Find out what might be causing that burning sensation in your mouth, feet, vagina, or skin — and find out how to help relieve it.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Can menopause cause a burning sensation in your body?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Have you noticed an unusual burning sensation lately, but you’re not sure what could be causing it? Perhaps it burns when you pee, or your vagina feels curiously hot all of a sudden. Maybe your mouth is on fire, or your hands and feet feel tingly.
Menopause might be the last thing that springs to mind. But if you’re somewhere between your late 30s and your 50s and your menstrual cycle has started to change, it could suggest that menopause is on the way. This is especially likely if you’ve noticed other telltale symptoms such as mood swings or brain fog.
Experiencing any type of burning sensation can be uncomfortable and maybe even a little alarming if you don’t know what’s causing it. But once you figure out the cause, with the right treatment, it can be manageable. If it turns out to be a signal you’re in the lead-up to menopause (known as perimenopause), remember that there are lots of treatment options depending on your symptoms, so reach out to your doctor for advice.
Perimenopause aside, a burning feeling under the skin may be caused by any number of things, from an insect bite to shingles. Feeling burning in the vulva or vagina might suggest you’ve got an infection, so the best thing to do in any case is to see your health care provider, who can help you find the cause.
If you are on the journey to menopause, read on as Dr. Allison K. Rodgers, reproductive endocrinologist, obstetrician, and gynecologist from Illinois, US, shares everything you need to know. From why a burning sensation can happen at this stage of life to how to deal with it, find out all about one of the lesser-known perimenopause symptoms.
Key takeaways
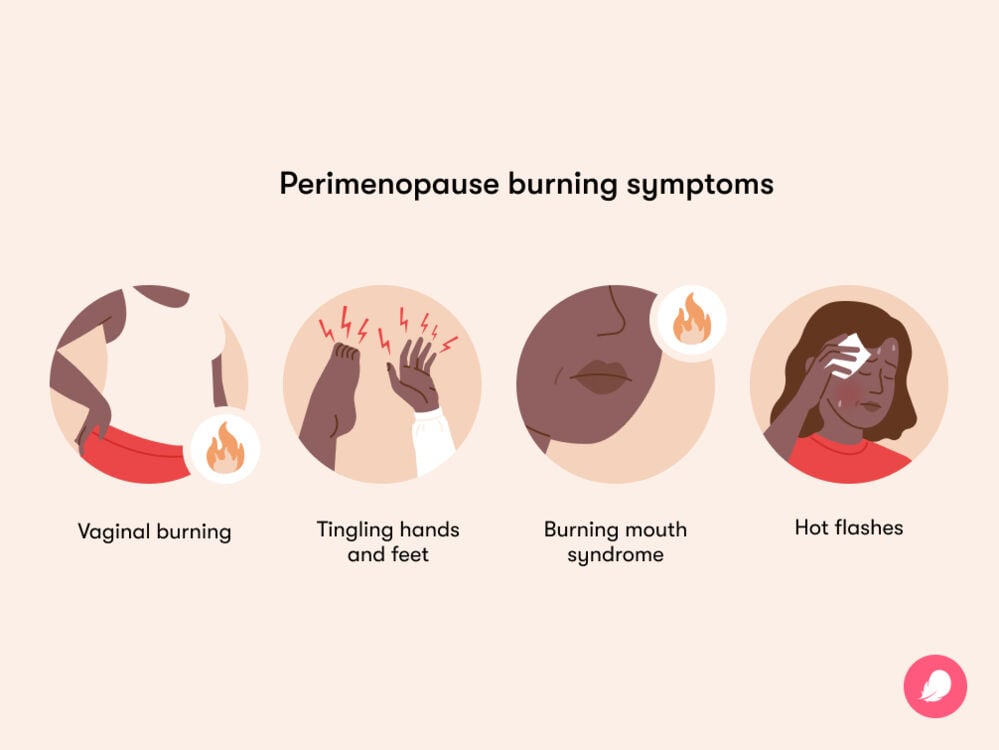
- Some women and people with periods notice burning sensations in their vagina, their mouth, or their skin, hands, or feet around the time of menopause.
- Falling levels of the hormone estrogen — which is what happens during the run-up to menopause — are thought to be the main cause of burning, tingling, and unusual skin sensations, says Dr. Rodgers.
- Hormone therapy (HT, previously called hormone replacement therapy or HRT) may be offered to help treat the most common menopausal symptoms. While research is limited to say whether HT could ease burning sensations linked to perimenopause or menopause, it may help some people.
Can menopause cause a burning sensation in my body?
You’re probably familiar with the term menopause, but the symptoms linked to it can start earlier than you think, during what’s called perimenopause. The terms perimenopause and menopause are often used interchangeably, but they’re two separate things.
Perimenopause is the phase leading up to menopause (the official name for your final period), plus one year after. Perimenopause usually begins somewhere between your late 30s and 50s — but most often in your 40s. Then, when you haven’t had a period for 12 months (this happens most commonly between the ages of 45 and 55), you’re classed as having gone through menopause. From that point on, you are postmenopausal.
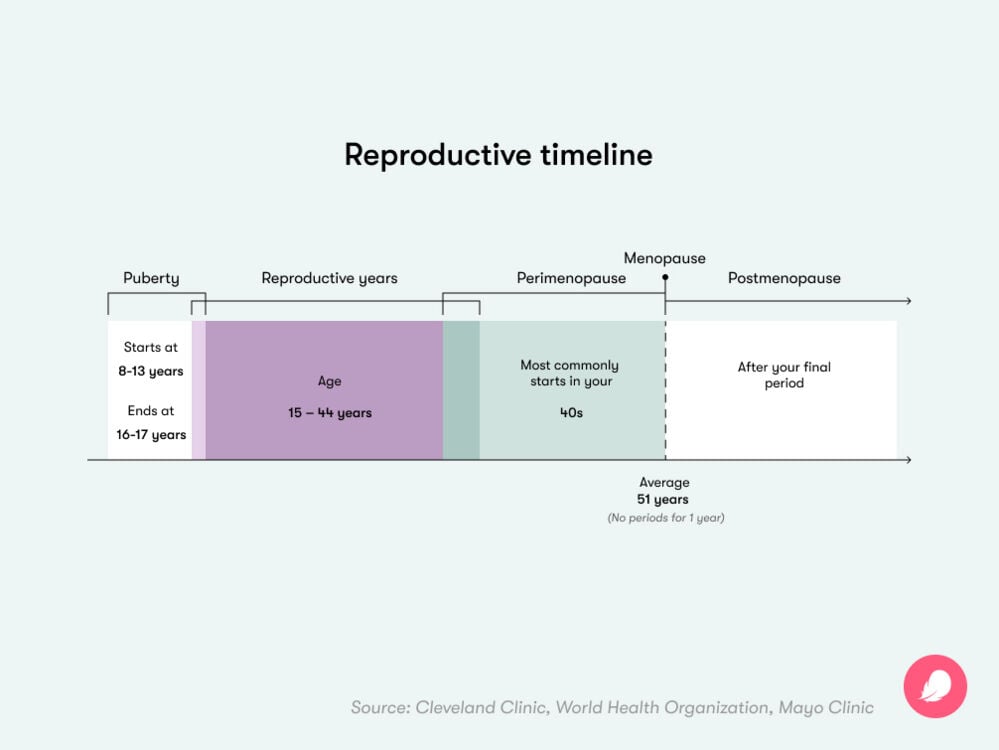
Menopause is a process that everyone who’s born with a female reproductive system will go through. Perimenopause can often signal the start of new symptoms such as hot flashes, sleepless nights, and more. These differ for everyone — some people might not notice many symptoms at all, while others might feel them more intensely.
A burning sensation in one or more areas of your body is a possible sign of perimenopause. “Most symptoms of menopausal-related burning are in the vagina, vulva, and bladder/urethra,” says Dr. Rodgers. But other people “may notice dryness of their skin and mouth and [more] rarely will have numbness, tingling, or burning in their hands and feet,” she adds.
Experts aren’t completely sure why some women experience a burning sensation in the run-up to menopause, so more research is needed. But just like other, more widely known perimenopause symptoms such as brain fog, headaches, and hot flashes, it’s believed to be caused by changing hormones.
Estrogen is a hormone that plays an important role in lots of your body’s functions. To make this happen, you have estrogen receptors in different parts of the body. When estrogen levels go up and down during perimenopause before eventually reducing for good, this can affect you in lots of different ways due to all those estrogen receptors. One thing that can happen is that your vaginal lining or your skin may become dehydrated and less elastic, which can trigger unusual sensations such as a burning feeling in your vagina, mouth, or your hands and feet.
Vaginal burning
You may already be aware of one thing that can happen during perimenopause: vaginal dryness. This is a symptom of a medical condition called vaginal atrophy — when your vaginal walls start to become thinner and dryer — and it can cause a feeling like burning or itching.
“People can feel a dry, tight, painful burning sensation in their vagina, caused by the drop in estrogen,” explains Dr. Rodgers. Having less estrogen can also make your vaginal canal narrower, which may add to your discomfort. “This is caused by reduced blood flow to the vagina and the loss of vaginal folds,” Dr. Rodgers adds.
Vaginal burning can be uncomfortable and may make your day-to-day and your sex life difficult. But your doctor may be able to help, so schedule an appointment with them.
Burning mouth syndrome
If you experience scalding, tingling, or even a bitter and metallic taste on your tongue, you may have burning mouth syndrome, which is a lesser-known condition that peaks during perimenopause.
“Dry mouth can be a really irritating perimenopausal symptom,” says Dr. Rodgers. And similar to vaginal burning, the cause is also likely hormone related. “Since estrogen also keeps the mucosal membranes [the moist lining] in our mouths healthy, the drop in estrogen during menopause can cause dryness of this as well,” she adds.
If your dry or burning mouth starts happening regularly enough to bother you, make an appointment with your doctor. It may be triggered by something else, like acid reflux, an allergy, or certain medicines. But if they find that perimenopause is the cause, and you’ve also got other symptoms (like hot flashes), hormone therapy may be suggested. You might find it helps with a burning mouth, but keep in mind that it’s not guaranteed to work in this way, as one study points out.
Tingling hands and feet
A perimenopause symptom that’s rarely talked about is tingling in your hands, feet, or elsewhere — also known as paresthesia. If you notice an unusual sensation anywhere in your body that feels a bit like pins and needles, or if your arms and legs start tingling or become numb and itchy, there’s a chance perimenopause could be the cause. Of course, it’s still important to get checked by the doctor to rule out any other cause.
One study suggests that just over 30% of perimenopausal women may notice paresthesia, although more research is needed. “This symptom of [peri]menopause is not well understood,” says Dr. Rodgers.
Just like other common symptoms during the menopause transition, these tingling sensations are thought to happen because low estrogen levels “cause changes to the peripheral nerves,” she explains. In some cases, tingling in the hands and feet can happen as a result of low vitamin B12 levels. Any type of nerve sensation can be unsettling, but there may be things you can do to ease any discomfort. Your doctor will be able to share some advice that’s relevant to you.
Take a quiz
Find out what you can do with our Health Assistant
Hot flashes
If you notice a burning sensation that feels like heat creeping through your chest, neck, and face, and you are perimenopausal, then it is most likely a hot flash. This common perimenopause symptom affects more than 80% of women. And if you get hot flashes at night, they’re called night sweats.
Also known as “vasomotor symptoms,” hot flashes can be uncomfortable and may keep you up at night. In this case, “temperature regulation can help,” Dr. Rodgers says, so dress in layers that can easily be removed if a hot flash comes on, invest in a fan to help you keep cool, and try to limit alcohol. If none of this helps, speak to your doctor, as treatment options are available.
Dry or itchy skin
Estrogen is closely linked to skin hydration, so lower levels of the hormone can cause your skin to become less elastic and dehydrated. This can make you feel dry and sometimes itchy. A drop in estrogen also means less collagen is produced, which can leave the skin feeling less supple. Lower collagen can also sometimes result in a tingling sensation or the feeling of something crawling on the skin (known as formications), although this is more common in postmenopausal people.
How can I relieve menopause-related burning sensations?
If you’re finding your perimenopause symptoms tricky to handle, chatting with people in a similar situation may make you feel less alone. You can do exactly that in Flo’s safe community space, Secret Chats. Download our cycle-tracking app to get involved in these conversations, as well as keep a log of your cycles, note your symptoms, and more.
Like any new and persistent symptom, the best thing to do is always get it checked by a doctor so they can try to find the cause. If it turns out to be menopause related, there are a few different treatment options they might suggest, but these can differ depending on what kind of burning sensation you’re experiencing.
You can read on to find out more about the specific treatment options for vaginal burning, burning mouth syndrome, tingling hands and feet, hot flashes, and dry or itchy skin. But one thing that may be suggested for all perimenopausal symptoms is to make some lifestyle changes.
Doing your best to lead a healthy lifestyle is always a good idea around the time of menopause, regardless of your specific symptoms. Your doctor may suggest you aim to reduce stress, exercise regularly, and improve your diet if possible. Foods that are low in fat and high in fiber, like whole grains and lentils, as well as fruits and leafy green vegetables, are ideal. These contain essential vitamins and minerals and will hopefully help to make you feel good. Dr. Rodgers adds that “cutting out caffeine, alcohol, nicotine, and cannabis” may also help.
Treatment for vaginal burning
“Using a vaginal lubricant or a vaginal moisturizer can be helpful,” says Dr. Rodgers. Beyond that, a treatment that can be offered is hormone therapy. HT increases low estrogen levels and “reverses many of the menopausal changes that cause symptoms of vaginal burning,” explains Dr. Rodgers. HT is typically given by pills, vaginal rings, inserts, or skin patches.
There are two other hormonal treatment options that can help tackle vaginal burning. One is vaginal estrogen therapy, which is more localized than HT because it’s only used in the vagina rather than the whole body. This can either be applied as a cream or inserted as a suppository or a ring inside your vagina. The other is called intravaginal dehydroepiandrosterone (more commonly known as DHEA), which works by making the vaginal wall thicker and more moist. Both of these changes could help to ease the feeling of burning.
Treatment for burning mouth syndrome
There are a few things your health care provider might suggest trying if you’ve got a burning mouth. Certain medications, such as ones to block nerve pain, others used for seizures, or antidepressants, may help. Prescribed mouth rinses may also be an option, and “staying hydrated [and] sucking on ice, mints, or gum can often help this feeling,” says Dr. Rodgers.
If the problem is ongoing, you may want to consider trying something different. Research suggests that a type of talking therapy known as cognitive behavioral therapy (CBT) could help those with burning mouth syndrome symptoms, so this could be something to explore.
Hormone therapy is unlikely to be prescribed for burning mouth syndrome alone. But if you have other perimenopause symptoms, your doctor may suggest it, and you may find it helps relieve your burning mouth at the same time. As with many things, there are pros and cons of hormone therapy. It’s right for some people and less so for others. Chat with your doctor about it, and they can help you decide whether it’s the right option for you.
Treatment for tingling hands or feet
The best thing to do is ask your doctor about how best to tackle your paresthesia. Some people see an improvement in symptoms with exercise, so try to make time for some movement if you’re able to. If it’s being caused in part by low vitamin B12, speak to your doctor about what they would advise. You could also try upping your levels with foods that are naturally rich in the vitamin, such as meat, fish, milk, cheese, and cereals.
While hormone therapy isn’t usually offered for paresthesia, if you have other perimenopause symptoms like hot flashes, your doctor may suggest you try it. There’s a chance that increasing your estrogen levels in this way may help to reduce tingling sensations at the same time.
Cognitive behavioral therapy may also be something to explore. Although you might not imagine talk therapy could be useful for a physical sensation, it has been shown to help some people.
Treatment for hot flashes
While hormone therapy is often the go-to treatment for certain perimenopause symptoms like hot flashes, it might not be something you can — or want — to use. If you’re already using combined hormonal contraceptive pills, then your doctor might suggest you keep taking them in the early stages of perimenopause. They may help ease hot flashes as well as regulate unpredictable cycles — another common symptom of perimenopause. Contraceptive pills work by steadying your changing hormone levels, which means they can be helpful during perimenopause.
“There are some nonhormonal options to help with symptoms as well,” says Dr. Rodgers. Some selective serotonin reuptake inhibitors, which are otherwise typically taken to help mood disorders, may be one option. Others include a seizure medication called gabapentin, a hay fever medication called fezolinetant, and an overactive bladder medication called oxybutynin. As with any type of medicine, they may come with side effects, so it’s important to discuss your options with a doctor so you know what to expect.
Treatment for dry or itchy skin
When your estrogen levels drop during perimenopause, it can make you less thirsty, meaning you drink less and risk becoming dehydrated — which can affect your skin. Further research is needed to understand the link between hydration and dry skin conditions, but drinking plenty of water is always a good idea to improve your health. Don’t forget that you can consume more fluids by both eating and drinking. Aim to take in the recommended daily amount — which is about 11.5 cups or 2.7 liters — even if you don’t feel thirsty. You can also keep your skin in good health generally during perimenopause and beyond by eating a balanced diet and avoiding smoking.
For crawling sensations on your skin, there’s no one-size-fits-all approach to stopping them, but you might notice that these start to ease if you take treatments (like HT, for example) for other perimenopause symptoms.
More FAQs
How do I know what stage of perimenopause I am in?
Your cycle length can be a good way to tell what stage of perimenopause you’re in. One of the first signs of perimenopause can be your cycles getting longer or shorter as your hormones start fluctuating. If you notice a regular change of seven days or more in your menstrual cycle length, you may well be in the early stages of perimenopause. If you go for 60 days or more without a period and you’ve also been having other symptoms like hot flashes and mood swings, you’re probably in late perimenopause. But everyone is different, so speak to your doctor to get more personalized advice.
What’s the most commonly reported symptom of menopause?
Hot flashes are the most common symptom of menopause, with up to 80% of women noticing some level of sudden intense heat during perimenopause. Usually, it happens in your upper body, around your face, neck, and chest. There are plenty of options for treatment, though, so reach out to your doctor if it’s interfering with your day-to-day life.
What’s the average age for menopause to end?
Most women will have their last period at around the age of 51, although anywhere between the ages of 45 and 55 is considered normal. After 12 months without a period, menopause is confirmed, and from then on, you are classed as postmenopausal.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
Abraham, Cynthia. “Experiencing Vaginal Dryness? Here’s What You Need to Know.” The American College of Obstetricians and Gynecologists, Oct. 2020, www.acog.org/womens-health/experts-and-stories/the-latest/experiencing-vaginal-dryness-heres-what-you-need-to-know.
Akdeniz, M., et al. “Does Dietary Fluid Intake Affect Skin Hydration in Healthy Humans? A Systematic Literature Review.” Skin Research and Technology, vol. 24, no. 3, Aug. 2018, pp. 459–65, doi: 10.1111/srt.12454.
American Menopause Society.” Menopause, vol. 30, no. 6, June 2023, pp. 573–90, doi: 10.1097/GME.0000000000002200.
“Burning Mouth Syndrome.” Mayo Clinic, 22 Feb. 2023, www.mayoclinic.org/diseases-conditions/burning-mouth-syndrome/symptoms-causes/syc-20350911.
Canário, Ana C. G., et al. “The Impact of Physical Activity on Menopausal Symptoms in Middle-Aged Women.” International Journal of Gynecology and Obstetrics, vol. 118, no. 1, July 2012, pp. 34–36, https://doi.org/10.1016/j.ijgo.2012.02.016.
“Changes in the Vagina and Vulva.” The North American Menopause Society, www.menopause.org/for-women/sexual-health-menopause-online/changes-at-midlife/changes-in-the-vagina-and-vulva. Accessed 3 July 2024.
“Combination Birth Control Pills.” Mayo Clinic, 13 Jan. 2023, www.mayoclinic.org/tests-procedures/combination-birth-control-pills/about/pac-20385282..
Dahiya, Parveen, et al. “Burning Mouth Syndrome and Menopause.” International Journal of Preventive Medicine, vol. 4, no. 1, Jan. 2013, pp. 15–20, www.ncbi.nlm.nih.gov/pmc/articles/PMC3570906/.
“Estrogen.” Cleveland Clinic, my.clevelandclinic.org/health/body/22353-estrogen. Accessed 20 July 2022.
“Formication.” Cleveland Clinic, my.clevelandclinic.org/health/symptoms/23960-tactile-hallucinations-formication. Accessed 3 July 2024.
Grandi, Giovanni, et al. “Contraception during Perimenopause: Practical Guidance.” International Journal of Women’s Health, vol. 14, July 2022, pp. 913–29, doi:10.2147/IJWH.S288070.
“Here’s How Menopause Affects Your Skin and Hair.” Cleveland Clinic, 19 Feb. 2021, health.clevelandclinic.org/heres-how-menopause-affects-your-skin-and-hair.
“Hormone Therapy for Menopause.” The American College of Obstetricians and Gynecologists, Oct. 2021, www.acog.org/womens-health/faqs/hormone-therapy-for-menopause.
“Hormone Therapy: Is It Right for You?” Mayo Clinic, 6 Dec. 2022, www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372.
“Hot Flashes.” Mayo Clinic, 12 Dec. 2023, www.mayoclinic.org/diseases-conditions/hot-flashes/diagnosis-treatment/drc-20352795.
“Hot Flashes: What Can I Do?” National Institute on Aging, www.nia.nih.gov/health/menopause/hot-flashes-what-can-i-do. Accessed 3 July 2024.
“How Do Healthcare Providers Diagnose Menopause?” Eunice Kennedy Shriver National Institute of Child Health and Human Development, www.nichd.nih.gov/health/topics/menopause/conditioninfo/diagnosed. Accessed 3 July 2024.
Labrie, Fernand, et al. “Efficacy of Intravaginal Dehydroepiandrosterone (DHEA) on Moderate to Severe Dyspareunia and Vaginal Dryness, Symptoms of Vulvovaginal Atrophy, and of the Genitourinary Syndrome of Menopause.” Menopause, vol. 23, no. 3, Mar. 2016, pp. 243–56, doi: 10.1097/GME.0000000000000571.
Lephart, Edwin D., and Frederick Naftolin. “Menopause and the Skin: Old Favorites and New Innovations in Cosmeceuticals for Estrogen-Deficient Skin.” Dermatology and Therapy, vol. 11, no. 1, Feb. 2021, pp. 53–69, doi: 10.1007/s13555-020-00468-7.
“Menopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401.
“Menopause.” World Health Organization, 17 Oct. 2022, www.who.int/news-room/fact-sheets/detail/menopause.
“Menopause 101: A Primer for the Perimenopausal.” The North American Menopause Society, www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal. Accessed 11 June 2024.
“Menopause Numbness and Tingling.” Positive Pause, www.positivepause.co.uk/physical-symptoms-menopause/numbness-tingling. Accessed 3 July 2024.
Mollaahmadi, Leila, et al. “Evaluation and Comparison of the Effects of Various Cognitive-Behavioral Therapy Methods on Climacteric Symptoms: A Systematic Review Study.” Journal of the Turkish German Gynecological Association, vol. 20, no. 3, Sep. 2019, pp. 178–95, doi:10.4274/jtgga.galenos.2019.2018.0170.
Nappi, Rossella E., et al. “Global Cross-Sectional Survey of Women with Vasomotor Symptoms Associated with Menopause: Prevalence and Quality of Life Burden.” Menopause, vol. 28, no. 8, Aug. 2021, pp. 875–82, DOI: 10.1097/GME.0000000000001793.
“Paresthesia.” Cleveland Clinic, my.clevelandclinic.org/health/symptoms/24932-paresthesia. Accessed 3 July 2024.
“Perimenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21608-perimenopause. Accessed 2 Apr. 2024.
Pięta, Wojciech, and Roman Smolarczyk. “Vaginal Dehydroepiandrosterone Compared to Other Methods of Treating Vaginal and Vulvar Atrophy Associated with Menopause.” Przeglad Menopauzalny [Menopause Review], vol. 19, no. 4, Dec. 2020, pp. 195–99, doi: 10.5114/pm.2020.101943.
Pinkerton, Joann V. “Menopause.” MSD Manual Consumer Version, July 2023, www.msdmanuals.com/en-gb/home/women-s-health-issues/menopause/menopause.
Priyanka, Hannah P., and Rahul S. Nair. “Neuroimmunomodulation by Estrogen in Health and Disease.” AIMS Neuroscience, vol. 7, no. 4, Oct. 2020, pp. 401–17, doi:10.3934/Neuroscience.2020025.
Rzepecki, Alexandra K., et al. “Estrogen-Deficient Skin: The Role of Topical Therapy.” International Journal of Women’s Dermatology, vol. 5, no. 2, June 2019, pp. 85–90, doi:10.1016/j.ijwd.2019.01.001.
Salamon, Maureen. “Menopause and Brain Fog: What’s the Link?” Harvard Health Publishing, 1 June 2022, www.health.harvard.edu/womens-health/menopause-and-brain-fog-whats-the-link.
Schilling, Chrissy, et al. “Current Alcohol Use, Hormone Levels, and Hot Flashes in Midlife Women.” Fertility and Sterility, vol. 87, no. 6, June 2007, pp. 1483–86, https://doi.org/10.1016/j.fertnstert.2006.11.033.
“Selective Serotonin Reuptake Inhibitors (SSRIs).” Mayo Clinic, 17 Sep. 2019, www.mayoclinic.org/diseases-conditions/depression/in-depth/ssris/art-20044825.
Shim, Youngjoo. “Treatment for Burning Mouth Syndrome: A Clinical Review.” Journal of Oral Medicine and Pain, vol. 48, no. 1, Mar. 2023, pp. 11–15, https://doi.org/10.14476/jomp.2023.48.1.11.
“Shingles.” Mayo Clinic, 20 Aug. 2022, www.mayoclinic.org/diseases-conditions/shingles/symptoms-causes/syc-20353054.
Simon, James A., et al. “Extended-Release Oxybutynin Therapy for Vasomotor Symptoms in Women: A Randomized Clinical Trial.” Menopause, vol. 23, no. 11, Nov. 2016, pp. 1214–21, doi: 10.1097/GME.0000000000000773.
“Skin Care and Aging.” National Institute on Aging, www.nia.nih.gov/health/skin-care/skin-care-and-aging. Accessed 3 July 2024.
“Staying Healthy at Menopause and Beyond.” The North American Menopause Society, www.menopause.org/for-women/menopauseflashes/women’s-health-and-menopause/staying-healthy-at-menopause-and-beyond. Accessed 3 July 2024.
“The 2023 Nonhormone Therapy Position Statement of The North American Menopause Society” Advisory Panel. “The 2023 Nonhormone Therapy Position Statement of The North American Menopause Society.” Menopause, vol. 30, no. 6, June 2023, pp. 573–590, DOI: 10.1097/GME.0000000000002200.
“Vaginal Atrophy.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/15500-vaginal-atrophy. Accessed 3 July 2024.
“Vaginal Atrophy.” Mayo Clinic, 17 Sep. 2021, www.mayoclinic.org/diseases-conditions/vaginal-atrophy/diagnosis-treatment/drc-20352294.
Vaidya, Rama. “Burning Mouth Syndrome at Menopause: Elusive Etiology.” Journal of Mid-Life Health, vol. 3, no. 1, Jan. 2012, pp. 3–4, doi:10.4103/0976-7800.98809.
“Vitamin B12 Deficiency Can Be Sneaky and Harmful.” Harvard Health Publishing, 23 Mar. 2022, www.health.harvard.edu/blog/vitamin-b12-deficiency-can-be-sneaky-harmful-201301105780.
Wang, Xueyin, et al. “Prevalence and Risk Factors for Menopausal Symptoms in Middle-Aged Chinese Women: A Community-Based Cross-Sectional Study.” Menopause, vol. 28, no. 11, Aug. 2021, pp. 1271–78, doi: 10.1097/GME.0000000000001850.
“Water: How Much Should You Drink Every Day?” Mayo Clinic, 12 Oct. 2022, www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256.
“What Can I Do to Help with Hot Flashes?” The American College of Obstetricians and Gynecologists, Aug. 2023, www.acog.org/womens-health/experts-and-stories/ask-acog/what-can-i-do-to-help-with-hot-flashes.
History of updates
Current version (16 July 2024)
Published (16 July 2024)
In this article

Track your perimenopause journey in the Flo app
-
Log symptoms and get tips to manage them
-
Learn what to expect with expert-led articles and videos
-
Connect with others who can relate to how you're feeling




