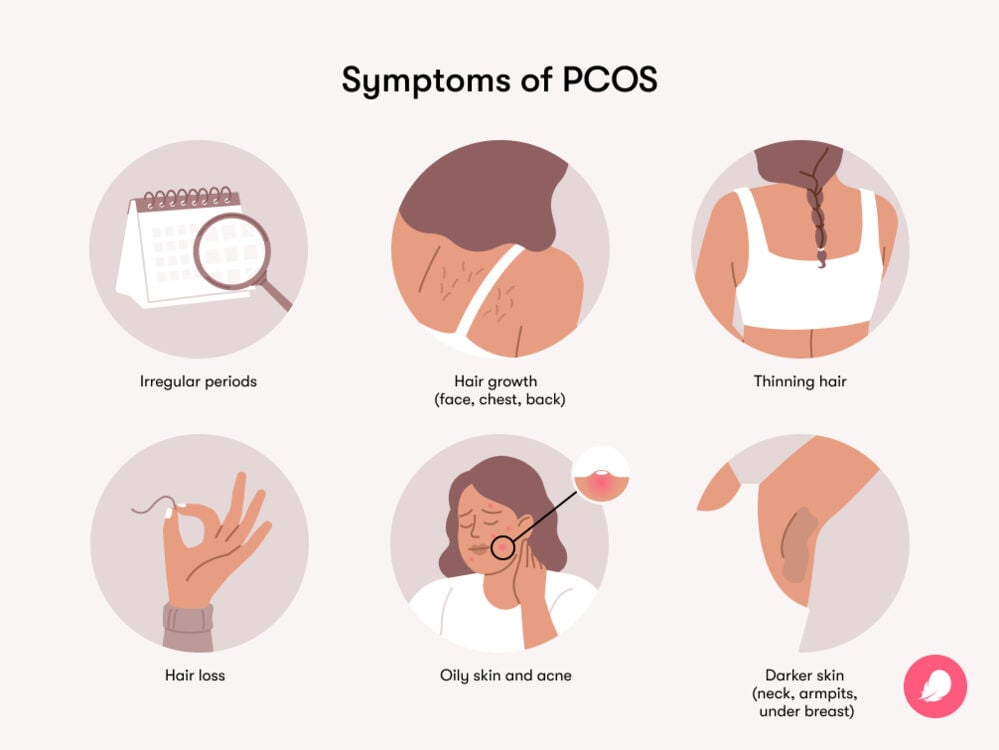
Not everyone with PCOS has all of the symptoms, and they can vary in severity for each person. But some common signs include:
- Irregular periods or no periods
- Difficulty becoming pregnant
- Dark, thick hair growth on areas like your face, chest, and back
- Weight gain, especially around your belly, and difficulty maintaining a weight that’s healthy for you
- Thinning hair and hair loss from your head
- Oily skin and acne
- Skin tags (excess pieces of skin on your neck and armpits)
- Skin that’s darker or thicker on your neck, armpit, and under your boobs
It’s hard to stay on top of multiple symptoms. Flo’s Symptom Checker feature can give you the information you need to have a confident conversation with your doctor about what’s going on inside your body.
PCOS diagnosis
If you recognize some of the symptoms above, then it’s time to reach out to your doctor.
What can you expect once you’re there? At the start of your appointment, they may ask you questions about what your cycle is usually like, any symptoms you’ve had or felt, and your family health history. This may feel personal, but this information can help you get the answers you need.
You might be referred for further tests and a follow-up appointment. They will use the following criteria to diagnose PCOS:
- Do you have irregular or infrequent periods?
- Do you have increased levels of androgens? This can be found by doing a blood test to check hormone levels. Some of the physical signs of PCOS, like hair growth on areas like your face or acne, can also be a sign that you have high levels of androgens.
- Does an ultrasound show that you have cysts on your ovaries?
If you meet two of the three criteria, then they may diagnose you with PCOS.
Having a clear picture of any patterns in your cycles and symptoms can help you during these appointments. You may want to use Flo’s cycle report feature to get information you can easily share with your health care provider.
Final thoughts on hormonal birth control
Being unsure about changes in your cycle can be daunting. However, rest assured, if you’re worried about the pill impacting your longer-term fertility or health once you stop taking it, know that there isn’t any evidence of that happening.
“As long as you don’t have any medical [reasons why you shouldn’t be using] hormonal birth control, inherently they don’t have any risk,” Dr. Beckham explains, adding that this “ultimately does not itself impact the future success of fertility.”
More FAQs about birth control and PCOS
How long does “post-pill syndrome” last?
Remember, “post-pill syndrome” isn’t a recognized medical condition, but after stopping the pill, you may experience new symptoms and cycle changes.
Dr. Beckham notes that this usually lasts for around three months. If you’re concerned about any changes or your cycle doesn’t return to what’s typical for you after three months, tell your health care provider.
Can coming off birth control cause ovarian cysts?
While this answer is a little complicated — technically it’s a no. However, Dr. Beckham explains that we need to reframe how we think of ovarian cysts as they can form during the ovulation process, which isn’t always a bad thing. They may also be more common than you think.
During your menstrual cycle, small fluid-filled sacs called follicles develop on your ovaries that store maturing eggs. If the egg is released, then these sacs shrink. However, sometimes they don’t, and a follicle can grow extra large. This can become a cyst.
Sometimes, “there can be some bleeding into them,” explains Dr. Beckham. “So actually taking birth control pills can be used in individuals who have a history of recurrent cysts to [stop] ovulation and reduce that occurrence.”
If you stop taking hormonal birth control, then you’re no longer putting a pause on ovulation. So, your body will start to ovulate again, and you might start to experience cysts related to ovulation again.
However, it’s worth keeping in mind that for the vast majority of people, ovulation is typical, and the cysts that form at this point in your cycle aren’t painful, dangerous, or anything to worry about. See your doctor if you have any concerns.
Can you suddenly develop PCOS?
You can get PCOS symptoms any time after puberty starts, but most people are diagnosed in their 20s and 30s.
“It can really happen anytime,” Dr. Beckham explains, adding that “significant changes in weight” can be a trigger for PCOS starting.
Remember that you can lean on your health care provider and a symptom- and cycle-tracking app like Flo to spot patterns around what’s normal for you.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“6 Things That Can Happen When You Stop Taking the Pill.” Cleveland Clinic, 7 Aug. 2019, health.clevelandclinic.org/6-things-that-can-happen-when-you-stop-taking-the-pill.
“Androgens.” Cleveland Clinic, my.clevelandclinic.org/health/articles/22002-androgens. Accessed 31 July 2024.
Barber, Thomas M., et al. “Obesity and Polycystic Ovary Syndrome: Implications for Pathogenesis and Novel Management Strategies.” Clinical Medicine Insights: Reproductive Health, vol. 13, Sep. 2019, doi:10.1177/1179558119874042.
“Birth Control.” Mayo Clinic, 10 May 2023, www.mayoclinic.org/healthy-lifestyle/birth-control/in-depth/birth-control-pill/art-20045136.
“Birth Control Pills.” Cleveland Clinic, my.clevelandclinic.org/health/treatments/3977-birth-control-the-pill. Accessed 31 July 2024.
“Can Birth Control Cause Infertility?” Cleveland Clinic, 17 Jan. 2023, health.clevelandclinic.org/can-birth-control-make-you-infertile.
“Excessive Hair Growth (Hirsutism).” NHS, www.nhs.uk/conditions/hirsutism/. Accessed 31 July 2024.
“Irregular Periods.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/14633-abnormal-menstruation-periods. Accessed 31 July 2024.
“Ovarian Cysts.” Mayo Clinic, 28 July 2023, www.mayoclinic.org/diseases-conditions/ovarian-cysts/symptoms-causes/syc-20353405.
“Polycystic Ovary Syndrome (PCOS).” Cleveland Clinic, my.clevelandclinic.org/health/diseases/8316-polycystic-ovary-syndrome-pcos. Accessed 31 July 2024.
Peven, Kimberly, et al. “Assessment of a Digital Symptom Checker Tool’s Accuracy in Suggesting Reproductive Health Conditions: Clinical Vignettes Study.” JMIR mHealth and uHealth, vol. 11, Dec. 2023, doi: 10.2196/46718.
“Polycystic Ovary Syndrome.” World Health Organization, 28 June 2023, www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome.
“Polycystic Ovary Syndrome.” Office on Women’s Health, 22 Feb. 2021, www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome.
“Polycystic Ovary Syndrome (PCOS).” Mayo Clinic, 8 Sep. 2022, www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439.
“Polycystic Ovary Syndrome (PCOS).” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/polycystic-ovary-syndrome-pcos. Accessed 31 July 2024.
“What Happens to Your Body When You Come off the Pill?” Patient, 26 Oct. 2023, patient.info/news-and-features/what-happens-to-your-body-when-you-come-off-the-pill.




