Ovulation tests promise to take the guesswork out of getting pregnant, but how accurate are they? A Flo expert explains everything you need to know.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Ovulation tests: How they work and when to take them


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
When you’re trying for a baby, the amount of advice and products promising to help you get pregnant can feel overwhelming. With fertility ads popping up all over your social media feeds and conception tips flying around your friendship circles, it can all start to feel very complicated.
Plus, you might find that getting pregnant isn’t quite as easy as your sex education classes implied. It might not happen right away, although 85% of couples who are trying to conceive will be pregnant after one year of trying. Been trying for 12 months or more? You might want to check in with your doctor to make sure that everything is OK (or after six months of trying if you’re over 35).
Among all of this noise, you may have heard of ovulation tests, which thankfully, are pretty straightforward. They’re designed to take the guesswork out of knowing when you’re most fertile and therefore most likely to get pregnant.
Intrigued? We’ve got the lowdown on how they work and when to take them, with advice from Flo expert Dr. Jennifer Boyle, obstetrician and gynecologist, Massachusetts General Hospital, Massachusetts, US.
And just remember, ovulation tests should never be used as a form of birth control. While they can be up to 99% accurate, they can also give false positive results, so it’s best to use another form of contraception if you want to avoid getting pregnant.
Key takeaways
- Ovulation tests work by detecting the amount of a hormone called luteinizing hormone (LH) in your pee.
- A surge in LH means that you are about to ovulate, usually in the next 36 hours.
- If you get a positive result, now is the time to have lots of sex if you’re trying to get pregnant.
- If you get a negative result, you should continue to take one or two tests each day, as you might ovulate slightly later than expected.
- Remember that ovulation tests should never be used as a form of birth control.
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
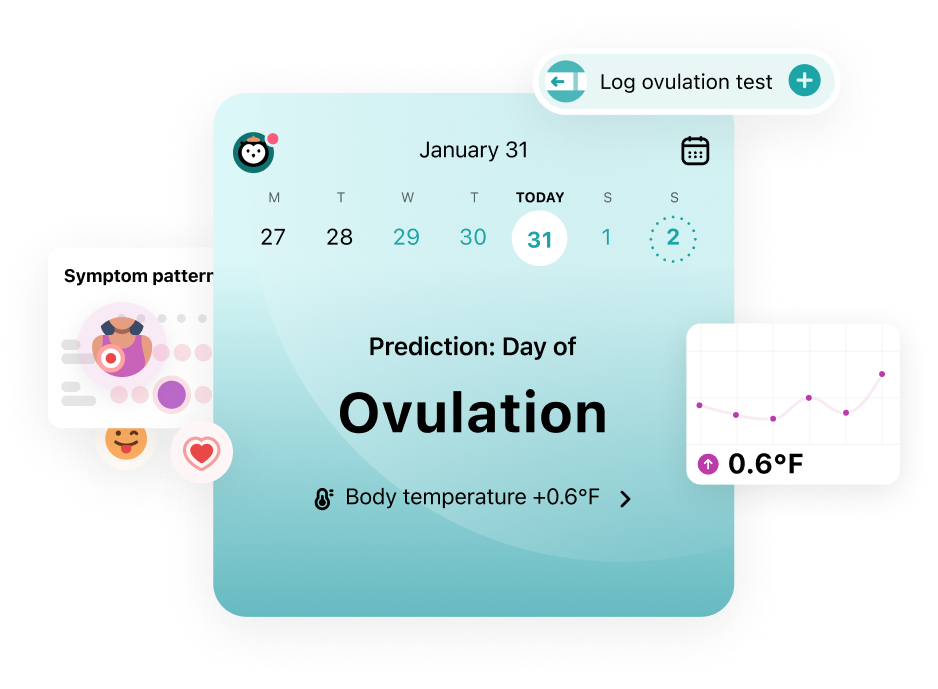
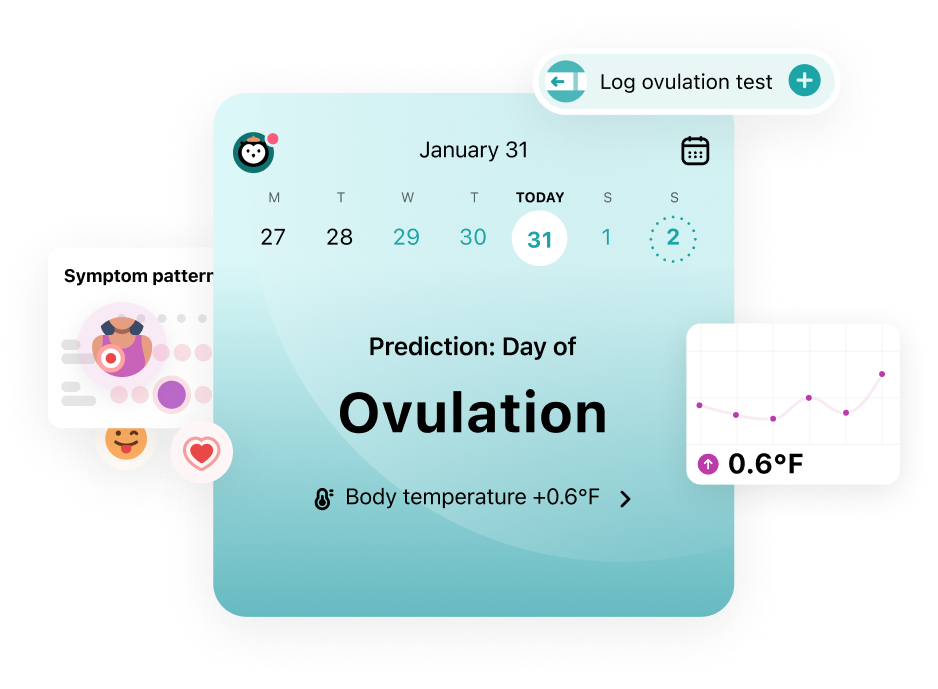
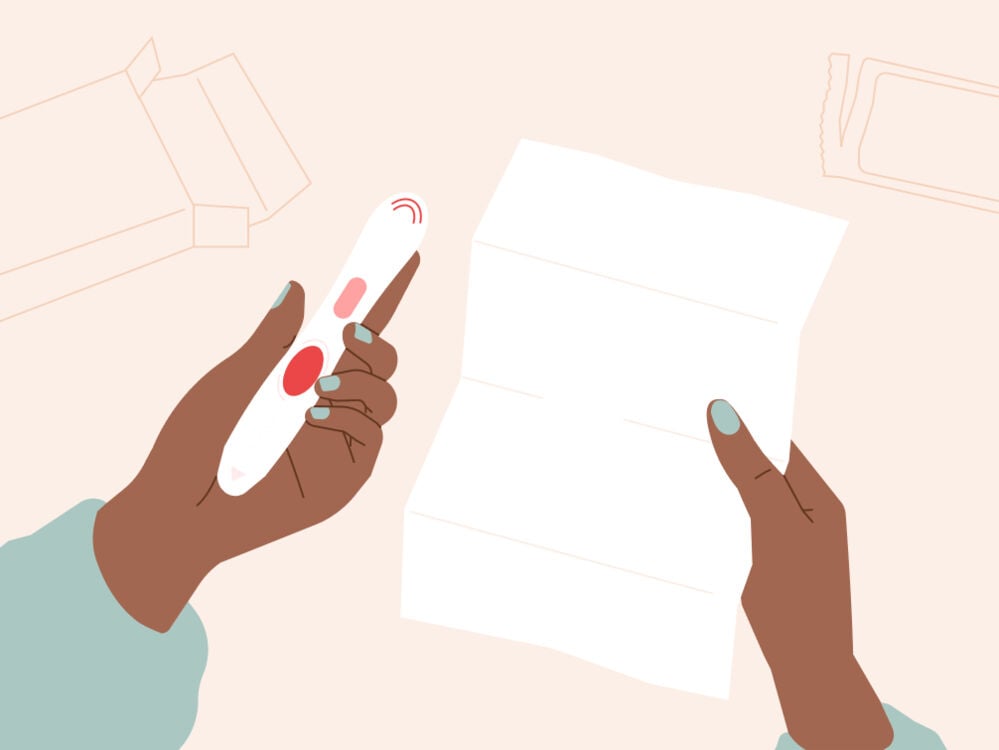
Understand your fertility better with the Flo app
- Learn more about your fertility signals
- Improve ovulation predictions by tracking temperature via Apple Watch
- Log your ovulation test results
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
Trying to conceive?
The Flo app can help you better understand your fertility
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
Understand your fertility better with the Flo app
- Learn more about your fertility signals
- Improve ovulation predictions by tracking temperature via Apple Watch
- Log your ovulation test results
Take a quiz
Find out what you can do with our Health Assistant
When do you ovulate?
Ovulation is when one of your ovaries releases an egg in the hope of it being fertilized by a sperm. This happens around halfway through your cycle. That means that if you have an average 28-day cycle, you’ll probably ovulate around day 14. Of course, tracking cycle lengths can vary, and anything between 21 and 35 days is considered normal.
Knowing when you’re ovulating can help you figure out when you’re most fertile and therefore most likely to get pregnant. Helpful, right? Generally, you’re most fertile from five days before ovulation to 24 hours after ovulation. This might sound like a long time, but it’s because sperm can live inside you for three to five days (yes, really!).
An egg can also live for 12 to 24 hours after it’s been released from your ovary. This whole period of time is known as your fertile window, and it’s your cue to have lots of sex to maximize your chances of getting pregnant.
Signs of ovulation
You might experience some telltale signs of when you’re ovulating each month that appear like clockwork around the middle of your cycle. However, we’re all different, and not everyone will get these, so don’t worry if you don’t.
Just so you know, some of the signs of ovulation to look out for include:
- Your cervical mucus will become slippery and wet, like egg whites.
- Your basal body temperature will rise slightly by around 0.5 to 1 F (0.22 to 0.56 C) (something you’ll notice if you’re keeping track of your basal body temperature to get pregnant.)
- Your cervix will move higher up inside your vaginal canal and become softer.
- You might experience bloating.
- You could have some light spotting.
- Your breasts might feel sore or tender.
- You could have some pelvic or abdominal pain.
- You might have a higher sex drive than usual.
- You might have some nausea.
If you do experience these signs, you could use them to track ovulation.
“Another great ovulation predictor test is just tracking your cycles and making sure you have sex one to two days before your usual ovulation day,” says Dr. Boyle. Don’t forget, you can track your periods in an app like Flo and get a personalized prediction of when you’re likely to ovulate.
Dr. Boyle continues, “I prefer these methods over the commercial tests, not only because they’re free, but because they help people to better understand and gain confidence in their bodies and trust their instincts. These skills will be incredibly helpful not just while trying for pregnancy, but during pregnancy itself, childbirth, breastfeeding, and in parenting in general.”
Of course, there’s absolutely nothing wrong with using ovulation tests to help you figure out when you’re ovulating, either. Which brings us to …
"Another great ovulation predictor test is just tracking your cycles and making sure you have sex one to two days before your usual ovulation day"
Ovulation sticks: How do ovulation tests work?
It’s totally understandable if you want the extra reassurance of using ovulation tests when you’re trying for a baby.
While they can be pricey, they’re pretty straightforward to use. They work by detecting luteinizing hormone (one of the key hormones released during the menstrual cycle) in your pee.
“LH levels surge 36 hours before the egg is released,” explains Dr. Boyle. “LH enters the urine about 12 hours after the surge. So a urinary LH predictor ovulation kit will be positive 24 hours before ovulation.”
How to take an ovulation test
It’s a bit like taking a pregnancy test: You just hold the stick in your stream of pee for however long the instructions tell you to. You could also collect your urine in a cup and dip the stick into it for the required amount of time if that’s easier.
“Since each brand of test is different, it’s important to follow the exact directions of the test you buy,” advises Dr. Boyle. “The more concentrated your urine is, the more likely it is that the test will pick up LH. If your urine is very diluted, it will be harder to pick up the LH. A lot of tests recommend holding your urine for at least four hours before doing the test.”
You might also be wondering about the best time to take an ovulation test. Experts recommend that you test every day from four days before your predicted ovulation day, or from day 10 of your cycle (if you have a 28-day cycle) if you’re not sure when you might ovulate.
Note: Ovulation predictions should never be used for birth control.
What kinds of ovulation tests are out there?
You’ll probably spot a few different kinds of ovulation tests at the drugstore, so choose the one that works best for you. For example, the tests might show the results in different ways, from darkening lines or words to smiley faces.
Do ovulation tests need to be done twice a day?
Your LH surge could be long (more than 24 hours) or short (less than 24 hours). With this in mind, it makes sense that you’d have a better chance of catching the peak if you took an ovulation test twice a day, especially if you have a short LH surge. However, you don’t have to test this often unless you want to.
When to start ovulation testing with irregular cycles
If you have irregular cycles, then you’re certainly not alone. Around 14% to 25% of women are estimated to have them. However, not knowing how long your cycle will be can make it tricky to know when to start using ovulation tests. To make sure you don’t miss the peak, Dr. Boyle recommends testing starting from four days before the moment when you’d ovulate in your shortest cycle to the day when you’d ovulate in your longest cycle.
“Some ovulation tests recommend that you start testing the day after your period ends if you have irregular cycles,” says Dr. Boyle. “This may result in you testing for many days, however. This can get annoying and costly. Sometimes I see patients who start testing early this way and then get sick of not seeing any change and give up. They stop testing before they are actually ovulating and can miss their fertile window.”
The bottom line is that choosing when and how often to use ovulation sticks is a personal choice, so trust your instincts and do what feels right for you. You know your body best, after all.
Are ovulation test results 100% accurate?
They’re not 100% accurate, but they’re pretty close. Research suggests that ovulation tests have an accuracy of 99%.
However, it’s important to know that false-positive ovulation test results can happen. “One study found that in 7% of cases, there was a false-positive test result,” says Dr. Boyle. “That means the test made it look like the person was going to ovulate, but when they evaluated the person a week or more later, they found that they hadn’t ovulated.”
A false-positive result could be due to a problem with the test, or you might not have gotten enough pee on the stick. If you think this might be the case, you could try taking another test and seeing if you get a different result. You can also try our ovulation calculator to get a quick prediction of when you’re likely to ovulate.
Ovulation test results: What to do next
Positive ovulation test
A positive result means you’re about to ovulate — usually within the next 24 hours. [9] This is a great time to have plenty of sex. And as your egg can live for 12 to 24 hours, it’s a good idea to have sex the next day too, if possible.
Negative ovulation test
If you get a negative result, don’t panic. This simply means that the test hasn’t picked up a surge in LH yet. In this case, the best thing to do is to test again. It’s a good idea to do this later in the same day, as if you have a short LH surge, you might have just missed it. Or you could wait until the next day, too.
But what should you do if you still don’t get a positive result? “If you have regular cycles, then this is likely a testing issue and not a problem with you,” assures Dr. Boyle. “Consider looking for ovulation in a different way [such as ovulation signs like wet, slippery cervical mucus] or just having sex based on your predicted fertile days. However, if you have irregular cycles or abnormal cycles, then you should see a doctor.”
This still isn’t necessarily a cause for concern. You could be having a longer cycle than normal, meaning you haven’t ovulated yet, or a shorter cycle, meaning you’ve missed the right time to test for ovulation. Either way, it’s good to get checked out by your health care provider to make sure that everything’s OK.
Remember: Ovulation predictions should never be used for birth control.
More FAQs
How long after a positive ovulation test are you fertile?
An ovulation test will be positive for 24 hours before ovulation, and your egg will then live for 12 to 24 hours after. Doing the math, that means you’ll be fertile for up to 48 hours after getting a positive ovulation test result.
Can I get pregnant two days after ovulation?
It’s unlikely that you can get pregnant two days after ovulation, as your egg only lives for 12 to 24 hours after being released.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Calculating Your Monthly Fertility Window.” Johns Hopkins Medicine, 10 Mar. 2022, www.hopkinsmedicine.org/health/wellness-and-prevention/calculating-your-monthly-fertility-window.
“Cervix.” Cleveland Clinic, my.clevelandclinic.org/health/body/23279-cervix. Accessed 9 Jan. 2024.
Charlewood, G. P. “Mittelschmerz or Ovulation Pain.” Suid-Afrikaanse Tydskrif Vir Geneeskunde [South African Medical Journal], vol. 32, no. 10, Mar. 1958, pp. 261–62.
“Fertility Awareness-Based Methods for Family Planning: A Literature Review.” Journal of Christian Nursing, vol. 37, no. 4, Oct./Dec. 2020, pp. E47–48, https://doi.org/10.1097/cnj.0000000000000758.
“How Long It Takes to Get Pregnant and How You Can Up Your Odds.” Cleveland Clinic, 27 Jan. 2023, health.clevelandclinic.org/how-long-does-it-take-to-get-pregnant.
McGovern, Peter G., et al. “Absence of Secretory Endometrium after False-Positive Home Urine Luteinizing Hormone Testing.” Fertility and Sterility, vol. 82, no. 5, Nov. 2004, pp. 1273–77, https://doi.org/10.1016/j.fertnstert.2004.03.070.
“Menstrual Cycle: What’s Normal, What’s Not.” Mayo Clinic, 22 Apr. 2023, www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/menstrual-cycle/art-20047186.
“Ovulation.” Cleveland Clinic, my.clevelandclinic.org/health/articles/23439-ovulation. Accessed 9 Jan. 2024.
“What Ovulation Signs Can I Look Out for If I’m Trying to Conceive?” Mayo Clinic, 7 Dec. 2022, www.mayoclinic.org/healthy-lifestyle/getting-pregnant/expert-answers/ovulation-signs/faq-20058000.
“Should You Use Ovulation Strips to Get Pregnant?” Cleveland Clinic, 13 May 2021, health.clevelandclinic.org/should-you-use-ovulation-strips-to-get-pregnant/.
Su, Hsiu-Wei, et al. “Detection of Ovulation, a Review of Currently Available Methods.” Bioengineering and Translational Medicine, vol. 2, no. 3, Sep. 2017, pp. 238–46, https://doi.org/10.1002%2Fbtm2.10058.
Ogle, Alicia. “Using Ovulation Tools to Predict Fertility.” Mayo Clinic Health System, 13 June 2023, www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/using-ovulation-kits-to-predict-fertility.
“What Are Menstrual Irregularities?” Eunice Kennedy Shriver National Institute of Child Health and Human Development, www.nichd.nih.gov/health/topics/menstruation/conditioninfo/irregularities. Accessed 9 Jan. 2024.
History of updates
Current version (09 January 2024)
Published (29 August 2018)
In this article
Get your personal guide to fertility
-
Learn how to read your body's ovulation signals
-
Find daily conception tips from our experts
-
Chat with others who are trying to get pregnant




