It’s a condition that impacts around one in 10 women around the world.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Everything you need to know about endometriosis

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Many of us know the pain of period cramps. Your hot water bottle can become your best friend during certain times of the month when your back, abdomen, and even legs are aching. But if those cramps become debilitating, they may not be caused by just your period — they could be a sign of endometriosis.
Endometriosis can sound like a bit of a mouthful. That’s why you might have heard some people call it “endo” for short. It’s a condition that affects around one in 10 women of reproductive age worldwide, but it can take several years on average for a diagnosis. For those who’d like the lowdown on endometriosis, we asked a Flo expert to break down everything you need to know about the condition.
What is endometriosis?
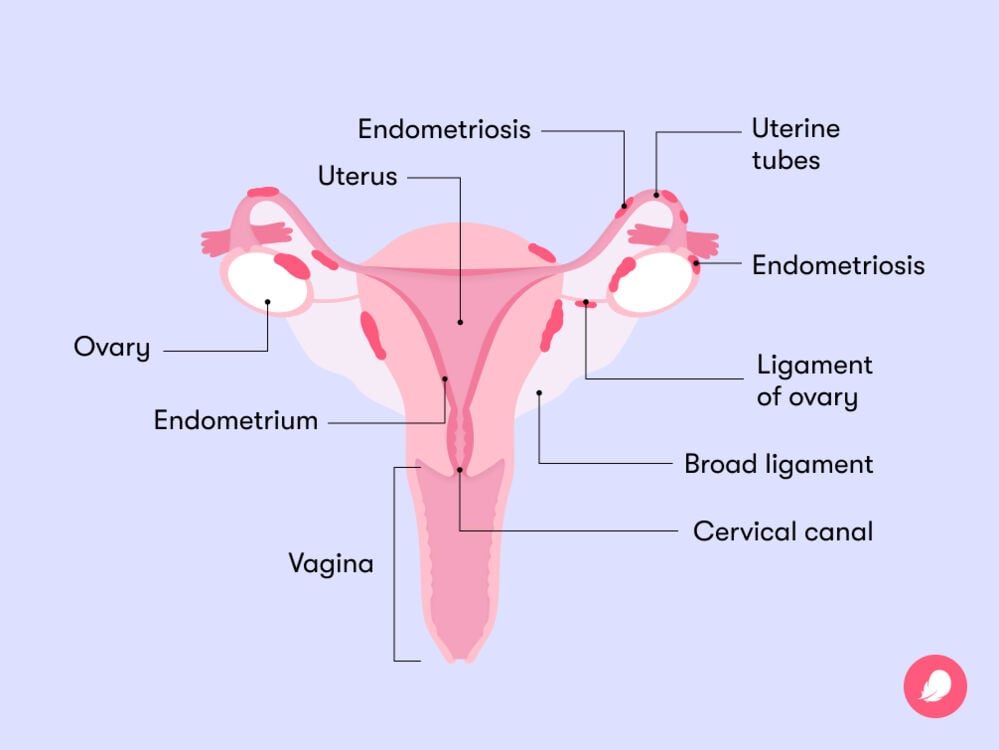
Before we get into the symptoms of endometriosis, it’s useful to understand what it actually is. Endometriosis is a chronic recurring and progressive condition where tissue similar to the lining of the uterus (called the endometrium) starts to grow in other places in the body. While this tissue tends to grow in the pelvis — typically on reproductive organs such as your ovaries and uterine (fallopian) tubes and sometimes on your bowels, bladder, and rectum — it has also been known to occasionally grow in the lungs, kidneys, and diaphragm.
You might be curious about how this excess tissue growth can cause chronic pain. The easiest way to answer this is to think about what happens during your period. The tissue that makes up the lining of your uterus builds up throughout your menstrual cycle, and when you have your period, it falls away and leaves your body through your vagina. Endometriosis tissue behaves in exactly the same way.
It builds up during your cycle because it’s hormonally sensitive, but when it’s time for the tissue to shed, it has no way of leaving your body. That means the area where the endometriosis tissue is growing can swell, causing lesions and inflammation around and inside the affected organs. That’s where much of the pain comes from. Similarly, endometriosis causes lesions in your body that produce prostaglandins (which are hormone-like substances). Prostaglandins can cause inflammation and severe pain. You can learn more about endometriosis using an app like Flo.
Take a quiz
Find out what you can do with our Health Assistant
How common is it?
Endometriosis is estimated to affect one in 10 women worldwide, but some experts believe it might actually be far more common than that. Many people have to wait years before their condition is correctly diagnosed due to the fact there isn’t a blood test or ultrasound that can diagnose it. Symptoms of endometriosis also tend to overlap with those of other conditions, such as constipation, irritable bowel syndrome, and normal cramps that people experience during their period. These similarities can mean that endometriosis is hard to spot in some cases. You can read more on this below.
Is endometriosis serious?
While it might be pretty common, endometriosis is still a serious condition that can really impact your quality of life. The chronic pain associated with it isn’t something you should just put up with and it isn’t the same as period cramps. Advocating for yourself in a medical setting can be really tiring, so if you’ve visited your doctor about your symptoms and experienced pushback, then try to be gentle with yourself. It’s absolutely not your fault and don’t be afraid to seek a second opinion. There are a number of ways you can manage your symptoms and you don’t have to stick with the first doctor you speak to.
Symptoms of endometriosis
The symptoms associated with endometriosis can vary depending on where the endometriosis is in your body. Typically, the earliest sign of the condition is painful periods. Other symptoms of endometriosis can include:
- Pain when peeing or pooping
- Heavy periods
- Vaginal bleeding when you’re not on your period
- Pelvic pain outside of menstruation
- Pain during sex
- Difficulty conceiving
It’s sometimes tricky to know whether the pain that’s associated with your menstrual cycle is normal or not because we’re so often told to expect it. However, it’s important to remember that if your typical period pain doesn’t go away with over-the-counter painkillers or if it’s preventing you from going about your daily activities or going to work or school, you should speak to your doctor. It could be a sign that you have a condition like endometriosis. You can learn more about what to expect during your period using an app like Flo.
How is endometriosis diagnosed?
As we’ve heard, endometriosis is notoriously tough to diagnose — so much so that it often takes years. On average, it takes between eight and 12 years to diagnose endometriosis. Let’s look into how a doctor would diagnose the condition and why it can take so long. Dr. Sameena Rahman, obstetrician, gynecologist, and professor at Northwestern Feinberg School of Medicine, Illinois, US, explains that your doctor may try one or more of these methods:
- A clinical checkup: Your doctor may ask about your medical history and symptoms before conducting an abdominal and/or pelvic exam. “Many of us will take into account family history and symptoms to make a clinical diagnosis and treat endometriosis based on clinical symptoms,” Dr. Rahman says.
- A scan: If your doctor thinks you may have endometriosis, they might send you for an ultrasound scan. This can be external (when your doctor looks at your pelvis through your abdomen) or transvaginal (where the scanning probe is inserted into your vagina). Sometimes, endometriosis can’t be seen using imaging techniques (like scans), so your doctor may send you for a laparoscopy instead.
- Laparoscopy: This is considered to be the gold standard and most common way of diagnosing endometriosis. A laparoscopy is keyhole surgery, so it’s minimally invasive and allows your doctor to inspect the different areas of your pelvis. Surgery might sound daunting, but the procedure is fairly quick. It involves your surgeon making a few small holes in your abdomen and inserting a small camera to see what’s going on inside of you. They may remove a sample of the area they suspect is endometriosis to be sent off to a lab to be assessed. This is called a biopsy. Keep reading to learn more about the different surgical options for endometriosis.
Endometriosis stages
When a doctor is diagnosing endometriosis, they will likely class it between stages one and four, based on a scale designed by the American Society of Reproductive Medicine. It’s important to remember that the stage of your endometriosis doesn’t describe how severe your symptoms are. You could have stage 4 endometriosis with minimal pain or stage 1 endometriosis with severe pain. It simply allows your doctor to identify where your endometriosis is growing and may be useful when they’re deciding what treatment you need. Here’s what each of the stages mean:
- Stage 1: Minimal endometriosis with a few small growths that can be found in your pelvis, abdomen, or other organs. Very little scar tissue or none at all.
- Stage 2: Mild endometriosis with slightly more growths that tend to be deeper in the tissue. A little scar tissue.
- Stage 3: Moderate endometriosis with deep growths. You may also have cysts in your ovaries and extensive scar tissue.
- Stage 4: Severe endometriosis that is widespread, resulting in multiple growths and scar tissue, as well as large cysts on your ovaries.
Endometriosis treatment
While there isn’t currently a cure for endometriosis, there are a range of treatment options that can help you manage symptoms and improve your quality of life. Before starting treatment, your doctor will consider how severe your symptoms are, whether you want to become pregnant in the future, and your overall physical health.
Hormonal therapy or treatments are often used to treat endometriosis. These can include:
- The combined pill (sometimes called the birth control pill)
- The progestin-only pill
- The intrauterine device (also known as the hormonal IUD or coil)
- Gonadotropin-releasing hormone agonists (these can be taken in the form of a shot, nasal spray, or tablet and are sometimes shortened to GnRH)
As we mentioned above, endometrial tissue is sensitive to your hormones, particularly estrogen. Using hormone treatments can slow down estrogen production, which may ease some of your symptoms. Using anti-inflammatory painkillers alongside hormone treatments could help to manage any pain you experience too.
If your endometriosis is more extensive or your symptoms are more severe, your doctor may recommend that you have surgery. There are a few different options to consider:
- Laparoscopy: As we learned above, laparoscopic or “keyhole” surgery involves your doctor making little cuts in your lower abdomen. They will then insert a small tube with a light and camera (a laparoscope) to look for endometrial tissue and potentially remove it. The tissue can be removed by burning it off (known as fulguration or ablation) or cutting it out (excision).
- Laparotomy: If any endometriosis tissue is left behind after a laparoscopy, then it’s possible that it may grow back. In this case, your doctor might recommend that you have another laparoscopy or may suggest a laparotomy. This is a slightly more complicated procedure and is used in fewer cases. It’s where your doctor will make a larger incision across your lower abdomen to remove any endometrial tissue from organs like the bladder, urinary tract, or bowel.
- Hysterectomy: A hysterectomy is when your uterus, uterine tubes, and sometimes your ovaries are removed. Your doctor will only recommend this as a treatment option if you don’t want to get pregnant in the future and you have stage 4 endometriosis. Hysterectomy is presented as a treatment option because it removes the organs that are the source of the endometriosis, reducing your chance of needing surgery again. However, many doctors use it as a last-resort option, as it’s very invasive.
It’s not always easy to know if surgery is right for you, especially if you have other treatment options. It’s really important to bear in mind that there’s no guarantee that pain relief from surgery will last forever. And like with any procedure, there’s no such thing as a one-size-fits-all solution. You can speak to your doctor to determine the ideal time to have surgery based on the state of the condition and your needs. And if you have any questions or concerns, don’t be afraid to ask your doctor.
What happens if endometriosis is left untreated?
Surgery and hormone treatment might sound a little bit daunting, but remember that there are lots of support and treatment options out there. Your doctor will be there every step of the way to talk you through your treatment options for easing your symptoms. If left untreated, endometriosis tissue can continue to grow, causing scar tissue, lesions, cysts, and adhesions. These can increase the pain you experience and cause other health complications (more on this below), so it’s best to treat and/or manage them if possible.
What causes endometriosis?
Experts have worked tirelessly over the last few decades to determine the cause of endometriosis. One of the most widely accepted explanations for endometriosis is retrograde menstruation. Sound confusing? Well, luckily, it’s actually pretty easy to explain. Retrograde menstruation is when period blood, which contains cells from your uterine lining, flows back through your uterine tubes into your pelvis, instead of leaving your body through your vagina. This can lead to endometrial cells sticking to your pelvis and other parts of your body, causing endometriosis.
Risk factors
While doctors still don’t know what causes endometriosis, there are some factors that could increase your risk of experiencing the condition. They include:
- Having a family history of endometriosis: Some researchers have linked endometriosis to genetics. If someone in your family has it, then this may increase your chances of having it, so make sure you share any information you have about your family’s medical history with your doctor.
- Starting your period early: It’s been suggested that if you have your first period before the age of 11, then you may be at a greater risk of developing endometriosis.
- Having a shorter menstrual cycle: If the length of time between your periods is shorter than 27 days, you may have an increased chance of endometriosis.
- Experiencing particularly heavy periods
- Having any conditions that prevent your period blood from leaving your body: For example, you may have a differently shaped uterus.
What causes flare-ups?
You might have heard the term “endometriosis flare-up” but aren’t totally sure what it means. “Flare-up” isn’t a medical term, but it describes a sudden worsening of symptoms. While most people with endometriosis tend to experience worse symptoms when they’re ovulating or on their period, they can occur at any time.
To figure out what’s causing your pain, it’s useful to track your cycle and see if your symptoms worsen at any particular time. You can do this using an app like Flo. It can also help to see if you experience worse symptoms after certain activities. You might find it helpful to log your endometriosis symptoms to share with your doctor.
Endometriosis complications
Due to the fact that endometriosis can cause lesions, other medical complications may follow if it’s left untreated. These can include bladder and bowel problems, meaning endometriosis can make going to the bathroom painful. It’s rare, but you may also notice blood in your pee. Complications can sound scary, and it’s totally normal to be worried about what is causing your pain. If you’re experiencing these symptoms or are worried, then you should speak to your doctor.

Can someone with endometriosis get pregnant?
If you have endometriosis and you want to get pregnant, then one of your main concerns may be how the condition could impact your fertility. Studies show that some people with endometriosis can experience difficulty getting pregnant. You might be curious as to why this is.
In some cases, endometriosis can cause damage to one or more of your reproductive organs such as your uterus, ovaries, and uterine (fallopian) tubes. The endometriosis tissue could obstruct the sperm from reaching the egg. It can also impact the number of eggs you have. This can be a hard part of an endometriosis diagnosis to take in, but try to remember that it is possible to get pregnant if you have endometriosis. In fact, it’s estimated that 50% to 70% of people with endometriosis may have no fertility issues at all, so there’s good reason to stay hopeful.
If you’re trying to conceive and have endometriosis, there’s a lot you can do to increase your chances of having a baby. If it doesn’t seem to be happening naturally, fertility specialists may be able to recommend assisted reproductive technologies to help you. For example, intrauterine insemination or in vitro fertilization (IVF) may be options to explore. IVF outcomes are positive for endometriosis. One study found that after one to four IVF treatments including frozen embryo transfer, almost 70% of women with stage one or two endometriosis were pregnant. In the same study, more than half of women with stage three and four endometriosis were pregnant (compared to around 80% of women without endometriosis).
It’s important to acknowledge that there can be a number of barriers to fertility treatment, including how much it can cost. So make sure you speak to your doctor about what may be accessible to you.
Endometriosis: The takeaway
Although diagnosis can take a long time and may be a complicated process, it’s worth pursuing, because finding out whether or not you have endometriosis can help you to get the answers you need. Logging your endometriosis symptoms and tracking your cycle using an app like Flo may help you understand some of the triggers for your symptoms while you’re waiting and after being diagnosed.
Once you have a diagnosis, your doctor will work closely with you to identify the most effective form of treatment. Endometriosis often affects everyone differently, so it’s really important that you take some time to figure out what might be the best next step for you.
Living with endometriosis can be challenging, but it doesn’t mean you have to lose out on your quality of life. Along with your medical team, family, friends, and the rest of the endometriosis community, you can find a way to regain control of your body. Remember, a problem shared is a problem halved.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Bulletti, Carlo, et al. “Endometriosis and Infertility.” Journal of Assisted Reproduction and Genetics, vol. 27, no. 8, Aug. 2010, pp. 441–47.
“Common Triggers of an Endometriosis Flare-Up.” Holtorf Medical Group, 4 Mar. 2022, holtorfmed.com/articles/womens-health/common-triggers-of-an-endometriosis-flare-up.
“Endometriosis.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/10857-endometriosis. Accessed 6 Mar. 2023.
“Endometriosis.” Yale Medicine, 11 Aug. 2022, www.yalemedicine.org/conditions/endometriosis.
“Endometriosis.” Mayo Clinic, 24 July 2018, www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656.
“Endometriosis.” The American College of Obstetricians and Gynecologists, www.acog.org/womens-health/faqs/endometriosis. Accessed 6 Mar. 2023.
“Endometriosis.” NHS, www.nhs.uk/conditions/endometriosis/. Accessed 6 Mar. 2023.
“Endometriosis.” World Health Organization, www.who.int/news-room/fact-sheets/detail/endometriosis. Accessed 6 Mar. 2023.
“Endometriosis Surgery.” Cleveland Clinic, my.clevelandclinic.org/health/treatments/4620-endometriosis-surgery. Accessed 6 Mar. 2023.
“Endometriosis Treatment & Management.” Medscape, 25 Jan. 2022, emedicine.medscape.com/article/271899-treatment.
“Heavy Periods.” NHS, www.nhs.uk/conditions/heavy-periods/. Accessed 6 Mar. 2023.
“Why It’s Necessary: Hysterectomy.” NHS, www.nhs.uk/conditions/hysterectomy/why-its-done/. Accessed 6 Mar. 2023.
Johnson, Neil P., et al. “World Endometriosis Society Consensus on the Classification of Endometriosis.” Human Reproduction, vol. 32, no. 2, Feb. 2017, pp. 315–24.
Kuivasaari, Paula, et al. “Effect of Endometriosis on IVF/ICSI Outcome: Stage III/IV Endometriosis Worsens Cumulative Pregnancy and Live-Born Rates.” Human Reproduction, vol. 20, no. 11, Nov. 2005, pp. 3130–35.
“Laparoscopy (Keyhole Surgery).” NHS, www.nhs.uk/conditions/laparoscopy/. Accessed 6 Mar. 2023.
“Endometriosis: Diagnosis and Management.” National Institute for Health and Care Excellence, www.nice.org.uk/guidance/ng73/chapter/Recommendations. Accessed 6 Mar. 2023.
Tanbo, Tom, and Peter Fedorcsak. “Endometriosis-Associated Infertility: Aspects of Pathophysiological Mechanisms and Treatment Options.” Acta Obstetricia et Gynecologica Scandinavica, vol. 96, no. 6, June 2017, pp. 659–67.




