Think you have some signs of PCOS? A gynecologist talks us through the key PCOS symptoms and explains how it’s diagnosed so you can get the advice and support you need.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Signs of PCOS: How to know if you have polycystic ovary syndrome

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
Around one in ten women aged 15 to 49 is thought to have polycystic ovary syndrome (PCOS), but lots of us don’t know the symptoms beyond irregular periods. So how do you know if you’re experiencing the signs of PCOS, and what does a diagnosis involve? We break it down with a little help from Dr. Ruth Arumala, Obstetrician and gynecologist, Texas, US. Think of this as your very own PCOS symptoms checklist.
Do I have PCOS?
If you’re reading this article, there’s a good chance you might be wondering whether you have PCOS. If so, then you’re in the right place. We’re going to take a closer look at the different polycystic ovary syndrome symptoms and walk you through what to expect from a diagnosis.
Most common PCOS symptoms
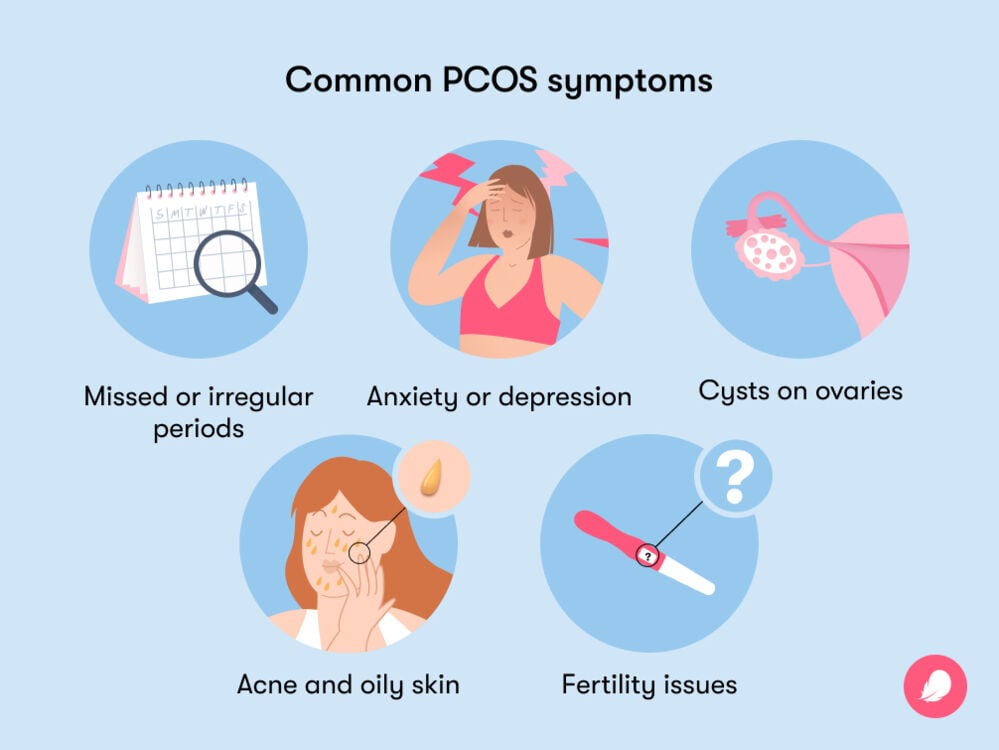
First of all, let’s make sure we all know what PCOS actually is. A common hormonal disorder, it can have three main signs or symptoms:
- Missed or irregular periods
- A high level of hormones called androgens (also known as “male” hormones)
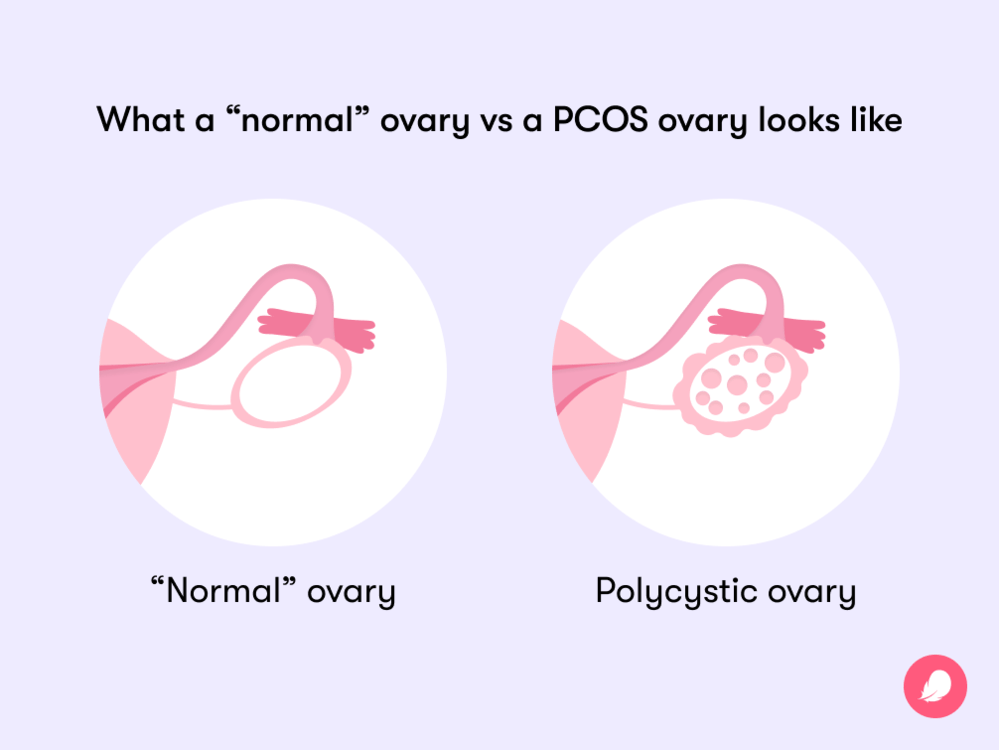
- Polycystic ovaries (when small egg sacs on the ovaries fill with fluid)
As we’ll explain in more detail, you don’t need to have all three of the symptoms to get a diagnosis. Instead, if you have two out of the three symptoms listed above and there’s no other clear explanation as to why you’re experiencing them, that’s when a doctor will typically diagnose PCOS.
You might be wondering what causes PCOS, but scientists don’t yet have a definitive answer to that question. However, they do believe you might be more likely to have PCOS if you are insulin resistant (which means your body can’t regulate blood sugar in the way it should), if you have a family history of it, or if you are overweight (which means you have a body mass index above 25).
PCOS symptoms checklist
As we now know, you’ll need to be displaying at least two of the three key symptoms of PCOS listed above in order to be diagnosed with the condition. But beyond that, there are several other indicators that you might have polycystic ovary syndrome. It’s always useful to be aware of the other signs and symptoms, so we run through them below. And remember, if you think you might have PCOS, reach out to your doctor so they can investigate.
Missed or irregular periods
We already know that missed or irregular periods are one of the most common signs of PCOS, but why? “In order to ovulate on a regular monthly basis, there is a precise [mix] of hormones that must occur,” explains Dr. Arumala. “The bottom line is that PCOS alters the ratio of hormones necessary for ovulation and [therefore disrupts] a regular menstrual cycle.”
This is because the high level of androgens, or “male” hormones, that are present in PCOS can mean that the ovaries stop releasing eggs regularly or might not release an egg at all. This can understandably have a secondary effect on your periods, meaning that they could become irregular or even stop for a while.
If you stop ovulating due to PCOS, you might also notice that you sometimes experience heavy bleeding. Our ovaries usually produce a balance of estrogen and progesterone, but if they stop ovulating, they’ll also stop producing progesterone. This could result in the uterus lining growing too much or becoming too thick, which can lead to occasional episodes of abnormal bleeding called “anovulatory abnormal uterine bleeding.” This bleeding is likely to be heavier and last longer than a normal period.
Excessive hair growth or hair thinning and hair loss
The high levels of androgens that often go hand in hand with PCOS could also have an impact on your hair growth. First, you might find that dark or coarse hair grows on your arms, chest, face, or abdomen. Dr. Arumala explains that this excessive hair growth is called hirsutism. It’s common in PCOS and thought to affect up to 70% of women who have the condition.
In contrast, you might also notice hair loss or thinning, which can be another upsetting sign of PCOS. “Androgens are the main regulators of hair follicles,” explains Dr. Arumala. “The response to androgens changes depending on what part of the body the follicle is housed in. They [can] cause small vellus hair [the soft hair that grows on most of your body] to change into larger terminal hairs [longer and darker hairs]. On the scalp, androgens can inhibit hair growth.”
Take a quiz
Find out what you can do with our Health Assistant
Acne and oily skin
Just when you thought that androgens couldn’t get any more troublesome, they can also cause your skin to become oily and produce spots. This acne is likely to be present on your face, back, or chest, and it might be harder to treat than normal acne. You can read more about how to treat PCOS skin issues here.
Insulin resistance, weight issues, and diabetes
Insulin resistance, weight issues, and diabetes are also linked to PCOS. In fact, they can even turn into a vicious cycle in terms of the impact they have on each other.
If you have insulin resistance, your body can’t use the insulin it produces in an effective way. This can lead to higher levels of androgens in your body, making insulin resistance one of the causes of PCOS; 65% to 70% of people with the disorder are affected by it.
Insulin resistance is, in turn, linked to weight gain because being overweight can be a cause of insulin resistance (although it’s worth noting that this isn’t always the case; not everyone with insulin resistance is overweight). “The more fat cells are present, the more androgens there are in the system,” adds Dr. Arumala.
Insulin resistance can also cause you to develop prediabetes or Type 2 diabetes (where your body no longer responds to insulin or its response is impaired, leading to high blood sugar levels). It’s estimated that over 50% of people with PCOS will develop Type 2 diabetes by the time they reach the age of 40.
The good news is that making healthy adjustments to your lifestyle, such as eating more healthily and moving more, could help to reverse insulin resistance and reduce your chances of developing PCOS. In people who have excess weight, “losing 5% of [their] body weight can reduce circulating active androgens,” explains Dr. Arumala. You can read more about a healthy PCOS diet here.
Polycystic ovaries
Surprisingly, despite the name, not everyone who develops PCOS actually has polycystic ovaries — confusing, right? Science is still puzzling this one out, with Dr. Arumala saying that medics are unsure why some PCOS patients have polycystic ovaries while others don’t. “PCOS is a complex, multifactorial disease with variable symptoms,” she adds.
So what exactly are polycystic ovaries? It’s important to note that they’re different from functional ovarian cysts, which are formed when a follicle in one of your ovaries swells to create a cyst. This can happen if the egg sitting in the follicle isn’t released during ovulation or if the fluid surrounding the egg doesn’t disappear after the egg is released. Typically, these types of cysts will usually shrink without any help within around 60 days, although they can sometimes remain swollen and create problems such as painful periods or pelvic pain.
On the other hand, the cysts developed due to PCOS are caused by a lack of ovulation. It’s comforting to note that these cysts are unlikely to be painful because they are tiny, at just around 2 to 9 mm each. “These cysts tend to form around the periphery of the ovaries, giving the ovaries a string-of-pearl-like appearance,” Dr. Arumala explains.
Fertility issues
The impact that PCOS can have on your menstrual period can have an effect on your fertility, too. If you’re trying to get pregnant with PCOS, but your periods become irregular or stop altogether, it can be understandably difficult to track your ovulation, meaning you might not be able to accurately time sex for conception.
PCOS can sometimes stop ovulation from occurring at all, making it one of the leading causes of infertility for women. It’s estimated that around 70% to 80% of women with PCOS might have difficulty conceiving. While this figure sounds scary, rest assured that there are a variety of treatment plans available (which you can read all about here).
You can also take comfort in the knowledge that with effective treatment, it’s believed that the majority of women with PCOS should be able to get pregnant.
Anxiety or depression
As well as talking about the physical signs of PCOS, it’s important to consider how PCOS makes you feel. There is a suspected link between PCOS and mental health, with some evidence showing an association between having PCOS and also having anxiety or depression. Scientists aren’t exactly sure why this is, but the good news is that there is plenty of help available.
If you’ve been affected by anxiety or depression, your health care professional should be able to help, whether by recommending some healthy adjustments to your lifestyle or through a treatment plan involving therapy or medications. You can also contact organizations such as the US-based Mental Health America or UK-based Mind for further support.
What to do if you think you have PCOS
If you’re experiencing any of the above PCOS symptoms or if you’re worried you might be experiencing other unusual symptoms of PCOS, Dr. Arumala has this advice: “Please see an OB-GYN.” They’ll be able to offer support and advice while running some tests if necessary.
If you do decide to take this step, you might be wondering what you can expect from an appointment. So let’s take a closer look at how PCOS is diagnosed and some of the PCOS tests that might be involved.
PCOS diagnosis
If you think you might have PCOS, please take some comfort in knowing you aren’t alone. The disorder is estimated to affect around one in ten women of reproductive age.
There is no single test available for PCOS; instead, you can expect a “diagnosis of exclusion,” says Dr. Arumala. “This means that all conditions and diseases that can cause similar signs and symptoms must be ruled out,” she explains.
Typically, most doctors use the following test for the diagnosis of PCOS: If patients have two out of the three main symptoms we looked at at the beginning of the article and they don’t have any other diagnosis that might explain them, they’re usually diagnosed with PCOS:
- Irregular or missed periods
- A high level of androgens or “male” hormones
- Polycystic ovaries
Unfortunately, this means that being diagnosed with PCOS could potentially take some time. There are no definitive timescales available, but one large global study found that while 43.4% of women were diagnosed within six months, a further 33.6% of women had to wait more than two years to receive a diagnosis. It can be frustrating to endure a long wait for a diagnosis — you’re not alone if you’ve felt that — but use the power you do have to keep pushing for tests from your health care provider if you feel like something’s not right.
If you’re wondering at what age symptoms of PCOS might start, keep in mind that they will usually begin in either your late teens or early twenties. Having said that, some cases may differ, so make sure you speak to a health care professional if you suspect you might have the condition.
“If you think you have PCOS, take comfort in knowing you aren’t alone.”
So what is likely to happen during a diagnosis? “A gynecologist will assess you, then conduct lab tests and [usually] an ultrasound,” says Dr. Arumala. During the initial assessment, you might be asked about your medical history — including information about your menstrual cycle — and checked for symptoms, including excessive hair growth or acne. Downloading an app like Flo can help you to keep all this information stored safely and privately in one place.
The lab tests conducted will be blood tests — although there is no definitive blood test for PCOS, there might be signs of PCOS in your blood work, such as raised androgen levels. You might then have an ultrasound to look for cysts on your ovaries or to check how thick the lining of your uterus is.
If the assessment, blood tests, and ultrasound show that you have two out of the three main symptoms listed above (with no other obvious explanation), then you are likely to be diagnosed with PCOS. This can understandably be upsetting news to hear, so if you’re in this position, be kind to yourself and remember to reach out to loved ones if you need support.
There is currently no cure for the condition, meaning it is something that’s lifelong, but be reassured that the symptoms can be managed with a wide range of PCOS treatment options. Your doctor will be able to discuss these with you when you’re ready to have that conversation.
What does PCOS feel like?
If you’ve recently been diagnosed with PCOS or you suspect you have signs of PCOS, it can help to hear about others’ experiences. Here’s what Flo users with PCOS have to say about how it feels to have the condition:
- “I’ve been struggling with PCOS for years until finally, I found [advice about managing] PCOS with a healthy diet and lifestyle. I thought this was worth a shot. Within a month, I got my period that had been missing for seven months, and my PCOS symptoms slowly started reducing.”
- “PCOS feels like being bullied by your body. Excess hair growth (EVERYWHERE), the constant fatigue, [and] the impact on my mental health have been interesting, to say the least. [It’s been] sad and difficult, but I’m praying for better days.”
- “I started taking birth control when I was a teenager, and it masked my symptoms. I didn’t get off it until several years later, [when] I began having symptoms of PCOS (weight gain, irregular periods, extreme mood swings, excess hair growth). I’m in my early twenties and just got officially diagnosed with PCOS. It feels good knowing I wasn’t totally crazy!”
- “I have PCOS, [but I’ve] never had weight problems, unwanted hair, hair thinning, acne, or any of the other symptoms besides the irregular periods.”
Signs of PCOS: The takeaway
There are a number of polycystic ovary syndrome symptoms to look out for, all of which can have an impact on both your physical and mental health. However, it’s worth keeping in mind that PCOS is diagnosed by exclusion, so experiencing one of the symptoms doesn’t necessarily mean that you have the disorder; you’ll need to have two out of the three main signs (irregular menstrual periods, excess androgen levels, and polycystic ovaries) to be formally diagnosed by a doctor.
It’s also worth remembering that PCOS affects around 5 million women in the United States alone and that there are a number of effective treatment options available. So while a diagnosis can be understandably scary, you are certainly not alone, and help will be available.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Abnormal Uterine Bleeding.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/15428-uterine-bleeding-abnormal-uterine-bleeding. Accessed 19 July 2022.
Arumala, Ruth. “PCOS Treatment: What Are Your Options?” Flo Health Inc., flo.health/menstrual-cycle/health/symptoms-and-diseases/pcos-treatment. Accessed 19 July 2022.
Azziz, Ricardo. “Controversy in Clinical Endocrinology: Diagnosis of Polycystic Ovarian Syndrome: The Rotterdam Criteria Are Premature.” The Journal of Clinical Endocrinology and Metabolism, vol. 91, no. 3, Mar. 2006, pp. 781–85.
Barber, Thomas M., et al. “Obesity and Polycystic Ovary Syndrome: Implications for Pathogenesis and Novel Management Strategies.” Clinical Medicine Insights: Reproductive Health, vol. 13, Sep. 2019, p. 1179558119874042.
Damone, Anna L., et al. “Depression, Anxiety and Perceived Stress in Women with and without PCOS: A Community-Based Study.” Psychological Medicine, vol. 49, no. 9, July 2019, pp. 1510–20.
“Does PCOS Affect Pregnancy?” National Institutes of Health, www.nichd.nih.gov/health/topics/pcos/more_information/FAQs/pregnancy. Accessed 19 July 2022.
Gibson-Helm, Melanie, et al. “Delayed Diagnosis and a Lack of Information Associated With Dissatisfaction in Women With Polycystic Ovary Syndrome.” The Journal of Clinical Endocrinology and Metabolism, vol. 102, no. 2, Feb. 2017, pp. 604–12.
“How Big Is an Ovary? 6 Causes of Enlarged Ovaries.” Flo Health Inc., flo.health/menstrual-cycle/health/symptoms-and-diseases/6-causes-of-enlarged-ovaries. Accessed 19 July 2022.
Ilyich, Iryna. “When to Take Ovulation Tests: Reasons for Positive and Negative Results.” Flo Health Inc., flo.health/getting-pregnant/trying-to-conceive/tracking-ovulation/ovulation-tests. Accessed 19 July 2022.
“Insulin Resistance and Diabetes.” Centers for Disease Control and Prevention, 11 Aug. 2021, www.cdc.gov/diabetes/basics/insulin-resistance.html.
Marshall, John C., and Andrea Dunaif. “Should All Women with PCOS Be Treated for Insulin Resistance?” Fertility and Sterility, vol. 97, no. 1, Jan. 2012, pp. 18–22.
McCartney, Christopher R., and John C. Marshall. “Clinical Practice. Polycystic Ovary Syndrome.” The New England Journal of Medicine, vol. 375, no. 1, July 2016, pp. 54–64.
Melo, Anderson Sanches, et al. “Treatment of Infertility in Women with Polycystic Ovary Syndrome: Approach to Clinical Practice.” Clinics, vol. 70, no. 11, Nov. 2015, pp. 765–69.
“Ovarian Cysts.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/9133-ovarian-cysts. Accessed 19 July 2022.
“PCOS (Polycystic Ovary Syndrome) and Diabetes.” Centers for Disease Control and Prevention, 28 Sep. 2021, www.cdc.gov/diabetes/basics/pcos.html.
“Polycystic Ovarian Syndrome (PCOS): What Is It, Causes, Symptoms & Treatment.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/8316-polycystic-ovary-syndrome-pcos. Accessed 19 July 2022.
“Polycystic Ovary Syndrome.” NHS, www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/. Accessed 19 July 2022.
“Polycystic Ovary Syndrome (PCOS).” The American College of Obstetricians and Gynecologists. www.acog.org/womens-health/faqs/polycystic-ovary-syndrome-pcos. Accessed 19 July 2022.
“Polycystic Ovary Syndrome (PCOS).” Mayo Clinic, 3 Oct. 2020, www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439.
Witchel, Selma Feldman, et al. “Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment with Emphasis on Adolescent Girls.” Journal of the Endocrine Society, vol. 3, no. 8, Aug. 2019, pp. 1545–73.




