Sex shouldn’t hurt during perimenopause, postmenopause, or at any point in your life. Here’s what to do if it’s affecting you.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Painful sex after menopause: Why it hurts and what you can do


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
It’s no secret that menopause involves a host of physical changes that can have a huge impact on your everyday life. Not everyone struggles, but for some people, symptoms such as mood swings, hot flashes, and brain fog can be difficult to live with. So, if you’ve already gone through menopause, it might feel like a relief to be on the other side.
Frustratingly, reaching menopause doesn’t always signal the end of all your symptoms. Some people, for example, find penetrative sex painful in the postmenopause phase of life, which can leave you feeling a little disheartened. For many of us, sex is an important part of life that helps us to release stress and bond with our partners. If sex starts to hurt, it can lead to insecurity, loss of intimacy, and in some cases, even a reduced quality of life.
If your sex life has been affected by menopause, it may help to know that you’re not alone. In the lead-up to menopause, 15% of women will experience changes to the lining of their vagina, known as vaginal atrophy. Even more postmenopausal women — over half — notice these changes. Symptoms include bleeding after sex, burning, itching, and painful sex, also called dyspareunia. But don’t lose hope. With the right treatment, painful sex after menopause is manageable, and you don’t have to put up with it.
Of course, it’s always possible that you might be finding sex uncomfortable for reasons other than menopause, such as vaginismus, a yeast infection, or a sexually transmitted infection. Here, Dr. Brandye Wilson-Manigat, obstetrician, gynecologist, and CEO of Brio Virtual Gynecology, California, US, shares everything you need to know about painful sex after menopause. But if you have any questions or concerns about your sexual health at any stage of life, always speak to a doctor.
Key takeaways
- Almost three-quarters of women experience pain during sex at some time during their lives, and up to 45% of women report painful sex after menopause.
- Hormonal changes are believed to contribute to vaginal dryness and discomfort from sex.
- Hormone therapy (also known as hormone replacement therapy or HRT) has been found to ease painful sex symptoms for many people if a drop in hormones is the cause.
- Simple additions to your routine, including using lube and vaginal moisturizer, can help to ease pain and dryness.
- Left unchecked, painful sex often gets worse, so don’t delay speaking to your doctor about treatment options.
Is it normal to experience painful sex after menopause?
Painful sex can happen at any life stage but — because of declining hormone levels — it often spikes during perimenopause and after menopause.
As a reminder, perimenopause and menopause are two separate things. Perimenopause refers to the years leading up to when menopause (your final period) is confirmed. It usually begins somewhere between your late 30s and 50s — most often in your 40s. You’re diagnosed as having gone through menopause when you haven’t had a period for 12 months (usually between the ages of 45 and 55). From then on, you are postmenopausal.
If you’re struggling with perimenopause symptoms — whether it’s painful sex or anything else — support from like-minded people can really help. Flo’s safe community space, Secret Chats, enables you to chat about your experiences with other people who know what it’s like. Download the app to get involved in these helpful conversations, keep a note of your symptoms, and more.
Painful sex during perimenopause or after menopause is usually “persistent or recurrent pain or discomfort that occurs during or as a result of intercourse,” explains Dr. Wilson-Manigat. The pain can be “localized externally to the vulva or internally to the vagina, pelvis, or lower abdomen,” she adds.
Menopause might impact the way you feel about sex and your body, but it’s important to remember that it is still possible to enjoy a pleasurable sex life as you approach the end of your periods and postmenopause. So, if penetrative sex is important to you and something you want to keep doing, make an appointment to see your doctor. Treatment options are available, and you don’t have to live with the pain.
What causes painful sex after menopause?
Just like other, more widely known perimenopause symptoms such as hot flashes and brain fog, painful sex is largely related to a drop in hormones. That’s because in perimenopause, your estrogen levels start to change and eventually reduce.
Estrogen plays a vital role in keeping your vaginal walls elastic and moist. When your estrogen levels decline during perimenopause and postmenopause, you might lose this elasticity, and the lining of your vagina might get drier, making tearing or bleeding more likely. “The tissues become thinner and less able to stretch,” explains Dr. Wilson-Manigat. “The vaginal canal shortens and narrows. Blood flow to the genital tissues can also decrease, leaving you drier during sex.”
The result of all this? Sex might feel uncomfortable. “Depending on the area of the pain, it may feel like tearing, burning, friction, or a rubbing sensation, or like pressure or aching,” Dr. Wilson-Manigat adds. Hormonal changes can also impact pH (which in turn can affect acidity levels) in your vagina, which can lead to recurrent urinary tract infections in some people, causing further discomfort.
If you experience any type of chronic pain during or after sex, don’t shrug it off. Left untreated, it often gets worse. “Unlike other symptoms of menopause like hot flashes/night sweats, which diminish over time, painful sex due to menopausal changes does not go away,” advises Dr. Wilson-Manigat. “Without treatment, the symptoms will worsen over time.” That’s not to say your sex life is doomed from the moment you become menopausal. There are things you can include in your everyday routine that may help.
8 ways to manage painful sex after menopause
Menopause is a process that anyone born with a female reproductive system will go through. But if it’s causing you pain, don’t feel like you have to live with it.
Everyone is unique, and no two people have the exact same symptoms, so there isn’t a one-size-fits-all approach to managing painful sex after menopause. To get started, you might need to experiment with different treatment options until you find the one that works for you.
Speak to your doctor
Asking your doctor for help figuring out the underlying cause of painful sex is the first step to getting it resolved. “Sex should not be painful,” says Dr. Wilson-Manigat. “There are many potential causes and treatments available, so if you are having pain, you should see your doctor.” They will be able to help you figure out what’s going on or refer you to a specialist if necessary.
And if you feel awkward or embarrassed about discussing this intimate topic, that’s totally understandable. But it can help to remember that your doctor has had similar conversations with countless other patients before, so there’s likely to be very little that could faze them.
Try vaginal moisturizers
Just like the skin on your face and body, if your vagina feels dry, then applying a few drops of vaginal moisturizing cream might help to rejuvenate the area. Hyaluronic acid-based moisturizers have been shown to work particularly well. “Vaginal lubricants and moisturizers are first-line treatments for those experiencing painful sex due to menopause,” says Dr. Wilson-Manigat. “Vaginal moisturizers are used regularly over time and provide a protective layer to the vaginal tissues, helping to minimize discomfort.”

Take a quiz
Find out what you can do with our Health Assistant
Use lube during sex
For many people, sex is painful because they have less natural lubrication than before. If this is the case, taking plenty of time to build arousal and applying a pea-sized blob of lube before you get started might be enough. “Vaginal lubricants work by reducing friction during penetrative intercourse, minimizing pain and discomfort,” says Dr. Wilson-Manigat.
Lube generally comes in four types: water-based, silicone-based, oil-based, and hybrid. Generally, silicone-based lubes are recommended for postmenopausal vaginal dryness over water-based ones. That’s because water-based lubes are thought to change the microbiome in your vagina, which may cause problems at this stage of life.
Medical treatments for vaginal dryness
Your doctor might also recommend the following:
- Estrogen therapy: If regularly using lube and a vaginal moisturizer isn’t doing the trick, talk to your doctor about hormone therapy, says Dr. Wilson-Manigat. “In some cases, both may be needed for complete relief of symptoms,” she explains.
- Intravaginal dehydroepiandrosterone (DHEA): Another type of hormonal therapy, this works by “increasing vaginal wall thickness, vaginal secretions, and the integrity of the vaginal tissues,” says Dr. Wilson-Manigat.
- Ospemifene: This non-estrogen therapy works by boosting your vaginal wall thickness, which can reduce the severity of painful sex symptoms, adds Dr. Wilson-Manigat.
Talk to your partner
Sex is about pleasure and enjoyment for both of you, so if you’re experiencing pain or discomfort, share this with your partner. Worrying can actually make it worse, so communication is important. Finding ways to work around it together may help you to relax and unwind, making the whole thing more pleasurable. In some rarer cases, anticipating pain can lead to an involuntary tightening of your vagina known as vaginismus, which makes penetration even more difficult. Sex therapy, Kegel exercises (more on that below), and vaginal dilators may help you if you’re experiencing this.
Consider physical therapy for pelvic floor
Your pelvic floor is a group of muscles and ligaments that support your bladder, vagina, and bowel, and they can weaken with age. Pelvic floor exercises can help to prevent incontinence and vaginal prolapse. “Although it does seem to improve sexual dysfunction overall,” these exercises are unlikely to solve painful sex in its entirety, notes Dr. Wilson-Manigat. If you’re considering trying therapy for your pelvic floor, chat with your doctor first to make sure you avoid anything that could inadvertently make your sexual pain worse.
Rethink what counts as sex
Don’t stop having sex altogether — unless you want to. Regular stimulation increases blood flow that can boost your vaginal health. It can help to reframe your idea of partnered sex, too. Enjoyable sex doesn’t need to include penetration, so consider exploring alternative ways to enjoy intimacy with your partner, such as kissing, mutual masturbation, and oral sex.
Using sex toys together can also be a gentler way to enjoy sex. There are many styles of toys, so shop around until you find one that suits your needs. You could try clitoral-targeted sex toys that don’t require penetration to achieve satisfaction or experiment with different-shaped toys made from different materials that might feel gentler to touch.
Try sex therapy
Sex may be a physical act, but how you think and feel can have a huge impact on your sexual experiences. If it’s been worrying you, it could help to talk to someone. “Treatment by a mental health specialist or sex therapist can definitely help manage the anxiety and other emotional and mental roadblocks that may develop as a result of painful sex, particularly if it’s been going on for a long time,” says Dr. Wilson-Manigat.
When to speak to a doctor about painful intercourse
If you experience any type of pain during or after sex, make an appointment with your doctor. They will first try to figure out the cause of your discomfort and then recommend the best way to treat it. You might need to have some tests, like scans or a blood test, but these should help your doctor recommend specific treatments based on the likely cause of your pain.
“Once treatment begins, you can expect improvement within a few weeks,” says Dr. Wilson-Manigat. Estrogen therapy can start to take effect in four to six weeks, she explains, while other medical treatments including DHEA and ospemifene may take up to 12 weeks.
More FAQs
What is dyspareunia?
Dyspareunia is a medical term to describe lasting or recurrent pain in the genital area or within the pelvis that occurs before, during, or after sex. It has many possible causes including medical and emotional factors, but you’ll be glad to hear it can be treated.
Does eating estrogen-rich foods help with painful sex after menopause?
Research into the impact that estrogen-rich foods can have on sexual health is lacking. But eating a diet that’s high in phytoestrogens (plant-based sources of estrogen) has been found to potentially help with general menopause symptoms. Examples of these foods include whole grain cereals, flaxseed, chickpeas, and legumes. Reducing caffeine and alcohol intake is a good idea, too. It’s worth reiterating, however, that no direct link has currently been found between eating estrogen-rich foods and improving vaginal dryness or painful sex.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“About Vaginal Oestrogen.” NHS, www.nhs.uk/medicines/hormone-replacement-therapy-hrt/vaginal-oestrogen/about-vaginal-oestrogen/. Accessed 7 June 2024.
Alizadeh, Ameneh, and Farnaz Farnam. “Coping with Dyspareunia, the Importance of Inter and Intrapersonal Context on Women’s Sexual Distress: A Population-Based Study.” Reproductive Health, vol. 18, July 2021, https://doi.org/10.1186/s12978-021-01206-8.
Archer, David F., et al. “Ospemifene for the Treatment of Menopausal Vaginal Dryness, a Symptom of the Genitourinary Syndrome of Menopause.” Expert Review of Endocrinology and Metabolism, vol. 14, no. 5, Sep. 2019, pp. 301–14, https://doi.org/10.1080/17446651.2019.1657008.
Bleibel, Belal, and Hao Nguyen. “Vaginal Atrophy.” StatPearls, StatPearls Publishing, 3 July 2023, www.ncbi.nlm.nih.gov/books/NBK559297/.
Changes in Hormone Levels.” The North American Menopause Society, www.menopause.org/for-women/sexual-health-menopause-online/changes-at-midlife/changes-in-hormone-levels. Accessed 7 June 2024.
Chen, Junya, et al. “Evaluation of the Efficacy and Safety of Hyaluronic Acid Vaginal Gel to Ease Vaginal Dryness: A Multicenter, Randomized, Controlled, Open-Label, Parallel-Group, Clinical Trial.” The Journal of Sexual Medicine, vol. 10, no. 6, June 2013, pp. 1575–84, https://doi.org/10.1111/jsm.12125.
Constantine, G., et al. “Female Sexual Function Improved with Ospemifene in Postmenopausal Women with Vulvar and Vaginal Atrophy: Results of a Randomized, Placebo-Controlled Trial.” Climacteric, vol. 18, no. 2, Apr. 2015, pp. 226–32, https://doi.org/10.3109/13697137.2014.954996.
“Dyspareunia (Painful Intercourse).” Cleveland Clinic, my.clevelandclinic.org/health/diseases/12325-dyspareunia-painful-intercourse. Accessed 7 June 2024.
“Estrogen.” Cleveland Clinic, my.clevelandclinic.org/health/body/22353-estrogen. Accessed 7 June 2024.
Franco, Maíra M., et al. “Pelvic Floor Muscle Training Effect in Sexual Function in Postmenopausal Women: A Randomized Controlled Trial.” The Journal of Sexual Medicine, vol. 18, no. 7, July 2021, pp. 1236–44, https://doi.org/10.1016/j.jsxm.2021.05.005.
Kao, A., et al. “Dyspareunia in Postmenopausal Women: A Critical Review.” Pain Research and Management, vol. 13, no. 3, May–June 2008, pp. 243–54, https://doi.org/10.1155%2F2008%2F269571.
Krychman, Michael L. “Vaginal Estrogens for the Treatment of Dyspareunia.” The Journal of Sexual Medicine, vol. 8, no. 3, Mar. 2011, pp. 666–74, https://doi.org/10.1111/j.1743-6109.2010.02114.x.
Labrie, Fernand, et al. “Efficacy of Intravaginal Dehydroepiandrosterone (DHEA) on Moderate to Severe Dyspareunia and Vaginal Dryness, Symptoms of Vulvovaginal Atrophy, and of the Genitourinary Syndrome of Menopause.” Menopause, vol. 23, no. 3, Mar. 2016, pp. 243–56, https://doi.org/10.1097/gme.0000000000000571.
MenoNote: Vaginal Dryness. The North American Menopause Society, 2022, www.menopause.org/docs/default-source/for-women/mn-vaginal-dryness.pdf.
“Menopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401.
“Menopause.” World Health Organization, 17 Oct. 2022, www.who.int/news-room/fact-sheets/detail/menopause.
“Menopause 101: A Primer for the Perimenopausal.” The North American Menopause Society, www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal. Accessed 7 June 2024.
“Painful Intercourse (Dyspareunia).” Mayo Clinic, 16 Feb. 2024, www.mayoclinic.org/diseases-conditions/painful-intercourse/symptoms-causes/syc-20375967.
“Pain with Penetration.” The North American Menopause Society, www.menopause.org/for-women/sexual-health-menopause-online/sexual-problems-at-midlife/pain-with-penetration. Accessed 7 June 2024.
“Pelvic Floor Muscles.” Mayo Clinic, 25 Apr. 2020, www.mayoclinic.org/diseases-conditions/urinary-incontinence/multimedia/pelvic-floor-muscles/img-20007099.
“Perimenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21608-perimenopause. Accessed 7 June 2024.
“Perimenopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666.
“Postmenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21837-postmenopause. Accessed 7 June 2024.
Rosenblum, Nirit. “Update in Female Hormonal Therapy: What the Urologist Should Know: NYU Case of the Month, December 2020.” Reviews in Urology, vol. 22, no. 4, 2020, pp. 182–85.
“Sex Therapist.” Cleveland Clinic, my.clevelandclinic.org/health/articles/24524-sex-therapist. Accessed 7 June 2024.
Swenson, Carolyn W., et al. “Aging Effects on Pelvic Floor Support: A Pilot Study Comparing Young versus Older Nulliparous Women.” International Urogynecology Journal, vol. 31, no. 3, Mar. 2020, pp. 535–43, http://dx.doi.org/10.1007/s00192-019-04063-z.
Thielen, Jacqueline M. “Vaginal Moisturizers and Lubricants: What’s the Difference? Which Do I Buy?” Mayo Clinic, 27 Jan. 2022, mcpress.mayoclinic.org/women-health/vaginal-moisturizers-and-lubricants-whats-the-difference-which-do-i-buy/.
“Vaginal Atrophy.” Mayo Clinic, 17 Sep. 2021, www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288.
“Vaginismus.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/15723-vaginismus. Accessed 7 June 2024.
“When Sex Is Painful.” The American College of Obstetricians and Gynecologists, Apr. 2020, www.acog.org/womens-health/faqs/When-Sex-Is-Painful.
History of updates
Current version (14 June 2024)
Published (14 June 2024)
In this article
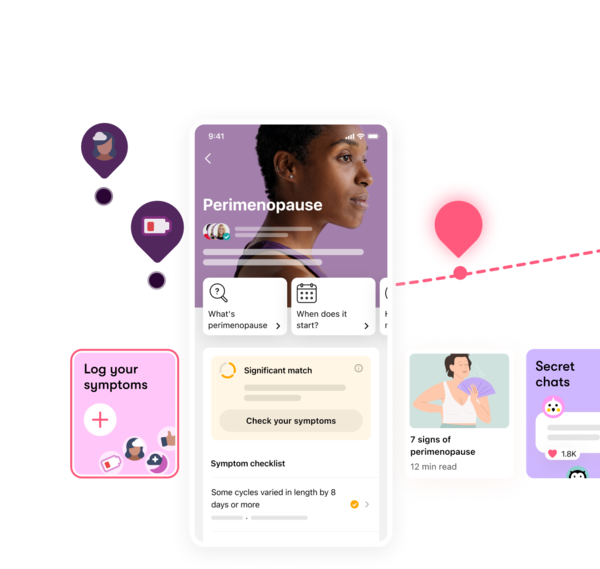
Track your perimenopause journey in the Flo app
-
Log symptoms and get tips to manage them
-
Learn what to expect with expert-led articles and videos
-
Connect with others who can relate to how you're feeling




